Getting a cancer diagnosis is a life-altering event, but few diagnoses are as grim as being told you have a glioblastoma. Glioblastoma multiforme (GBM) is a very aggressive form of cancer that starts in the brain and rapidly invades the healthy tissue around it. The rapid growth and complexity of the tumor make it very difficult to treat, leading to a median survival time of around 12 months with as little as 5% of patients surviving five years after their initial diagnosis [1][2][3]. Unfortunately, these statistics haven’t changed much since the current standard of care for GBM was established in 2005. Even when patients do go through a successful treatment, GBM tumors are notorious for recurring more aggressively than the initial tumor [4]. For the last 15 years, doctors have been treating patients’ GBM using surgery, chemotherapy, and radiation; in the meantime, research labs have been working tirelessly to develop treatments that more effectively fight off GBM. While the prognosis for patients with GBM remains bleak, ongoing research is learning from the deficiencies in existing treatments in order to prolong patient survival and work towards a cure.
Background
Glioblastoma multiforme is both the most prevalent and deadliest form of primary brain tumor, a tumor that begins in the brain rather than metastasizing from somewhere else in the body [5]. The name of the tumor tells us a few things about it. First, the “glio” in glioblastoma means that the tumor is composed of glial cells gone wrong. In a healthy adult brain, several types of glia work together, extracting specific nutrients from the blood, cleaning up excess neurotransmitters, insulating axons for faster signal conduction, mounting immune attacks against infection, and even doing some of their own signaling [6]. While the glia themselves don’t divide, the healthy adult brain harbors a reserve of cells that can divide indefinitely and differentiate to become different types of glia [7]. Thus, glia have important responsibilities in the healthy adult brain, but capabilities like cell division are part of what makes it possible for GBM to form.
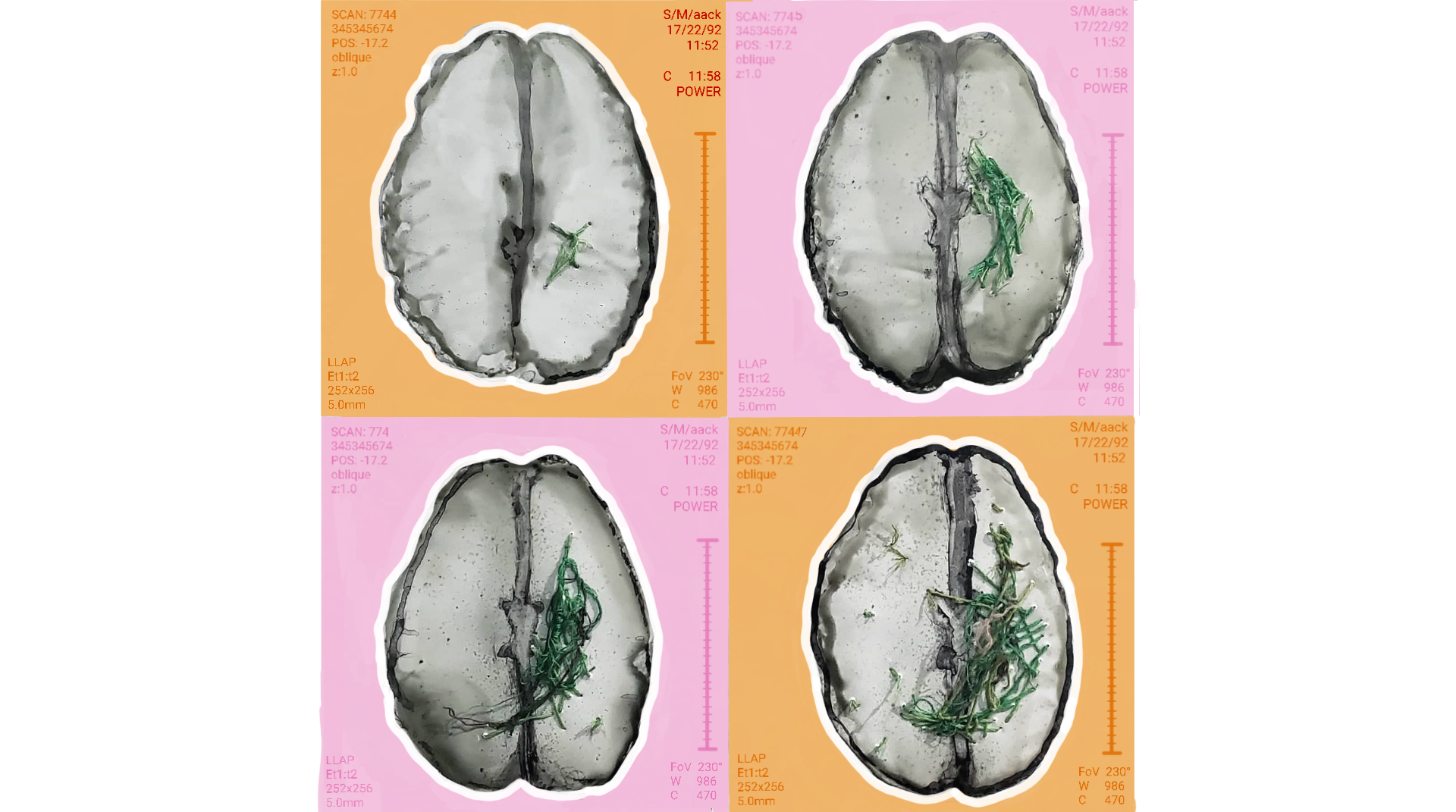
