Ketamine, a dissociative anesthetic, is notorious for its street reputation as an abused substance. Known by the general public as an illicit club drug, recreational users inhale, ingest, or inject the substance to reach a sense of euphoria. What sets it apart from other recreational drugs is the deep and timeless dissociative state typically termed as “k-holing”, which encompasses out-of-body experiences that–according to its users–are unparalleled by any other drug [1]. The stigmatization of ketamine is mainly centered around three sources: drug abuse, inappropriate use, and potential overdosage. The combination of recent upsurges in substance abuse within the past decade and an ongoing issue surrounding date-rape through the usage of drugs like ketamine have greatly shifted the general public’s opinion of ketamine, even in a medicinal sense.
Despite the contentions held against this drug, a “flip side” offers benefits for the medical field otherwise unknown or dismissed by the general public due to the stigmatization of psychedelic healthcare. What if there were a viable treatment option for side effects from current Parkinson’s medication? What about entertaining the idea of reversing genetic alteration disorders such as Tourette’s? What if we even had a drug capable of initiating neuronal regrowth in the prefrontal lobe and treating a broad spectrum of disorders from treatment-resistant depression to PTSD? The seemingly simple, yet radical idea of promoting ketamine as a therapeutic drug rather than just a sedative provides promising solutions for these conditions that have stumped preexisting medicine within the healthcare field.
Ketamine for Parkinson’s Disease
Throughout the last century, both healthcare providers and researchers struggled to combat the symptoms of Parkinson’s Disease, a progressive neurological condition characterized by the degeneration of neural tissue and dopamine deficiency within the basal ganglia, an area of the brain essential for our day-to-day motions [2] [3]. Simply brushing your teeth, opening the fridge, or putting on socks would feel rough and unwieldy without this structure in our brains. The symptoms of Parkinson’s impair these motions in the form of rigid tremors, muscle stiffness, frozen or slowed movements, and even hallucinations if far enough progressed, and they increase severely over time. Currently one of the most commonly prescribed medications for Parkinson's Disease is Levodopa, a central nervous system agent acting as a precursor for missing dopamine within the brain. Levodopa is used to combat dopamine deficiency, a commonality between Parkinson’s patients [4]. Initially, Levodopa doses administered to patients within the early stages of Parkinson’s provided symptomatic relief. Unfortunately, Levodopa soon becomes less