To most, the act of killing another human is unthinkable. And yet, for the victims of the thousands of homicides and millions of violent assaults that occur every year, this criminal behavior is all too real [1]. But what would motivate someone to commit such vicious acts of harm? For millennia, people have believed that the cause of violent behavior lies within the brain. The ancient Romans were documented to have “treated” (albeit loosely defined) behavioral disorders by drilling a hole into the subject’s skull [2]. Though this method was later found ineffective, the Romans were well ahead of their time in pinpointing the brain as a source of the behavior. While this discovery was grounds for further research, many following experiments in the 19th and 20th centuries were misguided, criminalizing mentally ill subjects even if they had not performed any criminal acts [3]. Still, this possible uncovering of a link between neurological dysfunction and aberrant, sometimes criminal behavior has not been ignored, forming the basis of much of today’s crime research [3]. Current research suggests that abnormalities in the brain’s regulatory systems for aggression and empathy can help explain why some individuals act in such criminal manners, specifically those afflicted with bipolar disorder (BPD).
The Gas and the Brakes: Brain Structures Involved in Aggression
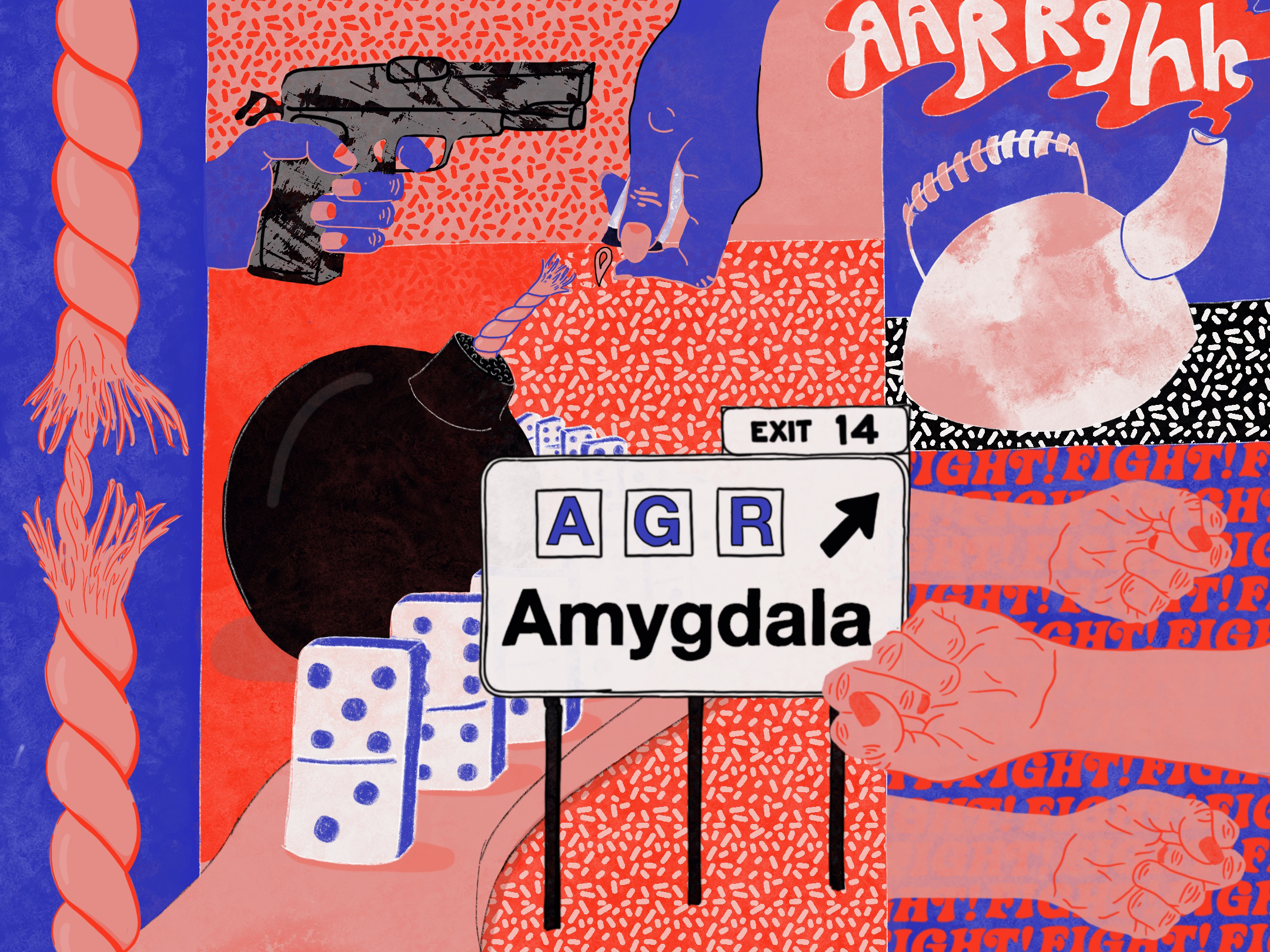
As researchers have investigated why people commit violent crimes, they have managed to uncover one vital clue: violent crime maintains a strong connection to unusual patterns of increased aggression. During their lifetime, around 7.3% of all people will experience intermittent explosive disorder, a condition in which people burst into violent rages [4]. Given the relatively high prevalence of disorders tied to aggression, significant research has been conducted into how these disorders function. One model, known as the aggressive diathesis model, attempts to explain aggression in terms of two main forces: ‘braking’ mechanisms that help control it and ‘driving’ mechanisms that induce and sustain it [5].