As well as being a glial tumor, GBM is “multiforme.” This means that within one tumor, there are regions with different genetic, cellular, and tissue-level characteristics [5]. From a genetic standpoint, GBM tumors also contain a multitude of different genetic mutations that disrupt processes that are normally in place to keep cell division and growth in check. On the cellular level, the size and type of different cells in the tumor is highly variable, including small cells and densely packed cells with multiple or abnormal nuclei [5]. On the tissue level, these tumors have areas with irregular blood vessels and high density, rapidly-dividing cells. The abnormal vessels aren’t structurally sound, which results in leaks, clots, and pockets of dead cells within the areas of proliferating ones [8][9]. Overall, this combination of rapid cell proliferation and blood vessel growth near the border of tumor tissue and healthy tissue is thought to be how GBM makes its aggressive spread into otherwise-healthy brain areas [8]. With all this complexity, a treatment that works against one portion of the tumor may not be effective against all parts of the tumor or work the same way in different patients.
Current Treatments
Similar to the treatment of other types of cancer, the standard of care for GBM includes surgical removal of the tumor, chemotherapy, and radiation, options that usually just prolong a patient’s life rather than cure their cancer. These treatments are inadequate in the fight against GBM due to the complexity of the tumor and the brain itself. Surgical debulking of the tumor is the first line of treatment against GBM, and analysis from the results of many studies has concluded that the more of a patient’s tumor is removed, the higher their chance of survival 6 months, 12 months, and 2 years after their surgery [10][11][12]. Yet full tumor removal isn’t always possible for several reasons. GBM is particularly invasive to surrounding healthy tissue, meaning that surgeons are not always able to see the extent of tumor spread even when they’re able to remove the majority of it [13]. Another complicating factor is the location of a patient’s tumor. If the tumor is infiltrating a particularly high-risk area of the brain, it may not be possible to remove it without introducing surgically-created impairments such as paralysis, loss of language abilities, or even losing the ability to breathe independently. In this case, it is only a matter of time until the tumor creates an impairment, and the surgeon will leave the tumor in this high-risk area so that the patient can retain their abilities as long as possible [13].