effective the longer the course of treatment is persisted; higher and higher levels of Levodopa and/or more frequent administration of the drug are required to reach a therapeutic effect. More specifically, increased doses of Levodopa are required to compensate for a continuous and increased loss of dopamine over time, which make Levodopa effective only momentarily rather than preventative towards the general progression of Parkinson’s [5]. Along with its limited ability in treating general Parkinson's progression, a side effect of Levodopa itself emerged as what is now called Levodopa-induced dyskinesia.
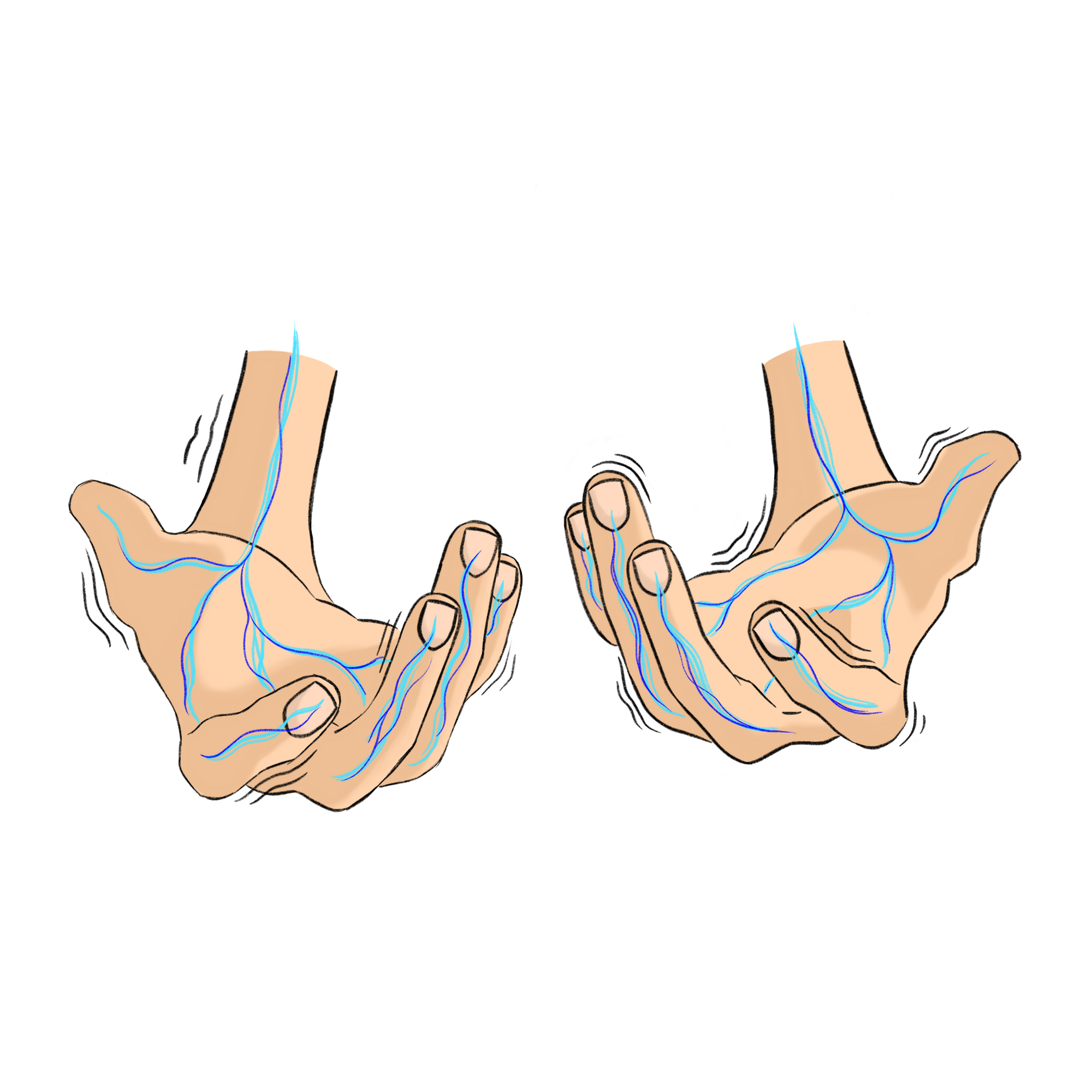
Dyskinesia is an involuntary, fluid, and “dance-like” jerk that many people mistake as a symptom of Parkinson’s disease itself [6]. Unlike Parkinson’s, dyskinesia is not typically centered around a specific joint. It can entail arm flailing, head bobbing, full-body squirming, and speech impairment simultaneously. To put it in simpler terms, people with Parkinson's have difficulty initiating movement, whereas people undergoing Levodopa-induced dyskinesia experience the opposite, with difficulty stopping their body movements. However, ongoing research on the use of sub-anesthetic ketamine-infused treatments has shown promising results in mitigating dyskinesia.
A 2016 meta-analysis detailed the possibility of subanesthetic ketamine infusion treatment in aiding involuntary movement from Levodopa medication through five separate case studies [7]. The patients involved in the analysis consisted of three females and two males, all above the age of 50 who had suffered from Parkinson's disease for over eight years each and for a combined total of 56 years. Subjects were provided with 0.15-0.3 mg/kg/hour microdoses of Ketamine for 50 to 96-hour periods with concurrent Levodopa treatment. Throughout the study, many physical differences were noticed in the patients who received Levodopa with ketamine infusions. There were substantial differences in pain level, reduced tremors, and long-term improvement of Levodopa-induced dyskinesia post-infusions in contrast to pre-ketamine administration. One case study subject who suffered lower back lumbar degenerative disk disease, a disease that is often exacerbated by dyskinesia, reported a dramatic decrease in his pain after ketamine infusion. In the best cases, patients were almost free of dyskinesia completely [7]. Drawing from the results of these case studies, it is evident that ketamine may provide instantaneous and long-term relief for Levodopa-induced dyskinesia and the painful side-effects associated with it. With that in mind, it is crucial to set aside the stigma surrounding ketamine in order to initiate innovative medical advancement for treating drug reactions like Levodopa-induced dyskinesia.
