Across the country, the lights are warming up for college game night. One freshman is getting his first starting spot as kick-returner. Looking over the crowded stadium, he sees his picture on the jumbotron. Everything blurs until the referee’s whistle signals kickoff and snaps him back into focus. He looks up and finds the ball spinning down towards him. He fields the ball a yard deep in his own end zone and sees a hole in the defensive coverage… One-hundred big ones to make the score six-zero with only ten seconds off the game clock!
As he darts left, intending to use the sideline as a straight shot to the end zone, he sees a defensive player coming out of the corner of his eye. The defensive back goes low, taking out his legs. On his way down to the turf, he sees the flash of a jersey and then a great burst of light as the world gets sucked into black. Our player lays facedown on the field, motionless. The medical team rushes to his aid after witnessing a tackle that seemed to more closely resemble a car accident…
* * *
Concussions happen so frequently in sports that we often consider them to be part of the price of participating. But their prevalence should not undermine the fact that they are a traumatic brain injury (TBI). The immediate deceleration that occurred when our player was hit caused the brain to rattle and collide repeatedly with the skull. This type of whiplash hit with such significant force that it majorly impacted the brain, despite the player wearing a well-fitted helmet. As the medical team tends to our concussed player, let’s explore what’s going on in his brain.
At the microscopic level, when his brain sustained an injury of that force, the biological effect of the damage starts with temporary loss of ability to regulate neuron potential [1]. Upon head impact, the player’s neuronal cell membranes are stretched, resulting in a neurochemical cascade that disrupts the chemical balance in the surrounding cell environment. At the center of the chaos, a burst of neurotransmitters is released, causing the player’s brain cells to immediately depolarize, affecting the sodium/potassium ion equilibrium between the interior and exterior environments of the cell. This is a big problem, as cell receptors cannot properly respond to stimuli and neurons cannot communicate when the cell is not at resting membrane potential. As an example, consider trying to make a phone call to 911 in the event of an emergency, but the lines are down. A critical message cannot be transmitted and acted on. Similarly, the environmental imbalance prevents the the cell from responding to signals propagated down axons. Now, the sodium/potassium ion