No child should grow up with the fear that the next breath they take in could be their last. Such extreme stress can affect the delicate developmental processes that take place early in life, and often has lifelong consequences. Between the ages of 2 and 16, the brain undergoes a period of rapid brain growth and development; neurons in the brain undergo axonal and dendritic elongation to create a vast, complex network. This neuronal growth largely follows the individual's genetic code, but it is also influenced by factors from the outside environment [1]. While the brain's response to external growth can certainly reinforce already established neural connections, it can also throw this intricate and delicate system off balance [1]. A 1980 case study of elementary school children done by JP Comer demonstrated that when a child does not receive enough positive attention (e.g. hugging, singing) from their parent, their self-image and self-esteem can suffer later in life. While children can still form other positive connections through social interactions, such interactions do not lead to the same outcomes as those formed by initial parent-child contact, and thus a parent's behavior can impact a child's development [2]. Another external factor that can impact a child's development is developmental inhibitors such as disorders like post-traumatic stress disorder (PTSD). PTSD is a psychological disorder that develops as a response to a traumatic or life threatening event, such as a natural disaster, a terrorist attack, or even a bank robbery [3]. PTSD can have debilitating effects on the developing brain, and is unfortunately quite prevalent in areas that experience constant violent conflict, such as the Gaza Strip [4].
PTSD and the Children of Gaza
In the year 2015, 800,000 children have a war zone to call home [5]. Since the creation of Israel in 1948, tensions between Israel and Palestine have resulted in thousands of civilian casualties for both countries. In recent years, the conflict has manifested itself in the Gaza Strip, the small area of land on the Mediterranean coast still controlled by Palestine. Currently, the conflict centers around trading sanctions placed on Gaza that limit its interactions with countries outside of Israel, as well as Palestine's claim that Israel possesses land that is rightfully Palestine's [6]. Survivors of the violence pay a brutal toll, particularly in the astounding number of children exposed to bloodshed in the area. Of a 2008 random sample of 240 children in the area, 58% had witnessed death, while 25% had experienced physical injury as a result of the conflict [4]. One consequence to these devastating conditions can be the manifestation of PTSD, a disorder that 61% of children in the area were diagnosed with in a separate random sample in 2009 [4].
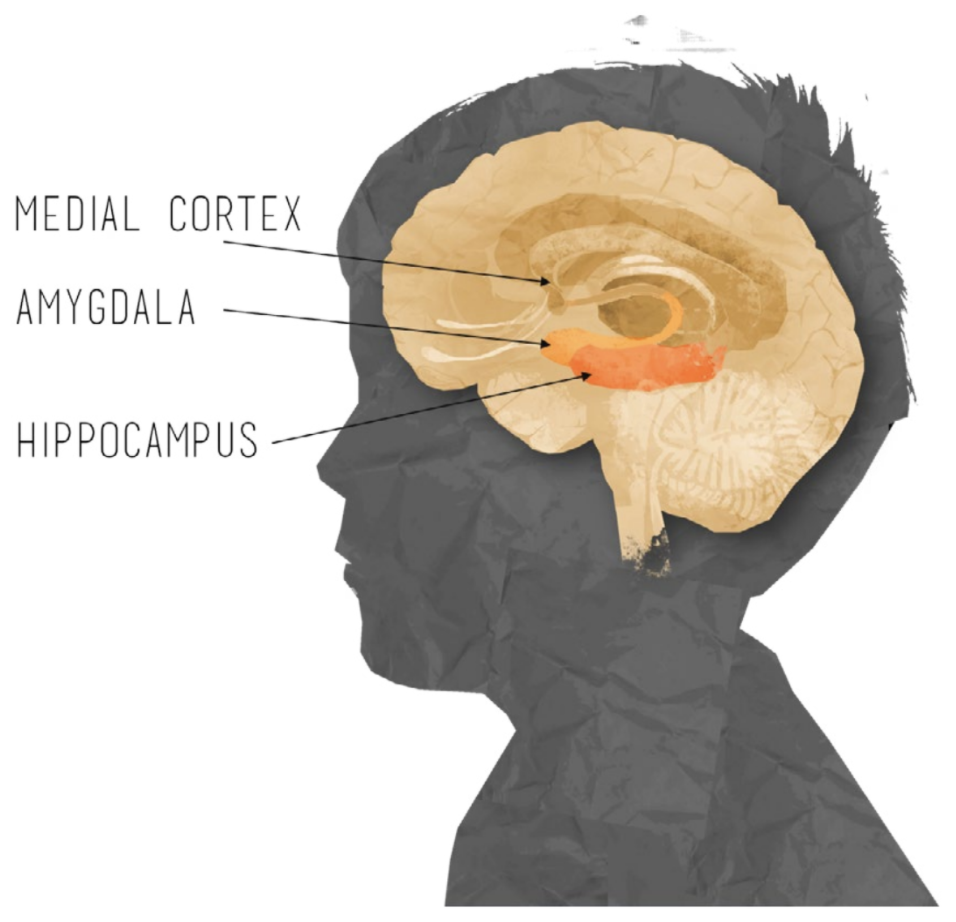
The symptoms of this disorder can be debilitating and include emotional upsetting flashbacks of the traumatic event, emotional detachment, and paranoia [7]. Each of these symptoms are correlated to changes in the size or activity in various regions in the brain, such as the hippocampus, the corpus callosum, and the amygdala [8]. These abnormalities are concerning, especially considering a study in which De Bellis et al. found brain volumes in patients with PTSD are correlated with the age at which the disorder was diagnosed [9]. In this study, researchers used Magnetic Resonance Imaging scans (MRIs) to examine the brains of 43 patients who had been diagnosed with PTSD. The MRI technique uses low-energy radio waves to picture internal organs, areas of the brain, and other internal structures. The study then analyzed the volumes of various sections of the brain in all 43 subjects [9]. Those who were diagnosed at an older age were found to have larger regional brain volumes that those who were diagnosed when they were younger. De Bellies et al. suggest that this could be because PTSD may impact the development of the brain, and thus the longer it goes untreated, the more seirous it becomes [9]. This study suggests that early identification and treatment of this disorder is imperative to minimize damage.