Ketamine for Tourette’s Syndrome
Tourette’s syndrome (TS) is a neurological disorder characterized by compulsive motor or vocal tics and/or compulsive behavior. These tics typically manifest in children from the ages of 2 to 15, and are notorious for their uncontrollable and repetitive head jerking, barking, kissing, obscene cussing, and even self-injurious behavior like self-hitting or slapping [8]. Although many people affected by TS have adapted and proudly accepted their condition, it's also worth noting that many feel the contrary. Patients who suffer from more advanced tics report them to be highly disruptive to their daily life, making TS a condition many urgently seek treatment for.
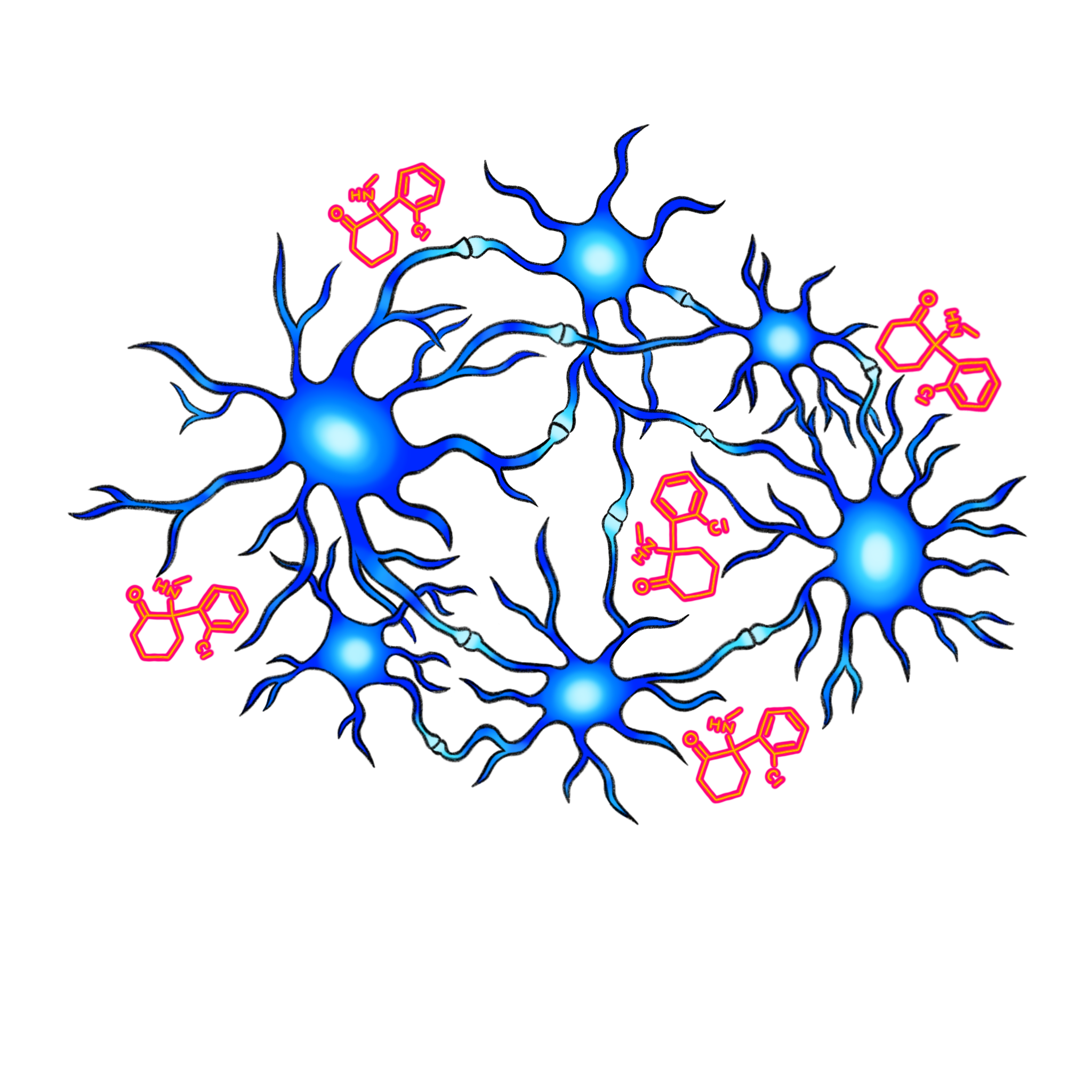
Although the pathology explaining the root cause of TS is unknown, what scientists can generally assume about it is the patterns of genetic mutation and abnormality associated with the condition. Researchers have connected TS and co-occurring similar disorders, such as autism, to a deletion in the 2p16.3 gene. This genetic mutation undermines the ability of neurons to communicate with each other and directly affects brain areas involved in TS. Individuals with the 2p16.3 deletion are over ten times more likely to develop autism and fifteen times more likely to develop TS than individuals without the mutation [10].