After surgery, most patients with GBM begin radiation therapy alongside a combination of several pharmaceutical agents in attempts to control tumor growth [14][15][16]. Radiation therapy works by damaging cells’ DNA. Since tumor cells go through the cell cycle so rapidly and cannot repair their DNA quickly enough to be viable when they reach the point of cell division, the cells proceed towards cell death rather than continuing to proliferate [17]. Normal cells, on the other hand, are able to repair damage from radiation more rapidly than cancer cells and can return to business as usual [17]. This dichotomy isn’t perfect though; some healthy cells get caught in the crossfire of radiation beams and aren’t able to recover from the damage when delivered at too high a dose [14][15][17]. Recent advances in radiation therapy include optimizing the dosage for elderly patients and improving the tumor volume targeted as brain imaging technologies have improved, though radiation alone is not enough to effectively heal a patient [14].
Along with radiation, many GBM patients choose to treat their disease with the chemotherapy drug temozolomide (TMZ) [14][15][16][18][19][20]. In some ways, TMZ is different from how many people may have seen chemotherapy depicted in popular media. For starters, TMZ is taken as a pill rather than as an intravenous drug, which saves patients the trouble of commuting to cancer centers for daily treatment and allows for specific pharmacological properties [20]. The unique structure of TMZ molecules confers the drug’s specificity for action in tumor tissue. TMZ is highly sensitive to pH and becomes activated in environments that are more basic than the body’s normal pH of 7.4. Conveniently for scientists, the pH surrounding a GBM tumor is slightly more basic than the rest of the body, meaning that TMZ can travel relatively safely through the rest of the body and only become activated once it’s at the edge of the tumor [20]. Once activated, TMZ silences gene transcription and prevents cell growth [20][21]. As with the damage caused by radiation, any normal cells affected have a mechanism of undoing the changes caused by TMZ, and tumor cells do not [21]. As with other chemotherapies, however, TMZ is limited in its benefits because the drug has difficulty getting from the blood to the tumor cells, high doses can cause systemic toxic effects, and tumor cells can develop resistance through DNA repair mechanisms [22].
There are a variety of other treatments approved for use, either in combination with those previously mentioned or used as second-line treatments in the case of a tumor recurrence, though none have created a drastic change in patient prognosis. Among these include various neuropharmaceuticals, gene therapies, and non-invasive electrical stimulation devices [23][24][25][26]. The overall consensus is that these treatments are technically effective at prolonging patients’ lives, otherwise the United States Food and Drug Administration wouldn’t approve them for use in patients. However, the true clinical significance of these treatments is minimal when considering the remarkably low bar for survival that’s present for GBM therapies. To develop therapies that not only focus on extending patients’ lives by a month at a time, but treatments that focus on an actual cure, scientists must learn from the shortcomings of existing treatments.
Developing treatments
Effective treatment for GBM remains elusive in part because nobody truly knows what causes it to begin with. While there are a few genetic mutations that are common among tumor cells, there are no known inherited causes or environmental factors that lead to GBM. When researchers don’t know what causes the tumor in the first place, it is exceedingly more difficult to develop effective, targeted pharmaceutical treatments. Similarly, without knowing the true cause of GBM, animal models used for pharmaceutical tests are limited in their clinical relevance because their tumors are often caused by only one type of simple gene mutation or by injection of a pre-made tumor when human GBM likely develops from a highly complex mechanism. New treatments must also figure out how to penetrate the entirety of the brain and kill individual tumor cells, avoiding normal cells, without physicians needing to see and pre-identify areas for treatment like with surgery or radiation. Thankfully, the field of GBM research is persistent, and there are many promising treatments in preclinical studies that have been developed out of the pitfalls of previous ones.
One category of treatments making meaningful headway in preclinical and clinical studies is immunotherapy, a group of treatments that aim to control the body’s immune system to help fight the tumor [27]. There are several types of immunotherapies including vaccines designed to increase the immune response to tumors, controlled viruses that infect and kill tumor cells, engineered immune cells that seek and destroy tumor cells, agents that block the activity of mutated immune cells in the tumor, and molecules that inhibit mechanisms the tumor uses to avoid the immune system [28]. Some of these have been FDA-approved for other types of cancers, but GBM is more challenging to treat with these methods because of the previously-discussed heterogeneous nature of the solid tumor as well as the danger that comes with intentionally creating a strong immune response in the brain [28]. GBM vaccines are a promising option for activating the immune system to fight a tumor once it’s been discovered [29]. Researchers are currently studying vaccines made of molecules called tumor antigens, which are present on tumor cells but not on normal cells. Some of these antigens are mutated versions of proteins that are present in other cells, whereas others include whole cells that are killed with radiation and subsequently injected [29]. There are several of these vaccines currently being tested for their safety and efficacy [30][31][32]. The overall consensus of researchers in the field is that there are a variety of immunotherapies that can provide modest benefit when administered on their own, and the likely solution to truly improve patient outcomes will be to combine several different immunotherapies that work with different mechanisms to fight the tumor from multiple angles [28].