pumps across the membrane are required to work harder to return the cell to a healthy membrane potential. While trying to return to its correct ionic potential, many free radicals are produced inside the cell. Free radicals are unstable atoms that roam around for another electron to make a stable pair, like a magnet looking for a piece of metal. However, in the process, they often cause damage to proteins, cell membranes, and DNA, the building blocks of bodily functions we often take for granted. If the impact directly affected the player’s temporal lobe, he may experience disturbances in normal visual and auditory perception and language comprehension when he awakens [1].
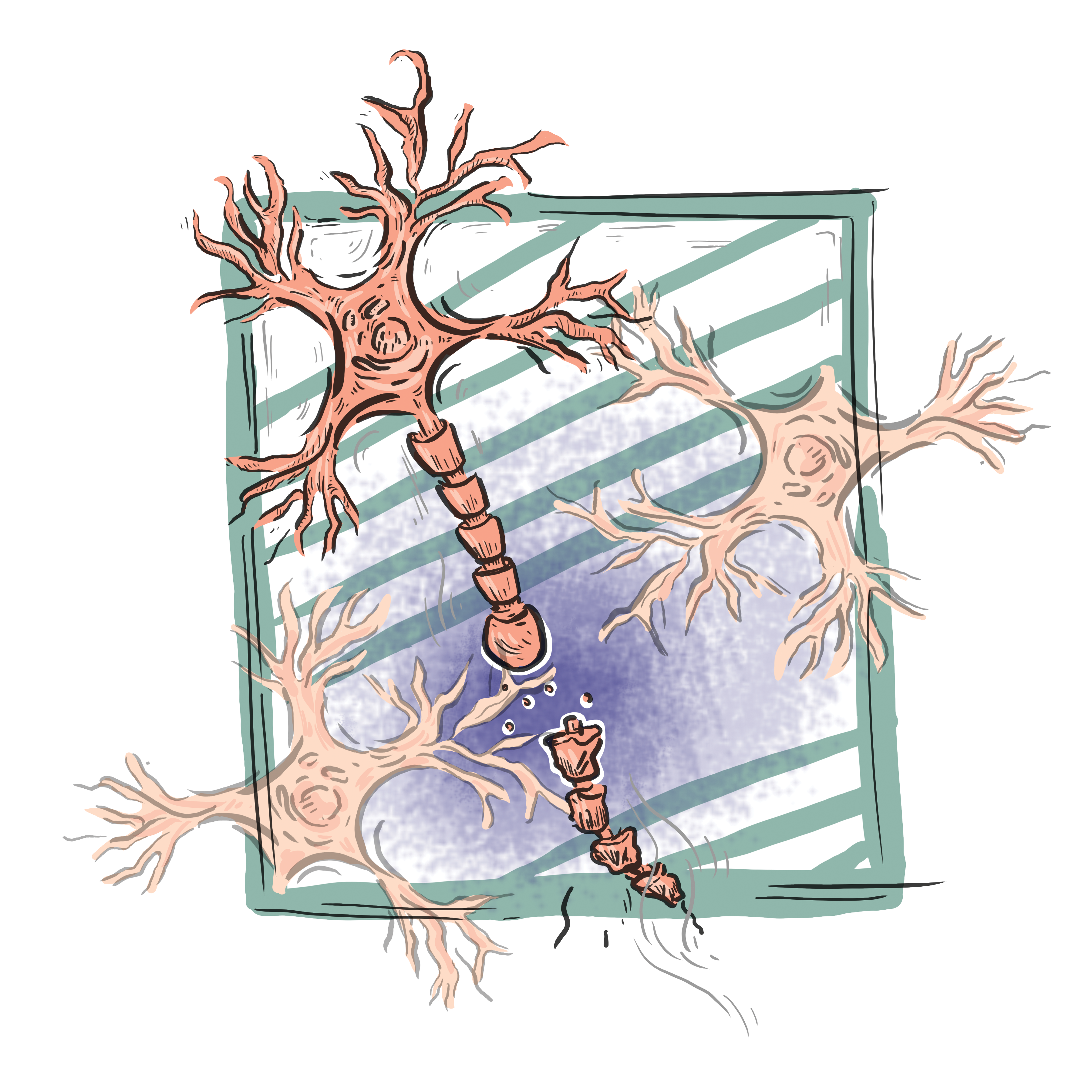
Simultaneously, the whiplash results in structural damage to the player’s neurons [1]. Unlike typical cells, neurons are made up of axons, long tubes along which signals propagate to the next neuron. They are structurally sound due to bundles of hundreds of microtubules that make up its skeleton. But the force from the incident easily broke these thin 25 nm tubes of protein, causing portions of the axons to swell. This disrupts communication between his neurons down axons and can lead to the eventual disconnection of neurons. If the axonal impact is widespread across the brain, our player’s behavior and physical abilities may be seriously affected for an extended period of time [1].
* * *
Let’s return to our player as he staggers to his feet and walks off the field with assistance from the medical team. If you look closely you can see his face slightly scrunched, wincing in pain. Resting now will allow neuroregeneration its due time to recover from the damage incurred. In a couple of months, he should be fine to play again provided he does not suffer from additional blows to the head [11]. In the case that a concussion can be inferred from the force of impact and aftermath, like our player being knocked unconscious, players are sidelined for the duration of the game. But a recent review of the current concussion management practices in the NFL (National Football League) from 1996-2001 revealed that 50% of players returned to play during the game after suffering a concussion [9]. Thankfully, this figure does not include our athlete. However, it is vital for players, coaches, NFL officials, and researchers (all stakeholders) to remember the effects associated with concussions, like ringing and nausea, often do not affect players immediately and this, coupled with the excitement and pressure to keep playing, leaves athletes with undetected injuries on the field at a severe risk, especially if another injury is sustained [3].