Ketamine, however, seems to ameliorate some of the adverse effects of the 2p16.3 deletion [9]. In a rodent study, 13 mice that possessed heterozygous NRXN1 exons, which are segments of DNA directly involved in the 2p16.3 deletion mutation, were administered subanesthetic doses of ketamine. C-2-Deoxyglucose functional brain imaging, a type of MRI that measures metabolism, was utilized to image the rodent subject’s brain activity after ketamine administration. Evidence uncovered from the scans supported that ketamine corrected thalamus connectivity within the brain of heterozygous NRXN1 rodents and overall increased connectivity within those regions in comparison to rodents who did not receive ketamine treatment. Researchers also found that ketamine partially improved the brain’s ability to communicate with itself and also decreased abnormal hyperactivity within the thalamus region of the brain [9]. With these results, researchers are now optimistic that ketamine will provide crucial insight to the treatment of disorders like TS that are associated with 2p16.3 deletion.
Ketamine for Mental Illnesses
Ketamine and psychedelic health don’t exclusively counter the effects of neurological diseases—they also show great potential in treating psychiatric disorders. A large portion of patients suffering from progressive neurological conditions report experiencing mental illnesses simultaneously, and it is worthwhile to explore the potential benefits of ketamine on diseases such as depression and PTSD.
Depression
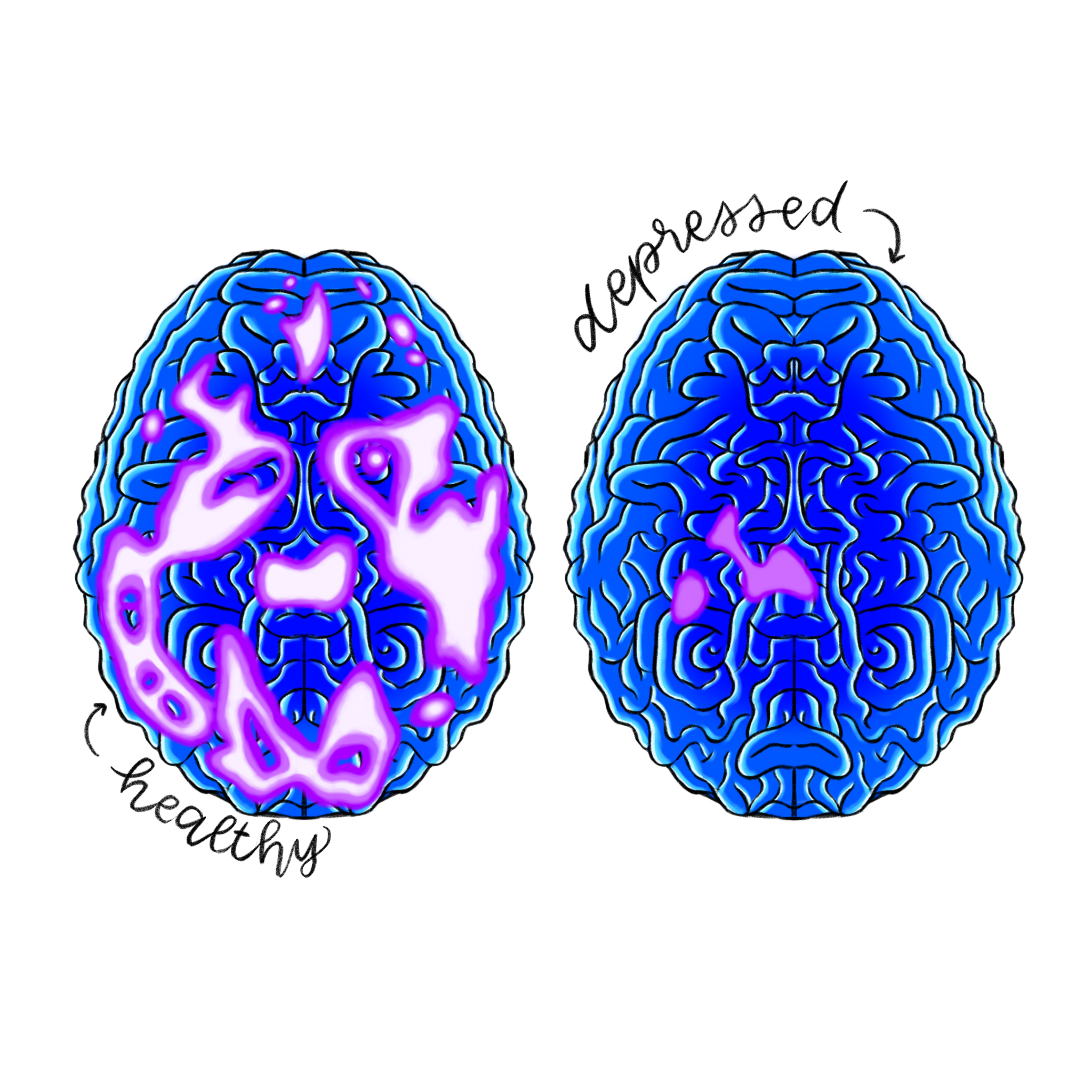
Clinical depression is characterized by feelings of helplessness, disinterest, isolation, and thoughts of suicide [11]. Typically, it is described as an imbalance of neurotransmitters and lowered brain activity within the amygdala, hippocampus, and the thalamic regions of the brain, which are associated with processing