Effects of PTSD on the Brain
As the above study suggests, children diagnosed with PTSD in the Gaza strip may be experiencing physical changes to their brains as a result of the disorder. In an investigation at the University of Pittsburgh, a different study conducted by De Bellis et al. found that there was a decreased volume of the corpus callosum, the area that connects the right and left sides of the brain, in children who had been diagnosed with PTSD. By analyzing MRI scans of 44 children with PTSD and 61 without, he determined that those children diagnosed with PTSD displayed significantly lower volumes in this section of the brain [10]. While this study seems to suggest that damage to, or a decrease in volume, of the corpus callosum has a significant impact on an individual, other studies in the field seem to suggest the opposite-that damage to the corpus callosum may in fact not have a substantial impact on the individual. In fact, the complete severing of this region has been introduced as a treatment for epilepsy, and despite some slight problems with coordination, patients do not appear to have many adverse symptoms [11]. However a condition known as alexithymia, where patients struggle to recognize emotion in both themselves and others, appears to be correlated to a decrease in cerebral connectivity. In a 1999 study that compared 14 alexithymic patients, to 15 non-alexithymic patients, the control patients displayed much higher rates of information transfer between hemispheres [12]. Ultimately, a decrease in corpus callosal volume serves to limit cerebral connectivity, and while the study only suggests that this decrease may be correlated with alexithymia, speculation and further investigation are certainly warranted. Additionally, since patients with PTSD and alexithymia both struggle with emotional realization, the finding suggests a potential significance to the reduced volumes found in patients with PTSD.
Altered neural development due to PTSD can have profound impact on other areas of the brain, including the hippocampus, an area involved with long term memory storage and emotion regulation. A 2007 longitudinal study by Carrion et al. examined the impact of PTSD on hippocampal volumes; the study, which examined 15 children with PTSD, indicated with MRI scans that over the course of the year the volumes of the children's hippocampus decreased [13]. While the small sample size used makes it difficult to generalize these results, this finding provides evidence against the argument that hippocampal volume may make an individual more susceptible to PTSD. This study shows a correlation between decreased volume of the hippocampus and time with the disorder, which suggests that the disorder could directly affect the volume of this area of the brain [13]. Additionally, Carrion et al. found increased levels of cortisol, a hormone associated with stress, in the saliva of the children tested. Cortisol helps the body manage stress, but in high amounts it has been observed to kill hippocampal cells, thus suggesting that the stress caused by PTSD may be reducing the volume of the hippocampus. This creates a positive feedback cycle in the brain, in which reduced volume in the hippocampus causes the brain to produce more cortisol to deal with the stress of the reduction, which in turn causes further hippocampal cell death [13]. Such a reduction in hippocampal volume and an increase in cortisol levels can lead to severe depression and difficult regulating emotions, particularly in manifestation of PTSD [14].
