Physical pain is an unavoidable aspect of everyday life. Most of us have experienced the sharp pain that comes with a paper cut, the dull ache of sore muscles, and the all-too-familiar sensation of stubbing a toe on a table leg. But imagine for a second feeling a different sort of pain – one that comes from a part of you that no longer exists.
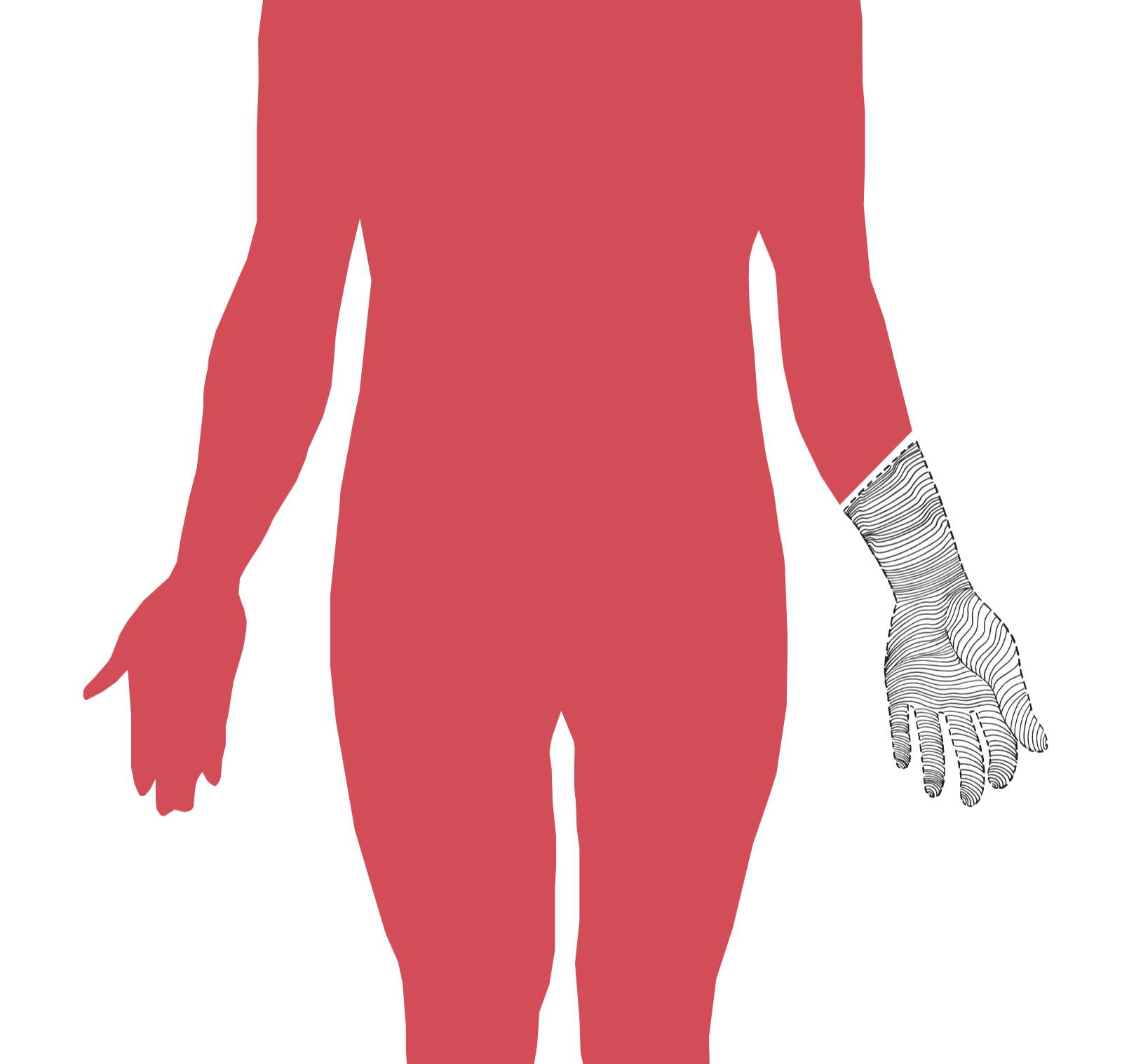
This pain is a constant reality for those who live with phantom limb pain (PLP), or the perception of pain in a body part that has been amputated. It is a common phenomenon experienced by those who undergo amputation, whether due to trauma or chronic illnesses such as cardiovascular disease and diabetes. While the perception of phantom pain can occur in any part of the body, the most common PLP occurs in amputated limbs [9].