emotions, storing memories, and transmitting sensory information respectively. Although the condition is unseen to the human eye, people who suffer from clinical depression can display physical symptoms such as weight gain or loss. In severe cases where depression either coexists or acts as an outcome of physical illness, medical practitioners can draw a linear association between depression and chance of recovery from preexisting physical diseases or illness within the patient [12]. Currently, an FDA approved form of ketamine known as esketamine is being utilized as an effective method of nasal spray treatment for clinical depression. Esketamine’s chemical structure allows it to bind to NMDA glutamate receptors tightly, making it possess a higher potency and efficacy than standard ketamine [13]. The higher potency found in esketamine allows healthcare providers to administer it in lower doses with lower risks of side effects, which can include dissociation and lightheadedness.
Since its approval in 2019, esketamine usage has gained popularity amongst healthcare providers and patients for its ability to promote neural connections [13]. Along with its highly effective nature, the most impressive trait of esketamine is its ability to combat treatment-resistant depression, or TRD, which is a form of depression unresponsive to multiple doses of an array of antidepressants.
In an analysis on esketamine, 802 patients who reported TRD unresponsive to 2 to 8 antidepressant trials were administered intranasal esketamine [14]. These patients were treated for a month and then an additional 44 weeks of flexible, frequent dosing up to 84 mg of esketamine. At the end of the trials, researchers reported an 11% increase in remission rates, rising from 47.2% remission of TRD after the 1 month induction phase, to 58.2% remission of TRD at the end of the trial [14].