Other researchers are taking a different approach to pinpoint weaknesses in the GBM tumor. One such study is on the drug Gboxin, a small molecule that works by interfering with the cells’ metabolism, inhibiting the cells’ ability to make ATP [33]. While researchers found that Gboxin inhibited cellular metabolism in many cell types, they observed that only their tumor cells died from this inhibition; non-tumor cells such as embryonic and neonatal cell cultures were able to recover. Researchers propose that this difference in effect is due to the unique environment within tumor cells’ mitochondria and the failure of an important protein complex in the electron transport chain to recover from the damage inflicted by Gboxin. One exciting key point is that the researchers working on this treatment used a GBM mouse model with mutations in several tumor suppressor genes, rather than a model where the tumor is created with only one mutation, as other studies have used. The increased complexity of their model means that their results are more likely to reflect how the drug would work against human GBMs. When considering how to make the transition from mouse models to human patients, researchers should consider that Gboxin has difficulty moving from the blood into the brain and tumor tissue. In preclinical studies, they overcame this challenge by administering the drug at a continuously high but therapeutic dose so that an appropriate concentration could make it to the brain [33]. For humans, ensuring continuous treatment with a high-enough dosage to have therapeutic effects could be very complicated and even be a barrier to treatment for some. In this case, treatments would come down to decisions between patients and their healthcare teams, which would weigh the risks and the benefits of treatment, quality of life, and even the financial impact of care.
Another promising preclinical study involves an identifying protein that was newly found to be common among invasive gliomas like GBM. This biomarker is called fatty acid binding protein 3 (FABP3), and under normal circumstances, it is important for transporting the molecules that make up the membrane of a lysosome [34]. When this protein is silenced in patient-derived GBM cells cultured in a Petri dish, the cells die more rapidly, and when the protein is hyperactivated, tumor activity increases. The silenced FABP3 is unable to deliver lysosomal membrane molecules, which leads to an unstable lysosomal membrane that leaks degradative enzymes into the cytoplasm, damaging structures the cell needs to survive. Learning about this lysosomal membrane permeabilization (LMP) pathway to cell death has inspired researchers to study drugs that could induce the same type of death for GBM cells. One research team in particular looked at an antihistamine called clemastine because of its ability to cross the blood-brain barrier and found that it could induce GBM cell death via the LMP mechanism as they had proposed without causing other cells’ death as long as the dose was within a therapeutic range. Interestingly, they found that clemastine had the greatest cytotoxic effect on migrating tumor cells at the leading edge of an invasive tumor and did not show any noticeable cytotoxicity or side effects off target from the tumor cells [34]. The specificity of this drug for the most invasive migrating cells is encouraging considering the difficulty of removing those cells surgically or targeting them with radiation. While future studies on clemastine are necessary to determine how the treatment might be combined with others for maximal benefit, it is exciting and encouraging that treatments like this one may begin to fill holes left by other treatments as the body of research grows.