In fact, it is thought that repeated concussive or even subconcussive hits can lead to the onset of chronic traumatic encephalopathy (CTE). CTE is a tauopathy, a class of neurodegenerative diseases, along with Alzheimer’s disease and Parkinson’s disease, associated with tau protein. The robust axon structure of neurons is maintained by bundles of microtubules that are stabilized by these tau proteins. As noted with concussions, microtubules become damaged from head trauma. However, after suffering repeated hits to the head, the frayed microtubules release tau that then begins to clump together. Research shows that axonal injury causes phosphorylation, accumulation, and misfolding of tau proteins, which results in the formation of tangles in the brain [3]. For those who suffer from CTE, these tangles are found throughout the medial temporal lobe, which includes the hippocampus and controls conscious memory. Evidence also shows that tau has a toxic gain-of-function that gives it the ability to spread to other regions of the brain, causing more clumping even after the injury has stopped. Over time, the continued accumulation of tau leads to blocked and broken neural connections and overall neurodegeneration [3].
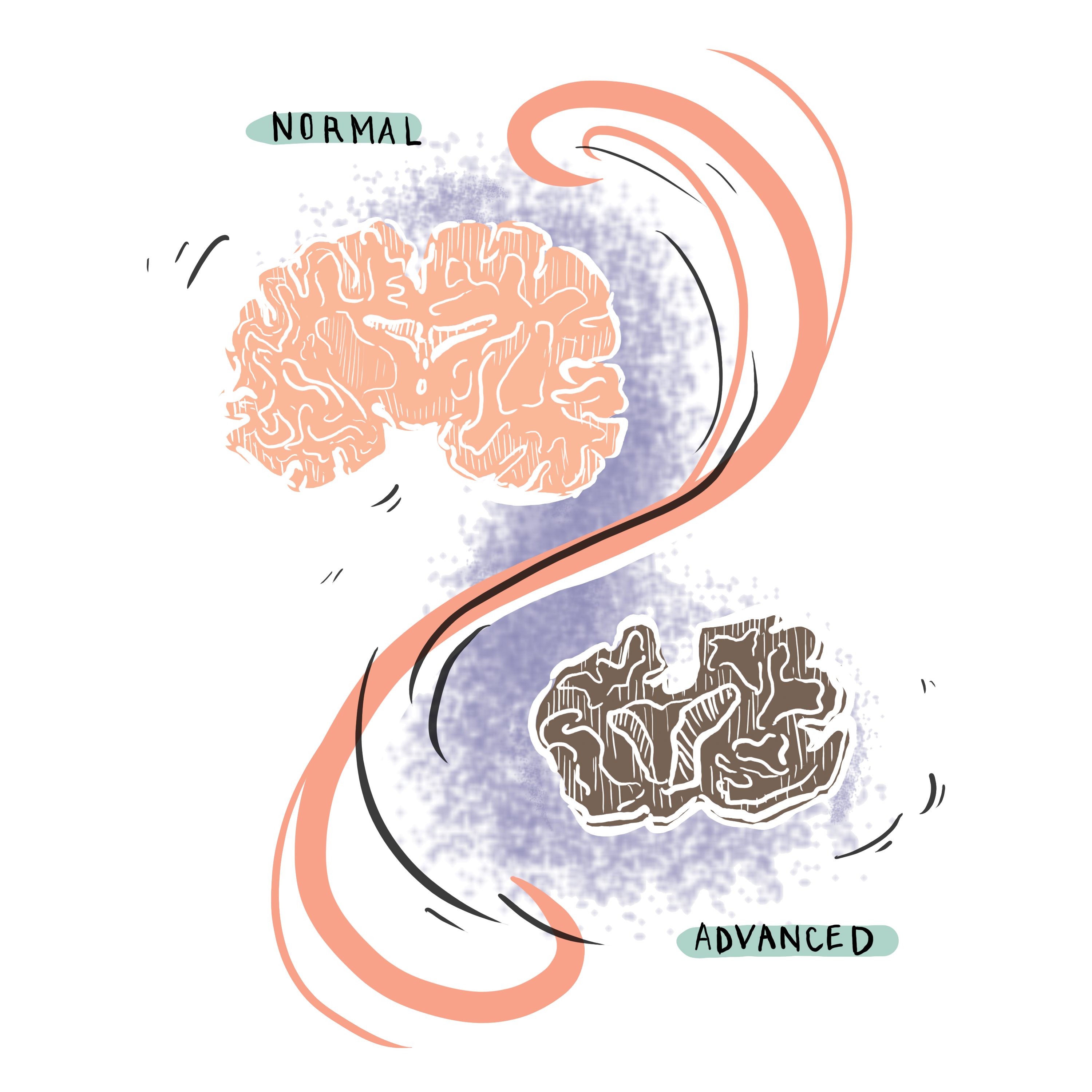
The tricky aspect of diagnosing CTE is that symptoms may not present themselves until later stages in life so they look awfully similar to other tauopathies, like Alzheimer’s disease. Recorded symptoms of CTE have been divided into affective disorders and cognitive changes. In a review from 2015 of all known CTE cases, researchers pinpointed symptoms as mild as headaches and concentration loss to symptoms as severe as language difficulties, motor impairments, and suicidality [4]. Though standards have been made to diagnose other neurodegenerative diseases by clinically evaluating the individual and using imaging to rule out other options, it is not the same case for CTE. Symptoms are different for each individual and many football players who have been diagnosed post-mortem for CTE were asymptomatic. Axonal integrity including areas of swelling, bleeding, and lesions in the brain can be examined using established Diffusion Tensor Imaging (DTI), but the indicative tau protein buildup in those who have CTE cannot be detected through Magnetic Resonance Imaging (MRI) nor through biomarker techniques [6]. The only definitive evidence clinicians have to diagnose CTE is with a brain tissue sample taken upon autopsy that exhibits irregular tau patterns. Part of the lack of diagnosis has to do with the lack of documentation of CTE compared to other neurodegenerative diseases. In the past 60 years, only 153 cases of CTE have been documented, 63 of which were from NFL players. However, many of the victims were also diagnosed with Alzheimer’s disease, Parkinson’s disease, or Lewy body dementia, making it difficult to establish definitive causation and risk [10]. To complicate the facts even more, the definitive cause of CTE is still unknown—it may be caused by few severe head injuries, many subconcussive