In another similar review, ketamine was studied as an option for combatting TRD within adults under the age of 65 [15]. Participating subjects who had experienced depressive episodes were administered intravenous ketamine in 0.5mg/kg doses over 40 minute time intervals two to three times a week. Before and after the trials, the Montgomery-Asberg Depression Rating Scale, or MADRS, a scale used to assess severity of depressive episodes in response to antidepressant medication, was utilized to quantify the effect of ketamine on participating subjects. The MADRS quantifies 10 symptoms of TRD symptoms on a rating scale of 0 to 6. The sum of the ratings acquired from the MADRS represents the level of severity of depression, meaning the higher the score, the more severe a patient’s depressive symptoms are. Scores that fall within 9-17 score categorize TRD as mild, 18- 34 scores are categorized as moderate, and scores that fall between 35-60 as severe. After the trial, results of the MADRS reported significant differences between patients who received single doses and those who received repeated doses of ketamine versus patients who received a placebo treatment. Results revealed a decline in the MADRS score amongst participants who received ketamine treatment in comparison to the control group [15]. These findings further support the idea that ketamine has a unique niche and future in psychiatric medicine.
PTSD
After witnessing a terrifying or traumatic event, partial recovery from trauma typically takes around three weeks while full recovery can take up to three months [16]. For some, however, recovery is never completely achieved. Post traumatic stress disorder (PTSD) is a psychiatric disorder in which a person who either witnesses or experiences a traumatic event suffers anxiety, heightened reactions, nightmares, and intrusive flashbacks long after the event. People who suffer from PTSD can even start feeling detached from those close to them. The condition is typically triggered by sensory stimuli which includes visuals, scents, sounds, or thoughts that are in some way associated with the traumatic event. The brain scan of a person suffering from PTSD can look significantly different from someone without the condition [17]. Activity within the amygdala, medial frontal cortex, and hippocampus regions of the brain, which are all responsible for fear response and decision-making, are heightened within people with PTSD during triggering stimuli [18]. Current treatments for this condition include trauma focused psychotherapy or an array of antidepressant medication. Zoloft, Paxil, Prozac, and Effexor are currently the most effective medications in treating PTSD but unfortunately, they are not always viable solutions to the symptoms [19].
In one review study, a survey sample of 41 patients who suffered from PTSD were administered 0.5mg/kg doses of ketamine to test the capabilities of the drug in comparison to midazolam, a common anesthetic [20]. Subjects had pre-existing, chronic PTSD and were unmedicated before the study. As the study was implemented through a randomized double-blind cross-over manner, subjects received both placebo and treatment consecutively, and neither researchers nor subjects knew which order treatment was administered until the trial ended. All 41 patients completed the first dose of ketamine infusion, while 29 of the 41 received an additional dose. Infusions were administered over a 40 minute time period, and patients were assessed 24 hours after intravenous infusion using a metric known as Impact of Event Scale-Revised (IES-R). This is the most widely known and used method of measuring event-induced distress, and it was utilized throughout the study to evaluate the effect of ketamine as a treatment for PTSD [21]. Data from the IES-R allowed researchers to conclude that subanesthetic intravenous ketamine treatment, compared to midazolam, was substantially more effective in reducing PTSD symptom severity. Although the symptoms of PTSD slowly recurred after 48 hours, 7 participants—17% of the sample size—exhibited long-term improvements in distress 2 weeks after ketamine treatment [20]. Many victims of PTSD have slipped through modern healthcare due to a lack of effective treatment plans. The integration of ketamine into current prescription treatment plans can support patients in ways that traditional PTSD medication alone cannot by providing patients with enhanced and instantaneous relief.
The findings of these studies on TRD and PTSD display promising data that not only provides solutions for their respective conditions, but also begs the question of ketamine’s potential in treating illnesses concurrently. Can we start treating comorbid psychiatric conditions, or conditions that occur within someone simultaneously, with the same drug? A recent study conducted and led by C.S. Albott in 2018 tested this theory alongside the efficacy and safety of intravenous ketamine infusions on 15 veteran subjects who had both PTSD and TRD [22]. After 0.5 mg/kg doses of intravenous ketamine, the drug had promoted rapid improvements in PTSD and TRD synchronously. The median relapse time for the 12 participants who experienced PTSD remission was 41 days. This favorable outcome pushes the limits of ketamine’s long-lasting effects even further, as the degree of efficacy of ketamine treatment on PTSD postulates the drug’s success in treating other chronic illnesses. With ketamine, we can start to postulate its potential in treating neurodegenerative and neurological diseases while treating psychiatric conditions concurrently.