Future of GBM Treatments
Glioblastoma still has many mysteries for researchers and physicians working to cure their patients. Currently approved treatments for GBM are broad and ineffective, leaving behind dangers such as migrating, chemotherapy-resistant cells that cause recurrence. Yet, in the true scientific spirit, researchers are learning from the limitations of previous work and taking advantage of our ever-increasing understanding of biological processes. The more scientists have learned about cell death mechanisms, the better their ability to develop treatments such as clemastine and Gboxin. Treatments like drug-induced lysosomal membrane permeabilization and blocking ATP production are only possible because neuroscience research continues to evolve and uncover different processes every day. Pharmaceutical studies also are becoming more clinically relevant as more factors associated with GBM are better understood. As we saw with Gboxin, more complex models for evaluating drug performance are more likely to reflect the drug’s behavior when fighting against a patient’s GBM [33]. Though the prognosis for patients is still harsh, the publication rate for peer-reviewed articles about GBM has exploded since 1995 and shows no signs of slowing [35]. With so many brilliant scientific minds coming together, it is only a matter of time before more beneficial treatments come to fruition.
References
- Witthayanuwat, S., Pesee, M., Supaadirek, C., Supakalin, N., Thamronganantasakul, K., & Krusun, S. (2018). Survival Analysis of Glioblastoma Multiforme. Asian Pacific journal of cancer prevention : APJCP, 19(9), 2613–2617. https://doi.org/10.22034/APJCP.2018.19.9.2613
- Salcman, M. (1980). Survival in Glioblastoma. Neurosurgery, 7(5), 435–439. doi: 10.1227/00006123-198011000-00001
- Cantrell, J. N., Waddle, M. R., Rotman, M., Peterson, J. L., Ruiz-Garcia, H., Heckman, M. G., … Trifiletti, D. M. (2019). Progress Toward Long-Term Survivors of Glioblastoma. Mayo Clinic Proceedings, 94(7), 1278–1286. doi: 10.1016/j.mayocp.2018.11.031
- Gallego O. (2015). Nonsurgical treatment of recurrent glioblastoma. Current oncology (Toronto, Ont.), 22(4), e273–e281. https://doi.org/10.3747/co.22.2436
- Holland E. C. (2000). Glioblastoma multiforme: the terminator. Proceedings of the National Academy of Sciences of the United States of America, 97(12), 6242–6244. https://doi.org/10.1073/pnas.97.12.6242
- Jäkel, S., & Dimou, L. (2017). Glial Cells and Their Function in the Adult Brain: A Journey through the History of Their Ablation. Frontiers in Cellular Neuroscience, 11. doi: 10.3389/fncel.2017.00024
- Dimou, L., & Gallo, V. (2015). NG2-glia and their functions in the central nervous system. Glia, 63(8), 1429–1451. https://doi.org/10.1002/glia.22859
- Rong, Y., Durden, D. L., Meir, E. G. V., & Brat, D. J. (2006). ‘Pseudopalisading’ Necrosis in Glioblastoma: A Familiar Morphologic Feature That Links Vascular Pathology, Hypoxia, and Angiogenesis. Journal of Neuropathology & Experimental Neurology, 65(6), 529–539. doi: 10.1097/00005072-200606000-00001
- Brat, D. J., Castellano-Sanchez, A. A., Hunter, S. B., Pecot, M., Cohen, C., Hammond, E. H., … Meir, E. G. V. (2004). Pseudopalisades in Glioblastoma Are Hypoxic, Express Extracellular Matrix Proteases, and Are Formed by an Actively Migrating Cell Population. Cancer Research, 64(3), 920–927. doi: 10.1158/0008-5472.can-03-2073
