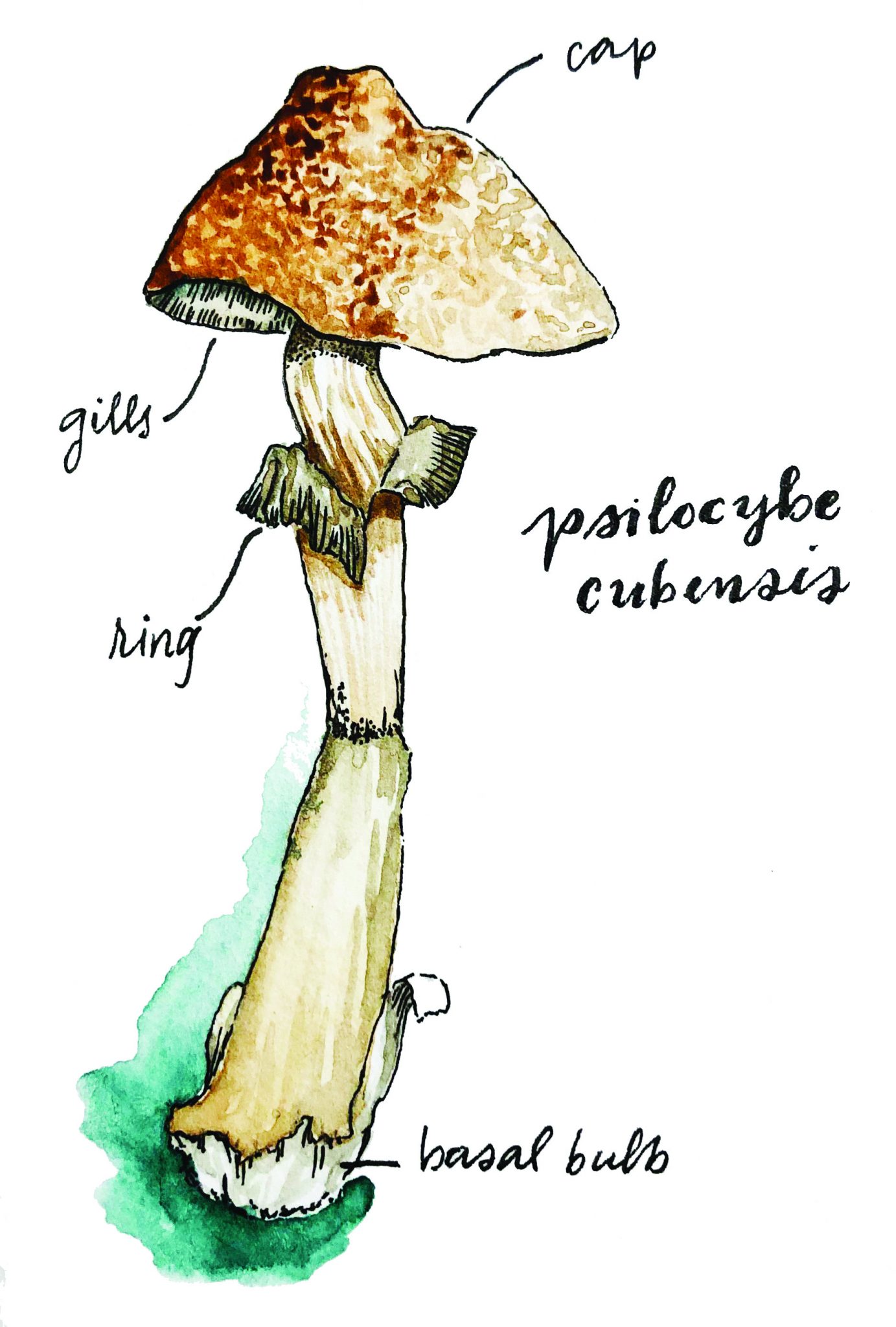
Psychedelics face an overwhelming stigma in Western culture that has limited scientific investigation into their uses since the 1960s. This came as a result of a lack of knowledge that contributed to their widespread misuse during that era. However, certain psychedelics could resurface in coming years as a treatment for psychiatric disorders that affect millions worldwide [1]. Scientists at research institutions such as Johns Hopkins University, the Imperial College London, and New York University have been steadily producing research confirming that the prodrug psilocybin, found in mushrooms of the psilocybe genus (commonly known as ‘magic mushrooms’), could be an effective treatment for disorders like depression, anxiety, and obsessive-compulsive disorder [2][3][4]. However, in order to understand how this new discovery could reshape the psychiatric landscape, it is first crucial to understand what psilocybin—and its metabolite, psilocin—is and how it interacts with the human body.
