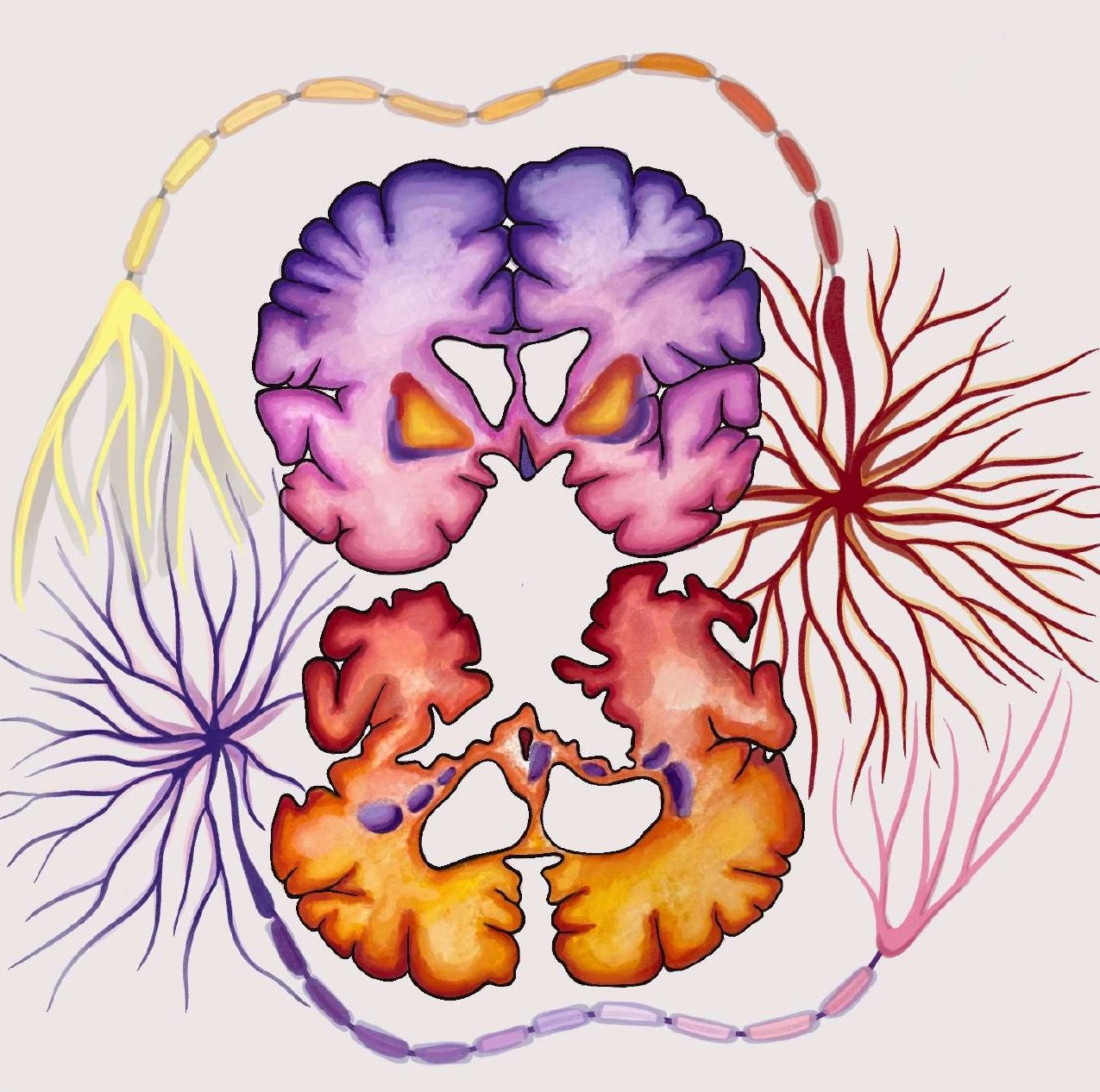
When discussing her grandmother’s and father’s diagnoses with Huntington’s Disease (HD), Kimberly Pryce described the testing process as “a flip of a coin. Heads, you’re facing a progressive, life-threatening brain disease that you can pass on to your kids. Tails, you’re OK” [1]. Pryce perfectly demonstrates how since HD is an inherited disease, diagnosis is not only devastating for the impacted individual but also for their family, as it indicates that siblings and offspring could be at risk. HD is a rare genetic disorder that causes the progressive breakdown of brain cells, historically attributed to the striatum of the brain [2]. The Huntingtin gene (HTT) is dominant, so if a parent has the disease, their children have a 50% chance of inheriting it. The frequency rate of HD is 6.52/100,000 persons in the United States alone, and while HD often develops in people between the ages of 30 and 40, onset can occur during childhood [3]. The condition leads to motor, cognitive, and psychiatric disturbances. One of the most characteristic symptoms is chorea, defined by involuntary movements that typically begin in the fingers, toes, and facial muscles but will spread to all parts of the body. Chorea is a result of only a few genetically determined disorders, therefore it is a strong indicator of HD. The disease is often comorbid with psychiatric symptoms including depression, anxiety, irritability, loss of interest, and passive behavior [4]. HD is detrimental to the quality of life of a person, and while some medications suppress certain symptoms, there is currently no cure. In this article, we will explore some breaking research and investigate three new potential treatment options as a result of these findings.