Identifying these two forces and constructing the aggressive diathesis model required heavy and meticulous research. Through his research, American physiologist John F. Fulton was able to lay out the foundations of this model [3]. In 1935, he performed a landmark operation in which two chimpanzees had part of their prefrontal cortices -- the frontmost portion of the brain -- removed. The operation left the chimpanzees completely devoid of emotion and much less likely to engage in aggressive behavior, suggesting that the prefrontal cortex played a role in regulating these behaviors [6]. And while the prefrontal cortex is important in regulating aggression as a whole, recent research suggests that the orbitofrontal cortex, a region within the prefrontal cortex, may play an even more specific part in the braking mechanism of aggression [3]. These observations have extended beyond chimpanzee research, appearing in human case studies as well. Phineas Gage, a construction foreman, had a work-related accident in which a metal rod pierced his frontal lobe, damaging his orbitofrontal cortex. Following the accident, Gage expressed unusually antisocial and aggressive behavior [3]. Similarly, one study of men and women with histories of aggression found that they carried more deformities in their orbitofrontal cortices than those without such histories [7]. With this evidence, researchers speculate that the orbitofrontal cortex may be significant for reducing aggression through this braking mechanism, but further research and experimental evidence will be needed to mitigate existing ambiguity in the strength of this relationship [7].
While the orbitofrontal cortex may act as the braking component of the aggressive diathesis model and work to suppress aggressive behavior, there still remains the driving component that induces and sustains aggression. Currently, researchers believe there are two main centers in the brain that contribute to this: the amygdala, a structure of the limbic system implicated in processing emotion, especially fear and anxiety [8]. In one study, three different groups of subjects -- one with diagnosed borderline-personality disorder (BPD), one with diagnosed schizotypal personality disorder, and one health control -- were shown images that were categorized as either emotionally unpleasant, neutral, or emotionally pleasant [9]. After being shown the images, the experimenters found that only subjects with BPD had exhibited greater amygdala activity when responding to emotionally unpleasant and pleasant images while maintaining low activity when shown neutral images. When subjects were asked to self-report their emotional responses to the images, BPD subjects were found to more frequently under-report their reactions with respect to their amygdala activity than the other two groups, suggesting that they may not have fully recognized the extent of their emotional responses [9]. To that end, patterns of amygdala function may offer insight into the structure’s role in promoting aggression within individuals with BPD. A similar study also investigates this possibility by collecting and analyzing functional MRI (fMRI) brain images of six women with BPD and six women without any major psychological disorders after exposing them all to emotionally aversive pictures, discovering that the six BPD individuals exhibited a greater increase in amygdala activity in response to the pictures [10]. Knowing the amygdala’s role in regulating fear- and anxiety-related emotions, its role in driving aggression as part of Fulton’s model is sensible, yet the observed increase in activity in specifically BPD subjects remains of particular interest. While this phenomenon is consistent with elevated sensitivity and strong reactions to emotional stimuli characteristic of patients with BPD, the amygdala’s role in inspiring this behavior will need further investigation, especially in the disparity in activity between BPD subjects and subjects without disorders characterized by aggression [9].

Other Physiological Drivers of Criminal Behavior
Still, an impaired ability to control aggression through these two mechanisms may not be the only factor affecting the likelihood of committing a violent crime; disorders that impair moral and empathetic judgement may also reduce criminals’ ability to retain culpability for their actions [11]. In one study conducted at a North American correctional facility, 121 adult males were sorted by their scores on a psychopathic evaluation into low, medium, and high-psychopathy groups. Participants were then shown an image of a hand or foot on their dominant side in either painful or non-painful situations, like pinching a finger in a door, and were instructed to imagine either the painful situation happening to themselves or to someone else. Following fMRI imagery showed that participants in medium- and high-psychopathy groups exhibited significantly lower activity of the amygdala and limbic system when imagining the painful situation happening to someone else than when imagining themselves in a similar situation. Additionally, when imagining the pain happening to someone else, medium- and high-psychopathy participants demonstrated increased activity of the ventral striatum, a brain region in the limbic system that is correlated with conduct disorder and rebellious behavior in adolescents [11]. Patterns of activity in each of these structures in psychopathic subjects may explain a lack of empathy for others experiencing pain, which, as some researchers speculate, may account for their violent criminal behavior [2].