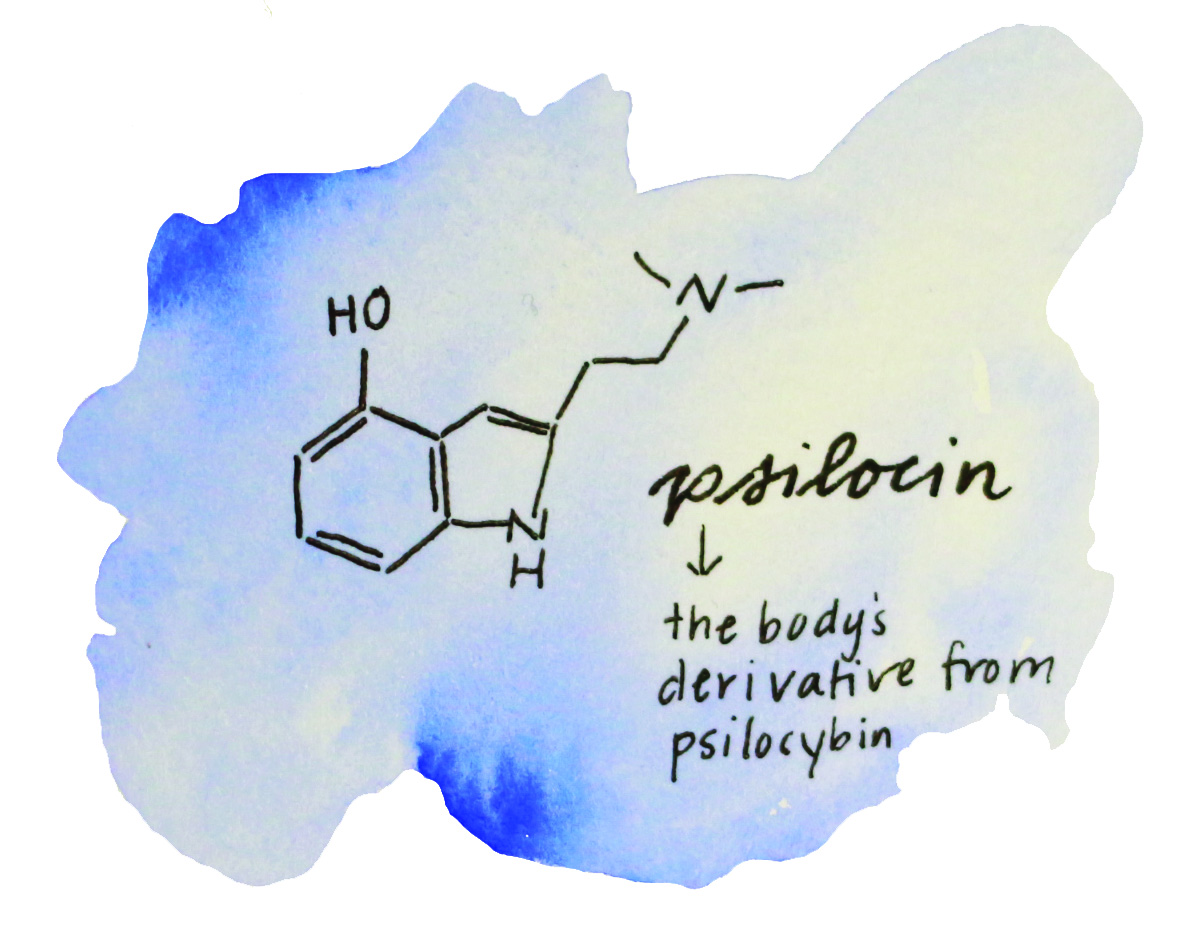
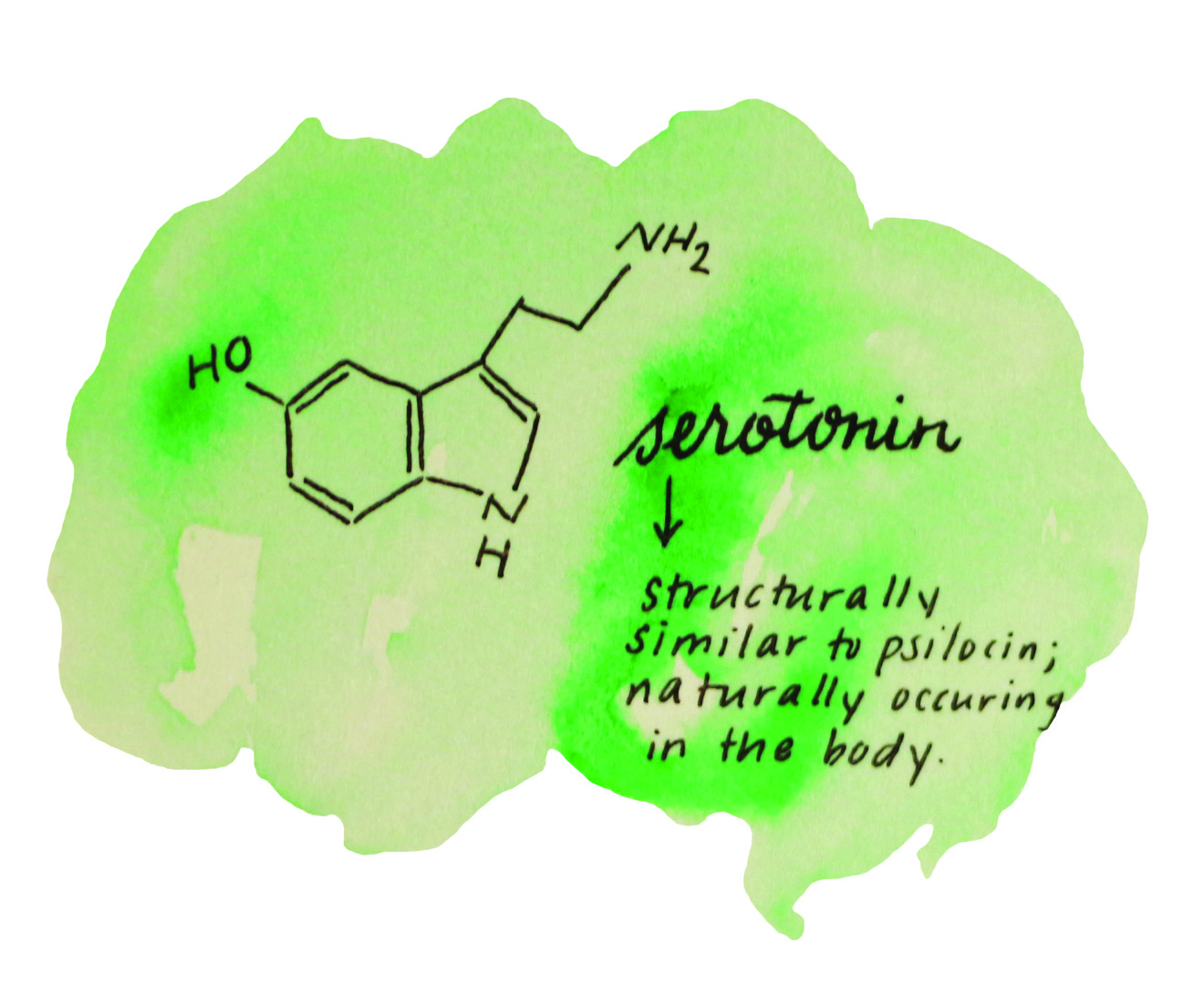
Psilocybin is a prodrug, a biologically inactive compound that can be metabolized by the body to produce a drug [5]. As a prodrug, psilocybin is unable to produce the effects typically associated with the ingestion of psilocybe mushrooms; however, it enables the body to produce the metabolite and psychoactive drug that does. After being ingested, molecules present in the intestinal mucus remove part of the psilocybin molecule known as the phosphoric ester group. This process transforms psilocybin into a new molecule: psilocin [5]. Psilocin is a psychoactive drug with a structure very similar to the mood-regulating neurotransmitter serotonin [5]. The newly formed compound, after traveling via the bloodstream to the brain, then acts primarily as an agonist to serotonin receptors due to its similar structure. This means that it elicits a physiological response from serotonin receptors just as serotonin would. It is hypothesized that the interaction between the psilocin and the serotonin receptors is what causes the patient to experience effects such as auditory and visual hallucinations as well as feelings of euphoria and greater connectedness to nature [6].
One of the most recent studies exploring the potentially beneficial effects of psilocybin mushrooms began in 2017 in England. A team of researchers at the Imperial College London sought to evaluate the effectiveness of psilocybin in remedying treatment-resistant depression (TRD) [2]. TRD is a form of depression in which patients are unresponsive to antidepressant medication, leaving them with little or no solution to their condition [7]. It affects approximately 10-30% of individuals with depression, meaning roughly four million people experience TRD worldwide [7][8]. The study was performed in a controlled setting where the patient-volunteers were guided through their experience by trained therapists [2]. In the trial, the scientists administered two doses of psilocybin, one 10 mg dose followed by a 25 mg dose one week later, to a group of 19 patient-volunteers affected by TRD, recording data pre- and post-treatment [2].