Additionally, a 2001 study examined whether the hippocampus could be involved with other aspects of PTSD, including flashbacks [10]. This study, conducted by Osuch et al., used Cerebral Blood Flow imaging, a technology which shows blood flow in areas of the brain, to make inferences regarding the amount of activity in areas such as the hippocampus. In the study, eight participants with PTSD were read a script of their traumatic event while their brain activity was monitored with Cerebral Blood Flow imaging [15]. Each participant experienced flashbacks of the event, and simultaneously displayed an increase in blood flow to the hippocampus. The most intense flashbacks were correlated with greater blood flow in the hippocampal region [15]. These occurrences help to explain the neural basis of flashback symptoms that children with PTSD often experience.
The hippocampus is not the only area of the brain that seems to be affected by PTSD. PTSD has also been associated with an increase of activity in the amygdala, the small, almond-shaped area which manufactures emotional responses, including fear. This results in hypersensitivity of the amygdala and thus heightened fear reactions [8]. There is also evidence that PTSD may cause a decrease in activity in the medial prefrontal cortex, an area of the brain that regulates emotional responses. Shin et al. examined the medial prefrontal cortex's role in PTSD through a neuroimaging analysis of 17 war veterans with PTSD. In the study, subjects were presented with images or sounds that elicited a fear response. They found that veterans with PTSD experienced either limited activation or, in some cases, the absence of activation of the medial frontal cortex in comparison to control veterans without PTSD. Not only are these individuals facing increased activity in the amygdala, but the medial frontal cortex is also failing to regulate this activity, thus resulting in the symptoms of heightened fear response exhibited by those with PTSD [8].
Treating PTSD
PTSD can be, and in fact has been, successfully treated. Gaza, however, provides a unique situation in which ongoing conflict makes it even more challenging to treat patients. One of the most effective treatments for PTSD in children in the United States is cognitive behavioral therapy, or CBT [16]. CBT focuses on addressing the thought processes of patients and how these processes create patterns of behavior. Some forms of CBT attempt to change the way patients evaluate their thoughts, giving them skills to identify how their thoughts can relate to the destructive outcomes that plague their daily lives [16]. Evidence of the therapy's success is indicated in a study where, after 10 weeks of CBT, 92% of the 12 children participating were free of PTSD. These results also held up in a sex month follow up examination [17]. Unfortunately, CBT is an exhaustive process, which requires more time with a therapist than other treatments. This makes it a rather impractical method of treatment for the Gaza Strip, given that the World Health Organization reported 0.87 psychiatrists for every 100,000 people in the area [18].
Furthermore, studies that actually took place in the Gaza strip seem to challenge the previously-found success of CBT. A study by Diab et al. indicated that children who undergo CBT in Gaza as a treatment for PTSD did not show a statistical improvement in well-being based on a 5-point self-rated scale. While this study is certainly flawed-allowing the children to rank themselves is not necessarily reliable and well-being does not specifically test for symptoms of PTSD-the lack of improvement is still concerning. The researchers in this particular study concluded that the lack of improvement was due to the a lack of community support for the children involved [4]. Ultimately, the researchers claimed that similar to behavior observed in other oppressed regions, the children of Gaza are tied by a sense of responsibility to their communities. When these children experience a traumatic event, they feel completely hopeless; they are not only terrified for their own lives but irrationally blame themselves for events happening so close to home. Thus, the researchers concluded that in an attempt to counteract this, it's important to foster better familial interactions so that the children know they are not alone, thus taking the impossible burden of responsibility off of their shoulders and potentially opening them to the therapeutic processes [4]. However, a substantiated understanding of CBT's effectiveness in Gaza still remains unclear.
