A fifty-year-old man with glioblastoma – one of the most invasive and aggressive types of brain cancer – had failed to find a treatment that worked for him; radiation, anti-tumor chemotherapy, and surgery showed no stable improvement [1]. Finally, doctors decided to perform an experimental procedure called CAR T-cell therapy, a form of treatment involving genetically altering the DNA of T cells and reinjecting those engineered cells back into the cancerous areas in his brain. The therapy had been successfully used to treat blood cancers in the past, but researchers hypothesized that the treatment could be altered to treat more invasive cancers; this case would be one of the first attempts to use the treatment on solid tumors through this specific approach [2]. This attempt was highly successful: every tumor the patient had regressed by 77-100%, the number of immune cells in his cerebrospinal fluid increased, suggesting that the injected cells were working correctly, and the patient experienced no major side effects throughout the entire process [1]. After exceeding all expectations, he was able to return to aspects of normal life. These results raised new questions about the experimental therapy’s success and its implications regarding cancer treatment in the future.
Cancer is one of the leading causes of death worldwide. Although it can take multiple forms, the disease always emerges through the same general pattern. Cancer stems from the dysfunction of the human body’s own cells – a rogue, random, spontaneous growth of cells that do not respond correctly to the body’s signals and gradually invade the entire body [3]. As technology advances over time, so does our understanding of the disease and our ability to treat it. Modern medicine offers many different means of treating cancer, like surgery and radiation, but certain types and locations of a patient’s cancer can make treatment more difficult. Moreover, the side effects from radiation and chemotherapy can be immensely painful and debilitating. Rather than attacking the body with foreign chemicals like most modern therapies, CAR T cell therapy takes the patient’s own blood cells to formulate a treatment that can be directly localized to the cancerous areas or injected into the patient’s bloodstream.
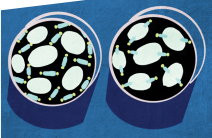
CAR T cell therapy uses chimeric antigen receptors (CARs), synthetic receptors that target specific surface molecules on cancerous cells and attack them by using the killing/cytotoxic capacity of T cells, a type of white blood cell that is responsible for recognizing and destroying infected or transformed cells in the body [2]. T cells remain in the body after their initial response to create longer lasting immunity against pathogens. The T cells are taken from the patient’s immune system and are altered by a process that takes approximately twenty-one days. First, the patient’s blood is broken down on a gradient after centrifugation to separate its red and white blood cells [1]. The isolated T cells are then infected with a virus that will express the CAR that is specific to the antigen expressed by the patient tumor. This virus will permanently alter the T cell DNA and enable the cells to recognize and attack cancerous cells instead of the infected cells they normally destroy in the body [2]. In the initial patient’s case, the T cells expressed a CAR that recognized a tumor-associated antigen interleukin-13 receptor alpha 2 (IL13Rα2), a gene highly expressed on glioblastoma cancer cells, which enabled the altered cells to attack his solid tumors [1]. The engineered T cells were injected directly into the patient’s tumors several times over the course of treatment and carefully assessed to see how the affected areas responded [1].
The success of this experimental treatment – an almost complete removal of brain tumors through genetically modifying immune cells in the patient’s body – supports CAR T cell therapy as a possible means of treating all types of cancer moving forward. But, although the initial attempt was more successful than expected, more attempts to treat cancer using this method must be performed before the process becomes regularly used in the field of medicine. Many aspects must be considered before it can become a leading form of cancer treatment. Manufacturing chimeric antigen receptors is highly intricate and expensive, and each cancer case requires specific care regarding the genes targeted by the reengineered receptors [1,2]. There is also no way to know if all forms of cancer would respond the same way to CAR T cell therapy; research accumulated from every attempt to treat blood cancer has shown that certain forms of leukemia are more susceptible to treatment than others [2]. Immune tolerance to self-antigens and the lack of guidelines to successfully locate the necessary target molecules are other significant barriers in providing more patients with this form of treatment. Currently, researchers are looking for other ways to alter the DNA of patients’ T cells for the expression of the CAR. The optimization will ultimately lead to a shorter and more efficient transformation of a patient’s T cells [2]. Regardless, the primary success fosters optimism that it may soon be possible to treat cancer without having to endure the unpleasant side effects of chemotherapy or radiation – or that we are steps closer to finding a cure.
References
1. Brown, C. E., Alizadeh, D., Starr, R., Weng, L., Wagner, J. R., Naranjo, A., ... &
Kurien, A. (2016). Regression of Glioblastoma after Chimeric Antigen Receptor
T-Cell Therapy. New England Journal of Medicine, 375(26), 2561-2569.
2. Maus, M.V., Grupp, S. A., Porter, D. L., & June, C. H. (2014). Antibody-modified T
cells: CARs take the front seat for hematologic malignancies. Blood, 123(17),
2625–2635. http://doi.org/10.1182/blood-2013-11-492231
3. Cooper, G.M. The Cell: A Molecular Approach. 2nd edition. Sunderland (MA): Sinauer
Associates; 2000. The Development and Causes of Cancer.