The researchers used two tools to record their data: a self-reported test, which measured a patient’s level of depression via a sequence of questions, and functional magnetic resonance imaging (fMRI) [2]. One week after the treatment occurred, the scientists observed that there was an overall decrease in the levels of depression in all 19 patients, as measured by the self-reported test. Furthermore, 47% of the patients maintained the reduction in their reported levels of depression for up to five weeks after the treatment. Even more interesting were the changes in brain activity recorded by the fMRI, which showed reduced blood flow to areas of the brain typically overactive in people suffering from depression, such as the amygdala—the region of the brain that, among other things, is involved in emotional response. These findings point to a possible explanation as to why the patients who received the treatment reported a decrease in their depressive symptoms [2]. A depressed person’s emotional response differs significantly from that of a non-depressed person: their responses to negative stimuli are extreme, while their responses to positive stimuli are negligible [9]. This characteristic, coupled with the reduction in blood flow to the amygdala, could provide some insight into why the depressed patients improved post-treatment [2]. The decrease in blood flow could point to decreased activity of the amygdala, which would mean that the depressed person’s emotional response to negative stimuli (and to stimuli in general) would be less extreme and more similar to the emotional response of a non-depressed person. It is important to note, however, that a change in blood flow is not a clear indication of a change in brain activity, so further research into this possible mechanism is necessary [2].
Scientists performing similar studies at New York University, the University of New Mexico, and Johns Hopkins University also corroborate these findings. For example, a study at New York University found that patient-volunteers suffering from cancer-related anxiety and depression showed a similar decrease in depressive symptoms following psilocybin treatment [3]. The researchers in the study administered a single dose of psilocybin (0.3 mg per kg of body weight) and a dose of niacin (250 mg), a form of vitamin B used as an active control, to patients who were randomly assigned two different session sequences: psilocybin first and niacin seven weeks later, or niacin first and psilocybin seven weeks later. 29 patients suffering from the aforementioned symptoms received the treatment in conjunction with psychotherapy. Patient-volunteers’ depression and anxiety levels were measured by self-reporting tests like the Hospital Anxiety and Depression Scale (HADS). Data of their mystical experiences were recorded using the Mystical Experience Questionnaire (MEQ30), which the patient-volunteers answered throughout the duration of the trial [3][10].
The results of the study were astounding: both groups showed a rapid decrease in depressive symptoms following the psilocybin treatment, as reported using the HADS test one day after the psilocybin doses [3]. Furthermore, both groups showed a persistent decrease in depressive symptoms up to six months following their first dose. The patient-volunteers also reported better attitudes toward death in the face of their illness and increases in their quality of life. The scientists hypothesized that one reason for the improvement in patients was the activation of serotonin receptors in the brain by psilocin; however, further research to find the exact mechanism must be done [3].
Another study at the University of Arizona investigated the efficacy of psilocybin in treating obsessive-compulsive disorder. Nine patient-volunteers were given four single-dose exposures to psilocybin, ranging from very low (25 micrograms/kg) to high (300 micrograms/kg) [4]. The sessions were separated by at least one week with each session lasting eight hours, after which patients were transferred to an inpatient unit for overnight observation. Patients described their experiences using self-reporting tests such as the Hallucinogen Rating Scale (HRS)–which measures an individual’s hallucinogenic experience via metrics like cognition, perception, and intensity–and the Yale-Brown Obsessive Compulsive Scale (YBOCS)–which measures an individual’s obsessive-compulsive symptoms, such as the compulsion to act on unwanted thoughts or thoughts that cause anxiety [11][4].
The results from the trial showed a decrease in OCD symptoms in all subjects during one or more of the sessions, as shown by reductions of 23% to 100% in the YBOCS score [4]. It is important to note, however, that there was no clear dose-response relationship between the change in YBOCS score and the intensity of the experience measured by the HRS. This indicates that psilocybin could be effective in treating OCD even at the very low dose (25 micrograms/kg). Once again, the researchers noted that although psilocin’s interaction with serotonin receptors correlated with the patients’ experiences, the exact mechanisms of how and why OCD symptoms decreased have yet to be discovered [4].