Future Directions
It’s important to weigh the adverse effects of ketamine testing as well. Ketamine is classified as a schedule III substance by the United States Drug Enforcement Administration, meaning that it ranks as “moderate to low” in potential for dependency [23]. Although it is not considered by the DEA as addictive as schedule I and II drugs like marijuana or oxycontin, potential for ethical violations within medicinal research, especially psychedelics, is bound to emerge. Overdosing, addictive potential, and the possibility of ethics violation play a significant role in the methodical and procedural aspects of drug administration. In practice, misguided prescription of ketamine is especially relevant to younger patients, as these individuals experience an increased risk of suicidal thoughts and ideation when treated with ketamine. Dosage, frequency, and forms of administration need to be accounted for in order to reduce feelings of dissociation, nausea, or general discomfort. Despite its low potential for physical or psychological reliance, ketamine is still capable of misuse by patients. To responsibly handle and distribute ketamine, patients receiving treatment should be over the age of 25, display little-to-no indication of addictive personality, must be allowed an option for withdrawal from treatment at any time, and must be given treatment within a controlled environment [24]. Additionally, when testing ketamine’s efficacy on mouse models who possess the same 2p16.3 genetic mutation found within humans, it's important to note that rodents are not complete heuristics for the advancement of Tourette’s syndrome research, and are not entirely effective in modeling the human condition. Animal models can serve as a start for medicating treatment, but they only provide evidence that promotes the continuance of research for humans rather than definitive answers for human treatment.
The emergence of promising and widespread psychedelic healthcare within the medical field is limited until steps are taken to dismantle the preconceived notion that ketamine is strictly an illicit recreational substance. If we can break down the stigma surrounding psychedelic drugs within our society, ketamine will prove itself to be the catalyst of major medical breakthroughs within the medical field.
References
- Drug Enforcement Administration. “Ketamine - Dea.” Drug Enforcement Administration Admin, June 2020, admin.dea.gov/sites/default/files/2020-06/Ketamine-2020.pdf.
- Heitz, David. “Why Are the Brains of Teens and Young Adults so Prone to Addiction ...” Rolling Hills Hospital, 2016, rollinghillshospital.org/brains-teens-young-adults-prone-addiction-deadly-consequences/.
- National Institute of Health. “Parkinson’s Disease.” National Institute on Aging, U.S. Department of Health and Human Services, 2013, www.nia.nih.gov/health/parkinsons-disease.
- Lanciego, J.L., Luquin, N., Obeso, J.A. Functional neuroanatomy of the basal ganglia. Cold Spring Harb Perspect Med. 2012 Dec 1;2(12)009621. doi: 10.1101/cshperspect.a009621.
- Cleveland Clinic medical. “Dopamine Deficiency: Symptoms, Causes & Treatment.” Cleveland Clinic, 2022, my.clevelandclinic.org/health/articles/22588-dopamine-deficiency.
- Drug scheduling. DEA. (n.d.). Retrieved March 13, 2023, from https://www.dea.gov/drug-information/drug-scheduling
- Albott, C. S., Lim, K. O., Forbes, M. K., Erbes, C., Tye, S. J., Grabowski, J. G., Thuras, P., Batres-y-Carr, T. M., Wels, J., & Shiroma, P. R. (2018). Efficacy, safety, and durability of repeated ketamine infusions for comorbid posttraumatic stress disorder and treatment-resistant depression. The Journal of Clinical Psychiatry, 79(3). doi: 10.4088/jcp.17m11634
- Va.gov: Veterans Affairs. Impact of Event Scale - Revised (IES-R) for DSM-IV. (2018, September 24). Retrieved March 13, 2023, from https://www.ptsd.va.gov/professional/assessment/adult-sr/ies-r.asp
- Feder, A., Rutter, S. B., Schiller, D., & Charney, D. S. (2020). The emergence of ketamine as a novel treatment for posttraumatic stress disorder. Rapid Acting Antidepressants, 261–286. https://doi.org/10.1016/bs.apha.2020.05.004
- Mayo Clinic Staff. “Antidepressants: Selecting One That’s Right for You.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 23 Sept. 2022, www.mayoclinic.org/diseases-conditions/depression/in-depth/antidepressants/art-20046273%C2%A0.