injuries, or other types of head trauma [3]. But the answer to this seemingly straightforward question can have a widespread impact beyond professional football, as subconcussive injuries are common at all sports levels. A comparison of head impact frequency across different levels of play showed that high school football players on average experienced 565 head impacts per season and college players 1000 impacts, showing that even athletes who do not play at the professional level may still be at risk for getting CTE [11].
However, the lack of research mentioned above is certainly changing within the next decade. CTE has made several appearances in the media recently, most notably with the homicide of Odin Lloyd and subsequent suicide by Aaron Hernandez of the New England Patriots in 2017 and the release of the film Concussion about CTE in NFL Hall of Fame player Mike Webster. These events have pushed different stakeholders in society to pay attention to this insidious disease.
At the research level, the National Institute of Biomedical Imaging and Bioengineering along with the National Institute of Neurological Disorders and Stroke recently came to a consensus on the definition of CTE as the accumulation of phosphorylated tau proteins in neurons in an irregular pattern. This scientific acknowledgement of CTE’s existence represents a major step towards paving the way to future clinical investigations and imaging innovations. Researchers are currently working on using non-invasive tau imaging to learn more about tau aggregation to open the field to investigating causes, diagnosis, and prevention of CTE [7]. Dr. Richard Stern, Director of Clinical Research at Boston University’s Center for the Study of Traumatic Encephalopathy (CSTE), the largest CTE research group, expects a viable test to be developed within the decade.
At the sporting level, the National Football League Players Association announced its new collaboration in 2009 with the CSTE to further their ongoing CTE clinical research. The NFL is also slowly making rule changes to limit head injuries, like expanding the rule against contacting defenseless receivers to apply to all players and immediately whistling a ball dead if a ball carrier’s helmet is knocked off [8]. But football, of course, is a game of forward motion. Finding a balance between safety and maintaining the essence of the sport will be difficult, but is critical to reduce instances of CTE in our athletes down the line. As research is ongoing for CTE-specific measures, one attainable fix we can start with is proper concussion management. There is currently no consensus on return-to-play guidelines for professional or recreational sports. Past research has shown abnormalities in brain scans 2-4 weeks after the traumatic brain injury, suggesting that safe return-to-play guidelines should be 4-6 weeks after a concussive hit to allow the brain time for complete recovery [6]. Unfortunately, as explored above, these timeframes often are not strictly enforced leaving many players at risk to develop a currently incurable disease.