The insufficient number of psychiatric professionals in the Gaza Strip makes treatment methods like CBT or even simple counseling less plausible options for children of the area. While pharmacological (medication-based) treatments are another approach to treating the disorder that would require less footwork, there is currently little knowledge regarding possible medicinal treatments for PTSD in children. One class of medications that does seem to be effective for PTSD in adults is selective serotonin reuptake inhibitors (SSRIs). Serotonin is a neurotransmitter that helps stabilize mood, reduce levels of stress (cortisol), and reduce amygdala anxiety responses, and SSRIs increase levels of serotonin in the brain [20]. Unfortunately, the United States National Center for PTSD claims that pharmalogical agents generally fail to completely eliminate symptoms of the disorder, but do seem to minimize them, allowing for greater efficacy from other therapeutic approaches like CBT. This makes it a challenge to combat PTSD with pharmacological treatments alone. Some drugs, however, can be significantly helpful in ending the destructive neurological patterns that may take place in patients with PTSD. For example, the drug D-cycloserine (DCS), commonly used to help relieve neurologic pain, has been shown in preliminary studies to reduce cortisol levels substantially when used in conjunction with therapy [20]. While this could help reduce the emotional processing difficulties of PTSD as it would enable the hippocampus to develop unimpeded by cortisol, this reduction will most likely not help with other symptoms such as anxiety or emotional detachment, which are associated with other areas of the brain.
Hope in Peace
Despite the lack of a clear treatment method for children in Gaza, recovery from PTSD is certainly possible. A longitudinal study by Professors Abdelaziz Thabet (Al-Quds University) and Panos Vostanis (University of Leicester) examined the progress of children with PTSD in the Gaza Strip during a year of peace.
Thankfully, their results were extremely positive. Of the 102 children in the study who displayed symptoms of severe PTSD after the period of violence, 74 were no longer symptomatic [21]. This study suggests that perhaps children display a level of resilience that adults do not. It seems that children may be able to heal from the traumatic events that can cause PTSD if given the opportunity with the absence of further stress-inducing events. In fact, many cases of PTSD (in either children or adults) reach their most sever period of symptoms within a year of the trauma and then subside in intensity. However, not all individuals in the above study were completely relieved of their symptoms, and even many of those who experienced some recovery still faced significant mental health problems such as depression. This study also suggests that those who have already experienced war time trauma are more susceptible to PTSD later on if another trauma is presented [21]. The findings of this study do not mean that it is not necessary to treat the children suffering in Gaza; rather, it suggests that the children of the Strip are not lost causes, and do indeed have a chance for remission.
Unfortunately, peace has yet to come to Gaza, and it is unlikely that these children will have any chance to catch their breath in the years to come. It seems that they will probably face further traumatizing situations if they are lucky enough to survive the brutal environment they call home. PTSD will continue to plague the region's children until a drastic increase in the mental health resources of the area can take place. Such support is especially important considering that the children who have known only violence all their lives will soon be the ones influencing the course of their region. Unfortunately, Gaza has neither the resources nor the man-power to ensure that every child diagnosed with the disorder receives the necessary aid. These children do not deserve to live with the fear and stress their home brings with them: the world has a responsibility to ensure that the children of the Gaza Strip do not become a forgotten part of this blood conflict.