The implications of the above studies are extensive, and many questions about these compounds and their effects on the human psyche remain. For example, the scientists at the Imperial College London and New York University acknowledge that, among other factors not tested for, the patients’ perceived sense of safety regarding the treatment may have had an impact on their levels of depression following the treatment [2][3]. Thus, further research is required to assess what other factors affect the success of the psilocybin treatment. Other questions regarding psilocybin include its legality. Today, psilocybin maintains its Schedule I classification as an abuse-forming drug with no medicinal purpose, putting it on the same level as heroin. However, a recent paper published by scientists at Johns Hopkins University calls for a reclassification of the mushroom to a possibly more appropriate Schedule IV drug, with low potential for abuse and potential medical use [12].
The studies evaluated show that psilocybin treatment is effective in treating a variety of psychiatric disorders, such as depression, anxiety, and obsessive-compulsive disorder. In each case the patient-volunteers experienced a decrease in the symptoms of the psychiatric disorders in question, both in the short- and long-term, speculated to be a result of the interactions between the psilocin and serotonin receptors in the patients’ brains [2][3][4]. These results show that psilocybin’s potential as a treatment for psychiatric disorders should be taken seriously and investigated further. Moreover, positive results in pilot studies of MDMA as a treatment for PTSD suggest that perhaps even other psychedelics could be used to treat psychiatric disorders [13]. These initial trials are evidence that the stigmas of the past should not impede future research into these potentially life-changing substances.
References
- Mental disorders affect one in four people. (2013, July 29). Retrieved from https://www.who.int/whr/2001/media_centre/press_release/en/
- Carhart-Harris, R. L., Roseman, L., Bolstridge, M., Demetriou, L., Pannekoek, J. N., Wall, M. B., . . . Nutt, D. J. (2017). Psilocybin for treatment-resistant depression: FMRI-measured brain mechanisms. Scientific Reports,7 (1). doi:10.1038/s41598-017-13282-7
- Ross, S., Bossis, A., Guss, J., Agin-Liebes, G., Malone, T., Cohen, B., . . . Schmidt, B. L. (2016). Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: A randomized controlled trial. Journal of Psychopharmacology,30 (12), 1165-1180. doi:10.1177/0269881116675512
- Ballenger, J. (2008). Safety, Tolerability, and Efficacy of Psilocybin in 9 Patients With Obsessive-Compulsive Disorder. Yearbook of Psychiatry and Applied Mental Health,2008 , 242-243. doi:10.1016/s0084-3970(08)70820-x
- Hasler, F., Bourquin, D., Brenneisen, R., Bär, T., & Vollenweider, F. (1997). Determination of psilocin and 4-hydroxyindole-3-acetic acid in plasma by HPLC-ECD and pharmacokinetic profiles of oral and intravenous psilocybin in man. Pharmaceutica Acta Helvetiae,72 (3), 175-184. doi:10.1016/s0031-6865(97)00014-9
- Fantegrossi, W. E., Murnane, K. S., & Reissig, C. J. (2008). The behavioral pharmacology of hallucinogens. Biochemical Pharmacology,75 (1), 17-33. doi:10.1016/j.bcp.2007.07.018
- Al-Harbi, K. S. (2012). Treatment-resistant depression: Therapeutic trends, challenges, and future directions. Patient Preference and Adherence, 369. doi:10.2147/ppa.s29716
- Depression. (2018, March 22). Retrieved from http://www.who.int/news-room/fact-sheets/detail/depression
- Murray, E. A., Wise, S. P., & Drevets, W. C. (2011). Localization of Dysfunction in Major Depressive Disorder: Prefrontal Cortex and Amygdala. Biological Psychiatry,69 (12). doi:10.1016/j.biopsych.2010.09.041
- Barrett, F. S., Johnson, M. W., & Griffiths, R. R. (2015). Validation of the revised Mystical Experience Questionnaire in experimental sessions with psilocybin. Journal of Psychopharmacology,29 (11), 1182-1190. doi:10.1177/0269881115609019
- Obsessive-Compulsive Disorder. (n.d.). Retrieved from https://www.nimh.nih.gov/health/topics/obsessive-compulsive-disorder-ocd/index.shtml
- Johnson, M.W., et al., The abuse potential of medical psilocybin according to the 8 factors of the Controlled Substances Act, Neuropharmacology (2018), https://doi.org/10.1016/j.neuropharm.2018.05.012
- Mithoefer, M. C., Mithoefer, A. T., Feduccia, A. A., Jerome, L., Wagner, M., Wymer, J., . . . Doblin, R. (2018). 3,4-methylenedioxymethamphetamine (MDMA)-assisted psychotherapy for post-traumatic stress disorder in military veterans, firefighters, and police officers: A randomised, double-blind, dose-response, phase 2 clinical trial. The Lancet Psychiatry,5 (6), 486-497. doi:10.1016/s2215-0366(18)30135-4