- Brown, T. J., Brennan, M. C., Li, M., Church, E. W., Brandmeir, N. J., Rakszawski, K. L., Patel, A. S., Rizk, E. B., Suki, D., Sawaya, R., & Glantz, M. (2016). Association of the Extent of Resection With Survival in Glioblastoma: A Systematic Review and Meta-analysis. JAMA oncology, 2(11), 1460–1469. https://doi.org/10.1001/jamaoncol.2016.1373
- Chaichana, K. L., Jusue-Torres, I., Navarro-Ramirez, R., Raza, S. M., Pascual-Gallego, M., Ibrahim, A., Hernandez-Hermann, M., Gomez, L., Ye, X., Weingart, J. D., Olivi, A., Blakeley, J., Gallia, G. L., Lim, M., Brem, H., & Quinones-Hinojosa, A. (2014). Establishing percent resection and residual volume thresholds affecting survival and recurrence for patients with newly diagnosed intracranial glioblastoma. Neuro-oncology, 16(1), 113–122. https://doi.org/10.1093/neuonc/not137
- Sanai, N., Polley, M.-Y., Mcdermott, M. W., Parsa, A. T., & Berger, M. S. (2011). An extent of resection threshold for newly diagnosed glioblastomas. Journal of Neurosurgery, 115(1), 3–8. doi: 10.3171/2011.2.jns10998
- Haj, A., Doenitz, C., Schebesch, K. M., Ehrensberger, D., Hau, P., Putnik, K., Riemenschneider, M. J., Wendl, C., Gerken, M., Pukrop, T., Brawanski, A., & Proescholdt, M. A. (2017). Extent of Resection in Newly Diagnosed Glioblastoma: Impact of a Specialized Neuro-Oncology Care Center. Brain sciences, 8(1), 5. https://doi.org/10.3390/brainsci8010005
- Mann, J., Ramakrishna, R., Magge, R., & Wernicke, A. G. (2018). Advances in Radiotherapy for Glioblastoma. Frontiers in neurology, 8, 748. https://doi.org/10.3389/fneur.2017.00748
- Villà, S., Balañà, C., & Comas, S. (2014). Radiation and concomitant chemotherapy for patients with glioblastoma multiforme. Chinese journal of cancer, 33(1), 25–31. https://doi.org/10.5732/cjc.013.10216
- Stupp, R., Mason, W. P., Bent, M. J. V. D., Weller, M., Fisher, B., Taphoorn, M. J., … Mirimanoff, R. O. (2005). Radiotherapy plus Concomitant and Adjuvant Temozolomide for Glioblastoma. New England Journal of Medicine, 352(10), 987–996. doi: 10.1056/nejmoa043330
- Baskar, R., Dai, J., Wenlong, N., Yeo, R., & Yeoh, K. W. (2014). Biological response of cancer cells to radiation treatment. Frontiers in molecular biosciences, 1, 24. https://doi.org/10.3389/fmolb.2014.00024
- Barciszewska, A.-M., Gurda, D., Głodowicz, P., Nowak, S., & Naskręt-Barciszewska, M. Z. (2015). A New Epigenetic Mechanism of Temozolomide Action in Glioma Cells. Plos One, 10(8). doi: 10.1371/journal.pone.0136669
- Fisher, T., Galanti, G., Lavie, G., Jacob-Hirsch, J., Kventsel, I., Zeligson, S., … Toren, A. (2007). Mechanisms Operative in the Antitumor Activity of Temozolomide in Glioblastoma Multiforme. The Cancer Journal, 13(5), 335–344. doi: 10.1097/ppo.0b013e318157053f
- Zhang, J., Stevens, M. F., & Bradshaw, T. D. (2012). Temozolomide: Mechanisms of Action, Repair and Resistance. Current Molecular Pharmacology, 5(1), 102–114. doi: 10.2174/1874467211205010102
- Jin, B., Li, Y., & Robertson, K. D. (2011). DNA methylation: superior or subordinate in the epigenetic hierarchy?. Genes & cancer, 2(6), 607–617. https://doi.org/10.1177/1947601910393957
- Kumari, S., Ahsan, S. M., Kumar, J. M., Kondapi, A. K., & Rao, N. M. (2017). Overcoming blood brain barrier with a dual purpose Temozolomide loaded Lactoferrin nanoparticles for combating glioma (SERP-17-12433). Scientific Reports, 7(1). doi: 10.1038/s41598-017-06888-4