References
- Epstein, H. (2002, March 12). An Outline of the Role of Brain in Human Cognitive Development. Retrieved October 16, 2015, from http://www.sciencedirect.com/science/article/pii/S0278262600912533
- Fasfous, A., Peralta-Ramirez, I., & Perez-Gracia, M. (2013). Symptoms of PTSD among Children Living in War Zones in Same Cultural Context and Different Situations. Retrieved October 28, 2015, from http://quod.lib.umich.edu/j/jmmh/10381607.0007.203/--symptoms-of-ptsd-among-children-living-in-war-zones-in-same?rgn=main;view=fulltext
- Gaza Strip Demographics Profile 2014. (2015, June 30). Retrieved October 28, 2015, from http://www.indexmundi.com/gaza_strip/demographics_profile.html
- Diab, M., Peltonen, K., Quota, S., Palosaari, E., & Punamaki, R. (2014). Effectiveness of psychosocial intervention enhancing resilience among war-affected children and the moderating role of family factors. Retrieved October 28, 2015 from http://www.sciencedirect.com/science/article/pii/S0145213414004098
- Conger, K. (2007, March 7). Severe stress hurts children's brains, changes hippocampus, study shows. Retrieved October 28, 2015, from http://news.stanford.edu/news/2007/march7/med-carrion-030707.html
- Frodl, T., Schaub, A., Banac, S., Charypar, M., Jäger, M., Kümmler, P., . . . Meisenzahl, E. (2006, September, 31). Reduced hippocampal volume correlates with executive dysfunctioning in major depression. Retrieved October 28, 2015, from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1557684/
- Hamblen, J. (2007, May 22). PSTD in Children and Adolescents. Retrieved October 28, 2015, from http://www.isu.edu/irh/projects/better_todays/B2T2VirtualPacket/Trauma/PTSD in Children and Adolescents - (National Center for PTSD.pdf
- Kaminer, D., Seedat, S., & Stein, D. (2005, June 4). Post-traumatic stress disorder in children. Retrieved October 28, 2015, from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1414752/
- Shin, L., Raunch, S., & Pitman, R. (2006, July 26). Amygdala, Medial Prefrontal Cortex, and Hippocampal Function in PTSD. Retrieved October 28, 2015, from http://onlinelibrary.wiley.com/doi/10.1196/annals.1364.007/abstract
- Jefferys, M. (2015, August 17). Clinician's Guide to Medications for PTSD. Retrieved October 28, 2015, from http://www.ptsd.va.gov/professional/treatment/overview/clinicians-guide-to-medications-for-ptsd.asp
- Mental Health System in West Bank and Gaza. (2006). Retrieved October 28, 2015, from http://www.who.int/mental_health/evidence/west_bank_and_gaza_who_aims_report.pdf
- Hein, F., Qouta, S., Thabet, A., & Sarraj, E. (1993, April 24). Trauma and mental health of children in Gaza. Retrieved October 28, 2015, from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1677511/?page=2
- Kar, N. (2011, April 4). Cognitive behavioral therapy for the treatment of post-traumatic stress disorder: A review. Retrieved November 3, 2015, from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3083990/
- Thabet, A., & Vostanis, P. (2000, February 1). Post traumatic stress disorder reactions in children of war: A longitudinal study. Retrieved November 3, 2015, from http://www.sciencedirect.com/science/article/pii/S0145213414004098
- Kar, N. (2011, April 4). Cognitive behavioral therapy for the treatment of post-traumatic stress disorder: A review. Retrieved November 3, 2015, from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3083990/
- De Bellis, M., Keshavan, M., Clark, D., Casey, B., Giedd, J., Boring, A., . . . Ryan, N. (1999). Developmental Traumatology Part II: Brain Development. Retrieved November 3, 2015, from https://www.sacklerinstitute.org/cornell/people/bj.casey/publications/publications/DeBellis.1999.pdf
- De Bellis, M., Keshavan, M., Clark, D., Casey, B., Giedd, J., Boring, A., . . . Ryan, N. (1999). Developmental Traumatology Part II: Brain Development. Retrieved November 3, 2015, from https://www.sacklerinstitute.org/cornell/people/bj.casey/publications/publications/DeBellis.1999.pdf
- Cognitive Behavioral Therapy. (n.d.). Retrieved November 3, 2015, from http://www2.nami.org/Content/NavigationMenu/Inform_Yourself/About_Mental_Illness/About_Treatments_and_Supports/Cognitive_Behavioral_Therapy1.htm
- Smith, P., Yule, W., Perrin, S., Tranah, T., Dalgleish, T., & Clark. (2007, August 1). Cognitive-behavioral therapy for PTSD in children and adolescents: A preliminary randomized controlled trial. Retrieved November 3, 2015, from http://www.ncbi.nlm.nih.gov/pubmed/17667483
- Osuch, E., Benson, B., Geraci, M., Podell, D., Herscovitch, P., McCann, U., & Post, R. (2001). Regional cerebral blood flow correlated with flashback intensity in patients with posttraumatic stress disorder. Retrieved November 3, 2015 from http://www.ncbi.nlm.nih.gov/pubmed/11522258