The percentage of amputees experiencing PLP soon after their amputation is estimated to vary between 50% and 80%; most estimates for long-term pain similarly range from 50% to 78% [9][6]. The type and duration of these pain experiences spans a wide range as well. Amputees often describe their pain as a burning, stabbing, itching, or shocking sensation that ranges anywhere from severe to mild and may be either constant or exacerbated [9]. Due to the many unique combinations of symptoms experienced by those suffering from PLP, there is currently no consensus on the classification of different types of phantom limb pain. However, it is clear that these amputees do experience pain. What, then, could be the cause of this phenomenon?
Proposed Theories of Phantom Limb Pain
A number of theories have been proposed in an attempt to explain PLP. One such theory involves the formation of neuromas, tangled masses of axons at the site of amputation. Some researchers believe that random firing of these neurons contributes to phantom pain [3]. Another hypothesis suggests that people who suffer from chronic pain form lasting pain memories that become wired into their brain, which would result in a similarity between the phantom pain and the pain they experienced before the amputation [3]. In another theory, researchers propose that the pain memories formed at the time of amputation are internally linked with memories regarding the specific position of the limb, which they refer to as proprioceptive memory. These proprioceptive memories and the associated pain memories are believed to be retained even after amputation, which could account for why some people can still sense and feel pain in their missing limb or even move it [1]. However, all of these theories have gaps in their explanations. The majority of people who have PLP experience it immediately after amputation before neuromas have had time to form, and many veterans who experience PLP after an amputation related to trauma do not have previous pain memories [3][9].
The Sensorimotor Cortex and Cortical Reorganization
Neuromas and pain memories are not the only explanations offered for phantom limb pain. Currently, the most widely accepted theory behind the etiology of this condition involves cortical reorganization of the somatosensory and motor cortices. The primary somatosensory cortex (S1), located in the parietal lobe of the brain, receives information from sensory systems such as touch. The motor cortex (M1), located anterior to the S1 in the frontal lobe, controls the voluntary muscle movements of the body. Both cortices are arranged via somatotopic maps, which link specific areas of the cortices with the body parts they control or receive sensory information from [8]. Cortical reorganization, then, can be seen as any change in the topographies of these neural landscapes.
This cortical reorganization is often seen in patients with PLP. A study conducted by MacIver et al. demonstrated this by examining the extent of cortical reorganization in 13 upper limb amputees. Using functional magnetic resonance imaging (fMRI), the researchers mapped the somatotopic areas that lit up when amputees pursed their lips, and compared them to the scans of participants who had never undergone an amputation. They found that when the amputees pursed their lips, not only was there bilateral activation of the S1/M1 areas related to the face and lip, but also contralateral activation of the amputated hand area [7]. This suggests that the S1/M1 areas devoted to the lip and face had invaded the area that was previously devoted to the now-amputated hand. Similar cortical reorganization has also been found in animals with missing limbs, such as in owl monkeys that have lost a digit [9]. Researchers suspect that this reorganization is the result of an increased excitability of the neurons in the S1/M1 cortices that had previously served only the amputated limb. A change in the production of GABA, an inhibitory neurotransmitter, is believed to be involved in the changed excitability of these nerve cells [3].