Constructing a Treatment Plan
Considering a possible physiological impetus behind some criminal behavior, rehabilitative measures may hold promise in reducing the incidence of violent crime. When it comes to aggressive behavior, mood stabilization therapies may help by reducing irritability; psychotherapy, too, can promote less impulsive behavior from aggressive patients, helping them take control over their aggression [2]. Unfortunately, psychopathy, as some researchers have determined, does not respond well to traditional group therapies, drug therapies, and other therapies for psychological disorders [2]. However, Michael F. Caldwell, a professor of psychology at the University of Wisconsin-Madison, devised a method termed “decompression treatment” that attempts to wean people with BPD off of a self-centered mentality that might push them toward psychopathy by performing small tasks involving low amounts of cooperation [12]. Eventually, people with BPD who undergo decompression treatment may also use traditional therapies with greater success than those who have not undergone decompression treatment, largely because they are less likely to use the therapy setting as a way to create excuses for their behavior or manipulate vulnerable attendees. Among 248 incarcerated males, Caldwell found that his decompression treatment reduced overall criminal reoffense rates from 78% to 56%, as well as a reduction of 36% to 18% in reoffense rates of violent crime, demonstrating the merit behind Caldwell’s model of treatment. With enough proper use, the treatment may be a useful approach to mitigating criminal behavior among those with aggressive disorders [12].

Understanding criminal behavior is a complicated and demanding task, but by breaking it down into its two components, aggression and psychopathy, we can tackle the smaller issues accompanying it and devise more effective treatment methods for those characterized by these patterns of behavior. While the effectiveness of these treatments and therapies may vary from person to person, the overall efficacy suggests that we can take many more steps to address and resolve criminal behavior through rehabilitation rather than incarceration. Ultimately, it is up to us to decide whether to steer our focus toward rehabilitation or retribution, but without the former, many criminals lose the chance to better themselves.
References
- Sumner, S. A., Mercy, J. A., Dahlberg, L. L., Hillis, S. D., Klevens, J., & Houry, D. (2015). Violence in the United States: Status, Challenges, and Opportunities. JAMA, 314(5), 478-488. https://doi.org/10.1001/jama.2015.8371.
- Kiehl, K. A., & Hoffman, M. B. (2011). THE CRIMINAL PSYCHOPATH: HISTORY, NEUROSCIENCE, TREATMENT, AND ECONOMICS. Jurimetrics, 51, 355-397.
- Faria, M. A., Jr. (2013). Violence, mental illness, and the brain - A brief history of psychosurgery: Part 1 - From trephination to lobotomy. Surgical neurology international, 4, 49. https://doi.org/10.4103/2152-7806.110146.
- Kessler, R. C., Coccaro, E. F., Fava, M., Jaeger, S., Jin, R., & Walters, E. (2006). The prevalence and correlates of DSM-IV intermittent explosive disorder in the National Comorbidity Survey Replication. Archives of general psychiatry, 63(6), 669-678. https://doi.org/10.1001/archpsyc.63.6.669.
- Siever, L. J. (2008). Neurobiology of aggression and violence. The American Journal of Psychiatry, 165(4), 429-442. https://doi.org/10.1176/appi.ajp.2008.07111774.
- Fulton, J. F. (1951). The Physiological basis of Psychosurgery. Proceedings of the American Philosophical Society, 95(5), 538-541. Available from: http://www.jstor.org/stable/3143238.
- Séguin, J. R. (2014). The frontal lobe and aggression. European Journal of Developmental Psychology, 6(1), 100-119. https://doi.org/10.1080/17405620701669871.
- Torrico, T. J., & Abdijadid, S. (2020). Neuroanatomy, Limbic System. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538491/.
- Hazlett, E. A., Zhang, J., New, A. S., Zelmanova, Y., Goldstein, K. E., Haznedar, M. M., Meyerson, D., Goodman, M., Seiver, L. J., & Chu, K. W. (2012). Potentiated Amygdala Response to Repeated Emotional Pictures in Borderline Personality Disorder. Biological psychiatry, 72(6), 448-456. https://doi.org/10.1016/j.biopsych.2012.03.027.
- Herpetz, S. C., Dietrich, T. M., Wenning, B., Krings, T., Eberich, S. G., Willmes, K., Thorn, A., & Sass, H. (2001). Evidence of abnormal amygdala functioning in borderline personality disorder: a functional MRI study. Biological Psychiatry, 50(4), 292-298. https://www.doi.org/10.1016/s0006-3223(01)01075-7.
- Decety, J., Chen, C., Harenski, C., & Kiehl, K. A. (2013). An fMRI study of affective perspective taking in individuals with psychopathy: imagining another in pain does not evoke empathy. Frontiers in Human Neuroscience, 7, 489. https://www.doi.org/10.3389/fnhum.2013.00489.
- Caldwell, M. F., & Van Rybroek, G. J. (2001). Efficacy of a Decompression Treatment Model in the Clinical Management of Violent Juvenile Offenders. International Journal of Offender Therapy and Comparative Criminology, 45(4), 469-477. https://doi.org/10.1177/0306624X01454006.