- Yamada, T., Tsuji, S., Nakamura, S., Egashira, Y., Shimazawa, M., Nakayama, N., … Hara, H. (2020). Riluzole enhances the antitumor effects of temozolomide via suppression of MGMT expression in glioblastoma. Journal of Neurosurgery, 1–10. doi: 10.3171/2019.12.jns192682
- Kinzel, A., Ambrogi, M., Varshaver, M., & Kirson, E. D. (2019). Tumor Treating Fields for Glioblastoma Treatment: Patient Satisfaction and Compliance With the Second-Generation Optune® System. Clinical Medicine Insights. Oncology, 13, 1179554918825449. https://doi.org/10.1177/1179554918825449
- Wenger, K. J., Wagner, M., You, S. J., Franz, K., Harter, P. N., Burger, M. C., Voss, M., Ronellenfitsch, M. W., Fokas, E., Steinbach, J. P., & Bähr, O. (2017). Bevacizumab as a last-line treatment for glioblastoma following failure of radiotherapy, temozolomide and lomustine. Oncology letters, 14(1), 1141–1146. https://doi.org/10.3892/ol.2017.6251
- Jain K. K. (2018). A Critical Overview of Targeted Therapies for Glioblastoma. Frontiers in oncology, 8, 419. https://doi.org/10.3389/fonc.2018.00419
- Yang Y. (2015). Cancer immunotherapy: harnessing the immune system to battle cancer. The Journal of clinical investigation, 125(9), 3335–3337. https://doi.org/10.1172/JCI83871
- McGranahan, T., Therkelsen, K. E., Ahmad, S., & Nagpal, S. (2019). Current State of Immunotherapy for Treatment of Glioblastoma. Current treatment options in oncology, 20(3), 24. https://doi.org/10.1007/s11864-019-0619-4
- Ahluwalia, M., Reardon, D., Abad, A., Curry, W., Wong, E., Peereboom, D., … Fenstermaker, R. (2018). ATIM-41. PHASE II TRIAL OF A SURVIVIN VACCINE (SurVaxM) For Newly Diagnosed Glioblastoma. Neuro-Oncology, 20(suppl_6), vi10–vi11. doi: 10.1093/neuonc/noy148.036
- Schumacher, T., Bunse, L., Pusch, S., Sahm, F., Wiestler, B., Quandt, J., … Platten, M. (2014). A vaccine targeting mutant IDH1 induces antitumour immunity. Nature, 512(7514), 324–327. doi: 10.1038/nature13387
- Rampling, R., Peoples, S., Mulholland, P. J., James, A., Al-Salihi, O., Twelves, C. J., … Ritchie, J. W. A. (2016). A Cancer Research UK First Time in Human Phase I Trial of IMA950 (Novel Multipeptide Therapeutic Vaccine) in Patients with Newly Diagnosed Glioblastoma. Clinical Cancer Research, 22(19), 4776–4785. doi: 10.1158/1078-0432.ccr-16-0506
- Phuphanich, S., Wheeler, C. J., Rudnick, J. D., Mazer, M., Wang, H., Nuño, M. A., … Yu, J. S. (2012). Phase I trial of a multi-epitope-pulsed dendritic cell vaccine for patients with newly diagnosed glioblastoma. Cancer Immunology, Immunotherapy, 62(1), 125–135. doi: 10.1007/s00262-012-1319-0
- Shi, Y., Lim, S. K., Liang, Q., Iyer, S. V., Wang, H.-Y., Wang, Z., … Parada, L. F. (2019). Gboxin is an oxidative phosphorylation inhibitor that targets glioblastoma. Nature, 567(7748), 341–346. doi: 10.1038/s41586-019-0993-x
- Le Joncour, V., Filppu, P., Hyvönen, M., Holopainen, M., Turunen, S. P., Sihto, H., Burghardt, I., Joensuu, H., Tynninen, O., Jääskeläinen, J., Weller, M., Lehti, K., Käkelä, R., & Laakkonen, P. (2019). Vulnerability of invasive glioblastoma cells to lysosomal membrane destabilization. EMBO molecular medicine, 11(6), e9034. https://doi.org/10.15252/emmm.201809034
- Groneberg, D. A., Addicks, A. M., Bendels, M. H., Quarcoo, D., Jaque, J., & Brüggmann, D. (2017). Glioblastoma research: US and international networking achievements. Oncotarget, 8(70), 115730–115735. https://doi.org/10.18632/oncotarget.21270