For now, the coaches make a good decision and our player will not return to the game. We can only hope that similar cautions continue to be taken for all players. With heavy implications of CTE stemming from concussive and subconcussive hits, we should at the very least ensure athletes that suffer concussions are removed from the game and are given a resting period, while working to implement more rigorous concussion protocols. It is our job as scientists, coaches, parents, and friends to understand the severe implications of concussions and respond to them as such. If we put our heads together, we can shift the view of CTE from an inevitable consequence to an avoidable risk.
References
- “2 Neuroscience, Biomechanics, and Risks of Concussion in the Developing Brain.” Institute of Medicine and National Research Council. 2014. Sports-Related Concussions in Youth: Improving the Science, Changing the Culture . Washington, DC: The National Academies Press. doi: 10.17226/18377.
- Molnar, Charles, and Jane Gair. “16.1 Neurons and Glial Cells.” Concepts of Biology- 1st Canadian Edition , Rice University, 2013.
- Gavett, B. E., Stern, R. A., & Mckee, A. C. (2011). Chronic Traumatic Encephalopathy: A Potential Late Effect of Sport-Related Concussive and Subconcussive Head Trauma. Clin Sports Med , 30 , 179–188. https://doi.org/10.1016/j.csm.2010.09.007
- Maroon JC, Winkelman R, Bost J, Amos A, Mathyssek C, et al. (2015) Chronic Traumatic Encephalopathy in Contact Sports: A Systematic Review of All Reported Pathological Cases. PLOS ONE 10(2): e0117338. https://doi.org/10.1371/journal.pone.0117338
- McKee, A.C., Cairns, N.J., Dickson, D.W. et al. Acta Neuropathol (2016) 131: 75. https://doi.org/10.1007/s00401-015-1515-z
- Ann C. McKee, Robert C. Cantu, Christopher J. Nowinski, E. Tessa Hedley-Whyte, Brandon E. Gavett, Andrew E. Budson, Veronica E. Santini, Hyo-Soon Lee, Caroline A. Kubilus, Robert A. Stern, Chronic Traumatic Encephalopathy in Athletes: Progressive Tauopathy After Repetitive Head Injury, Journal of Neuropathology & Experimental Neurology , Volume 68, Issue 7, July 2009, Pages 709–735, https://doi.org/10.1097/NEN.0b013e3181a9d503
- Tau imaging: V.L. Villemagne, N. Okamura, Tau imaging in the study of ageing, Alzheimer’s disease, and other neurodegenerative conditions. Curr Opin Neurobiol, 36 (2016), pp. 43-51
- Person. “Goodell Issues Memo Changing Return-to-Play Rules for Concussions.” NFL.com , National Football League, 26 July 2012, www.nfl.com/news/story/09000d5d814a9ecd/article/goodell-issues-memo-changing-returntoplay-rules-for-concussions .
- Marchi N, Bazarian JJ, Puvenna V, Janigro M, Ghosh C, et al. (2013) Consequences of Repeated Blood-Brain Barrier Disruption in Football Players. PLOS ONE 8(3): e56805. https://doi.org/10.1371/journal.pone.0056805
- Maroon JC, Winkelman R, Bost J, Amos A, Mathyssek C, et al. (2015) Chronic Traumatic Encephalopathy in Contact Sports: A Systematic Review of All Reported Pathological Cases. PLOS ONE 10(2): e0117338. https://doi.org/10.1371/journal.pone.0117338
- Cobb, B.R., Urban, J.E., Davenport, E.M. et al. Ann Biomed Eng (2013) 41: 2463. https://doi.org/10.1007/s10439-013-0867-6