Treatments for Phantom Limb Pain
Many treatments being tested to treat PLP draw upon this cortical reorganization theory. One such treatment that has shown positive results is the use of mental imagery. The MacIver et al. study tested the efficacy of mental imagery in their 13 amputees by asking them to imagine moving their phantom limb. Using fMRI, they found that after 6 weeks of doing this exercise, amputees no longer experienced activation of the contralateral hand area, and the activation area of the face and lips was smaller than before the mental imagery exercise. Even their pain levels decreased [7]. In a related treatment, researchers found that mirror therapy, where participants move their intact limb in front of a mirror and associate that movement with the phantom limb, also reduced PLP in participants and reversed cortical reorganization in the S1 [4]. The use of opioids has also been shown to decrease phantom pain, and interestingly, there is also a documented decrease in cortical reorganization in PLP patients who take these opioids [5]. These studies show a correlation between cortical reorganization and pain, with less cortical reorganization associated with less pain experienced in the phantom limb. However, there are limitations to these studies and the cortical reorganization theory. The sample sizes for each of these studies was rather small, and there has not yet been any research conducted on the long-term effects of these treatments. But perhaps the biggest limitation is that we currently lack an explanation as to why cortical reorganization is linked with phantom limb pain. While studies have shown that the reversal of cortical reorganization can decrease the severity of phantom pain itself, it remains unclear whether cortical reorganization is the cause of PLP, or if there is an unknown factor causing both cortical reorganization and PLP.
Conclusion
The link between cortical reorganization and phantom limb pain is apparent. However, it is also apparent that the mechanism behind cortical reorganization is still a mystery, leaving many unanswered questions as to how, why, or even if this phenomenon causes phantom pain. Cortical reorganization and other possible causes of phantom limb pain should be the focus of future research in order to develop more targeted and effective treatments for this mysterious condition.
References
- Anderson-Barnes, V.C., McAuliffe, C., Swanberg, K. M., & Tsao, J.W. (2009). Phantom limb pain – A phenomenon of proprioceptive memory? Medical Hypotheses, 73, 555-558.
- Flor, H., Elbert, T., Knecht, S., Wienbruch, C., Pantev, C., Birbaumer, N., … Taub, E. (1995). Phantom-limb pain as a perceptual correlate of cortical reorganization following arm amputation. Nature, 375, 482-484.
- Flor, H., Nikolajsen, L., & Jensen, T.S. (2006). Phantom limb pain: A case of maladaptive CNS plasticity? Nature Reviews, 7, 873-881.
- Foell, J., Bekrater-Bodmann, R., Diers, M., & Flor, H. (2014). Mirror therapy for phantom limb pain: Brain changes and the role of body representation. European Journal of Pain, 18, 729-739.
- Huse, E., Larbig, W., Flor, H., & Birbaumer, N. (2001). The effect of opioids on phantom limb pain and cortical reorganization. Pain, 90, 47-55.
- Kooijman, C.M., Dijkstra, P.U., Geertzen, J. H.B., Elzinga, A., & van der Schans, C. P. (2000). Phantom pain and phantom sensations in upper limb amputees: an epidemiological study. Pain, 87, 33-41.
- MacIver, K., Lloyd, D. M., Kelly, S., Roberts, N., & Nurmikko, T. (2008). Phantom limb pain, cortical reorganization, and the therapeutic effect of mental imagery. Brain, 131, 2181-2191.
- Purves ,D., Augustine G. J., Fitzpatrick D., Katz, L. C., LaMantia, A.S., McNamara, J.O., & Williams, S. M. (2001). Neuroscience (2nd ed.). Sunderland, MA: Sinauer Associates. Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK11095/
- Weeks, S. R., Anderson-Barnes, V.C., & Tsao, J.W. (2010). Phantom limb pain: Theories and therapies. The Neurologist, 16 (5), 277-286.