When TV commercials sing the famous jingle, “Nausea, heartburn, indigestion, upset stomach, diarrhea,” Pepto Bismol fans rejoice. There’s an appreciation out there when multiple problems have a single solution. However, when we look at the suite of disorders for which selective seretonin reuptake inhibitors (SSRIs) are prescribed — depression, panic disorder, obsessive compulsive disorder, social anxiety disorder, and anorexia to name a few [1, 2] — there isn’t the same “Huzzah!” as for Pepto. Run “SSRI” through a YouTube search query and the results are peppered with scared and angry people declaring SSRIs to be dangerous, even going so far as to claim that they are a direct cause of homicidal behavior.
Wild speculation is, to some extent, understandable when we aren’t sure exactly how a psychoactive drug works, yet prescribe it for a number of common ailments. Relevant experts in pharmaceuticals and neuroscience are still not sure how exactly serotonin reuptake inhibition has a therapeutic effect for the disorders for which it’s prescribed. [1, 2, 5] Research is still trying to pin down the mechanism behind SSRIs that produce their varied long term effects. But an increasing number of studies are making headway by focusing on subtle, unconscious changes in attention that occur after short term SSRI use and precede noticeable changes in mood or voluntary behavior. Some of the most immediate observed effects of SSRIs are altered tendencies of visual fixation — like how one goes about reading a person’s face.
Selective Serotonin Reuptake Inhibitors (SSRIs) were marketed commercially for the first time in the early 80’s as a popular alternative to preexisting antidepressants, and are now among the most often prescribed therapeutic drugs.
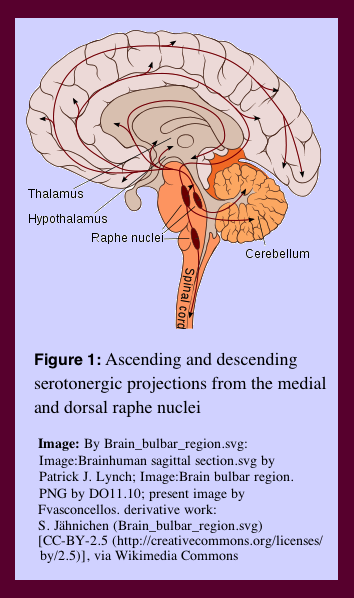
SSRIs prevent the reuptake of serotonin by presynaptic neurons thereby prolonging serotonin availability to post-synaptic receptors. This alters the level of activity of neurons in serotonergic pathways.
Looking in the Eye
This year, Simplicio et. al have published their research studying the short-term effects of SSRI drugs on facial exploration using eye tracking data. Eye tracking during the viewing of images has become a valuable technique for assessing behaviors associated with affective disorders and their treatments, allowing unique insight into attention and instantaneous reactions to stimuli. By holding the head still and recording gaze over an image, abnormal attentional biases have been identified in several affective disorders. [4] Various forms of neuroticism have been associated with avoidant viewing patterns of faces, leading Simplicio et. al to wonder how this avoidant behavior would be affected by SSRI use. [3]
Participants were screened for traits of high neuroticism, characterized by “a predisposition to negative affect and increased vulnerability to emotional disorders.” [3] These highly neurotic individuals were asked to look at series of pictures of faces during eye tracking to measure the areas and duration of attention paid to each face. Compared to participants rated as having low neuroticism, highly neurotic participants (High N’s) spent less time focused on the eyes and more focused on the mouth, and spent less time overall looking at the face. Within the High N population, those who maintained a longer gaze over the eyes rated fewer faces as having hostile characteristics, suggesting that increased focus on the eyes can lead to less anxious interpretations of facial expression. [3]
Half of the High N participants were given repeated regular dosage of Citalopram, an SSRI noted as being the most selective for serotonergic synapses, over seven days. The other half received a placebo. The Citalopram group increased both overall face scanning time and maintenance of gaze on the eyes for all facial expressions significantly more than the placebo. They also demonstrated a lower requirement of expression-intensity in order to correctly identify positive vs. negative emotions. Also notable, the Citalopram population did not lose their bias for the mouth region over the eye region, suggesting that the SSRI produces a nonspecific effect on facial gaze maintenance. These effects were seen without subjective reporting of mood change in either group. Simplicio et. al acknowledge that because participants were explicitly cued to respond to the faces, ability to compare their results to natural behavior is limited as the behavior may have been altered by task-driven strategy in a way that wouldn’t be seen in a natural setting. [3]
Simplicio et. al do speculate about how these results may be involved in the long term therapeutic effects of SSRIs. Though it’s too big of a jump to make with confidence, it’s possible that SSRIs make an intervention in the facial avoidance patterns associated with high neuroticism, and that these patterns could be partially causal to the persistent interpersonal difficulties characteristic of this group. If this small behavioral change allows for fewer misattributions of facial stimuli, the early effects of SSRI use could be crucial in disrupting a cycle of anxious symptoms. [3]
Participants in this study were selected for high neuroticism, thus limiting the ability for its implications to be applied in the grand scheme of SSRI administration. However, it does push research to explore the way that facial exploration is affected in more diverse populations. Working with a broader range of disorders, as well as more specific dimensions of neuroticism (for instance, including Low N’s), will get us closer to understanding SSRIs function in a way that will allow us to improve its use and to pacify a skeptical public. As progress is made in better understanding drug efficacy, a more trusting relationship can be developed between patients and providers.
Although, if it makes you feel any better, no one’s exactly sure why Pepto works either.
- Edwards JG. Selective serotonin reuptake inhibitors. BMJ. 1992;304:1644–1646. doi: 10.1136/bmj.304.6843.1644. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3651296/
- David J. Nutt, Sam Forshall, Caroline Bell, Ann Rich, John Sandford, Jon Nash, Spilios Argyropoulos, Mechanisms of action of selective serotonin reuptake inhibitors in the treatment of psychiatric disorders, European Neuropsychopharmacology, Volume 9, Supplement 3, July 1999, Pages S81-S86, ISSN 0924-977X, http://dx.doi.org/10.1016/S0924-977X(99)00030-9. http://www.sciencedirect.com/science/article/pii/S0924977X99000309
- Martina Di Simplicio, Sonia Doallo, Giulia Costoloni, Gustavo Rohenkohl, Anna C Nobre and Catherine J Harmer, ‘Can you look me in the face?’ Short-term SSRI Administration Reverts Avoidant Ocular Face Exploration in Subjects at Risk for Psychopathology, Neuropsychopharmacology advance online publication 13 August 2014; doi: 10.1038/npp.2014.159. http://www.nature.com/npp/journal/vaop/ncurrent/full/npp2014159a.html#bib14
- Armstrong T., Olatunji B. O. (2012). Eye tracking of attention in the affective disorders: a meta-analytic review and synthesis. Clin. Psychol. Rev. 32, 704–72310.1016/j.cpr.2012.09.004. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4172016/
- Meera Vaswani, Farzana Kadar Linda, Subramanyam Ramesh, Role of selective serotonin reuptake inhibitors in psychiatric disorders: a comprehensive review, Progress in Neuro-Psychopharmacology and Biological Psychiatry, Volume 27, Issue 1, February 2003, Pages 85-102, ISSN 0278-5846, http://dx.doi.org/10.1016/S0278-5846(02)00338-X. http://www.sciencedirect.com/science/article/pii/S027858460200338X