- Bremner, J. D. (2006). Traumatic stress: Effects on the brain. Dialogues in clinical neuroscience. Retrieved March 13, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181836/#:~:text=Brain%20regions%20that%20are%20felt,amygdala%2C%20and%20medial%20prefrontal%20cortex.
- Mayo Foundation for Medical Education and Research. (2022, December 13). Post-traumatic stress disorder (PTSD). Mayo Clinic. Retrieved March 13, 2023, from https://www.mayoclinic.org/diseases-conditions/post-traumatic-stress-disorder/symptoms-causes/syc-20355967
- Phases of trauma recovery | UPMC HealthBeat. (n.d.). Retrieved March 13, 2023, from https://share.upmc.com/2019/08/phases-of-trauma-recovery-50ph/
- Bozymski, K. M., Crouse, E. L., Titus-Lay, E. N., Ott, C. A., Nofziger, J. L., & Kirkwood, C. K. (2019). Esketamine: A novel option for treatment-resistant depression. Annals of Pharmacotherapy, 54(6), 567–576. https://doi.org/10.1177/1060028019892644
- Swainson, J., Thomas, R. K., Archer, S., Chrenek, C., MacKay, M.-A., Baker, G., Dursun, S., Klassen, L. J., Chokka, P., & Demas, M. L. (2019). Esketamine for Treatment Resistant Depression. Expert Review of Neurotherapeutics, 19(10), 899–911. https://doi.org/10.1080/14737175.2019.1640604
- U.S. National Library of Medicine. (n.d.). Esketamine. National Center for Biotechnology Information. PubChem Compound Database. Retrieved March 13, 2023, from https://pubchem.ncbi.nlm.nih.gov/compound/Esketamine
- Gouin, J.-P., & Kiecolt-Glaser, J. K. (2011). The impact of psychological stress on wound healing: Methods and mechanisms. Immunology and Allergy Clinics of North America, 31(1), 81–93. https://doi.org/10.1016/j.iac.2010.09.010
- U.S. Department of Health and Human Services. (n.d.). Depression. National Institute of Mental Health. Retrieved March 13, 2023, from https://www.nimh.nih.gov/health/topics/depression
- Common genetic link between autism and Tourette's impairs brain communication. Lancaster University. (2019, December 10). Retrieved January 31, 2023, from https://www.lancaster.ac.uk/news/common-genetic-link-between-autism-and-tourettes-impairs-brain-communication
- B Hughes, R., Whittingham-Dowd, J., Simmons, R. E., Clapcote, S. J., Broughton, S. J., & Dawson, N. (2019). Ketamine restores thalamic-prefrontal cortex functional connectivity in a mouse model of neurodevelopmental disorder-associated 2p16.3 deletion. Cerebral Cortex, 30(4), 2358–2371. 9
- Mayo Foundation for Medical Education and Research. (2018, August 8). Tourette syndrome. Mayo Clinic. Retrieved March 13, 2023, from https://www.mayoclinic.org/diseases-conditions/tourette-syndrome/symptoms-causes/syc-20350465
- Sherman, S. J., Estevez, M., Magill, A. B., & Falk, T. (2016). Case reports showing a long-term effect of subanesthetic ketamine infusion in reducing l-dopa-induced dyskinesias. Case Reports in Neurology, 8(1), 53–58. https://doi.org/10.1159/000444278
- Chong S. Lee, MD, FRCPC. levodopa-induced dyskinesia: Mechanisms and management. BCMJ, vol. 43, no. 4, May, 2001, Page(S) 206-209 - clinical articles. -. Retrieved March 13, 2023, from https://bcmj.org/articles/levodopa-induced-dyskinesia-mechanisms-and-management#:~:text=Levodopa%2Dinduced%20dyskinesia%20refers%20to,dystonia%2C%20tic%2C%20or%20myoclonus.
- Fear of levodopa: Does it stop working? Parkinson's Therapeutics. (2018, April 22). Retrieved March 13, 2023, from https://parkinsons-therapeutics.org/fear-of-levodopa-does-it-stop-working/