The Cause of Huntington’s Disease
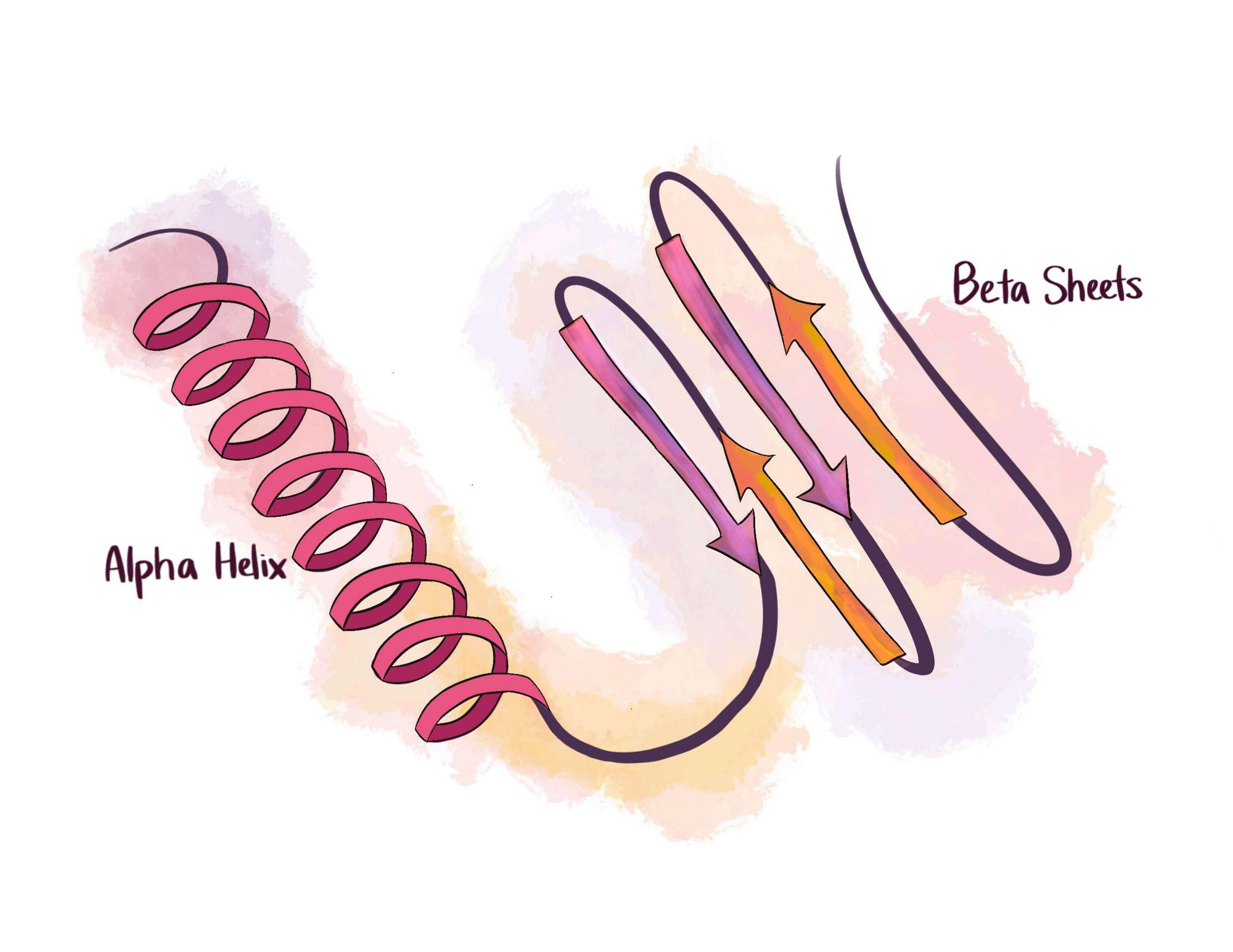
HD is caused by a gene mutation in HTT that codes for the protein Huntingtin. Genes are strands of DNA, which are made up of building blocks called nucleotides. There are four nucleotides – adenine (A), cytosine (C), guanine (G), and thymine (T). Sequences of DNA are later translated into proteins that are responsible for proper metabolic functioning. Huntingtin contains a triplet nucleotide, CAG, that repeats between 10 and 35 times normally [2]. Individuals with Huntington’s Disease, however, have a CAG nucleotide repetition of 36 or more times. The length of the CAG repeat is inversely related to the age of onset of symptoms. Thus, a person with 36-39 repetitions will likely have a late onset of HD between the ages of 60 and 80 years old, whereas an individual with over 80 repetitions will likely experience childhood onset [2]. The extra repetitions create an abnormally long protein called mutant Huntingtin, which misfolds and prevents proper functioning. Proteins are made up of amino acids that fold in specific configurations consisting of alpha-helices and beta sheets, crucial to their stability and function. When a protein misfolds, the amino acids form toxic clusters. Moreover, some mutant protein configurations catalyze the transition of normal proteins into toxic ones [5]. In HD, the mutant proteins alter calcium levels in cells and impair gene transcription. Eventually, the accumulation of proteins impairs a cell’s ability to carry out its function, causing cell death. Thus, the extra repetitions contribute to the symptoms of HD via the misfolding of important proteins.
The function of Huntingtin is not fully known, but it is clear that abnormalities in HTT have detrimental effects on a person's health. To better understand the role and function of Huntingtin, researchers examine its structure and behavior, allowing them to compare the mutant proteins to other harmful molecules. For example, it is hypothesized that mutant Huntingtin has properties similar to prions, infectious proteins that have the ability to induce abnormal folding and clustering [6]. Because of the similarities of prions to misfolded proteins, scientists can use them to better understand the pathology of neurodegenerative disorders like HD. Huntingtin mutant proteins are like prions because they are both found in extracellular spaces like cerebrospinal fluid and plasma, and they initiate the accumulation of malfunctioning proteins causing cell death [7]. In true prion diseases, mutant proteins are introduced to the body through oral and surgical routes as well as contaminated blood injection. Contrarily, in prion-like diseases, misfolded proteins form because of mutations and environmental factors. Researchers have suggested that mutant Huntingtin protein spreads via synapses, extracellular space, and biofluids, just like prions. Because of these prion-like properties, it is possible that HD can be targeted clinically with passive vaccination. For example, in a 2021 study, scientists focused on creating an antibody that would recognize cleavage sites on mutant Huntingtin [8]. These are the areas that enzymes cut for the purpose of accessing amino acids, breaking bonds, and activating dormant proteins. The antibody would assist enzymes in cutting the amino acid chain at the cleavage site to reduce the size of the mutant Huntingtin proteins and expedite their degradation. Preliminary findings of their study revealed lower levels of mutant Huntingtin in the plasma of a mouse model of HD [8]. While this study does not conclusively prove the effects of Huntingtin protein immunotherapies, it is a stepping stone in discovering a treatment for HD.
Purkinje Cells
Recent research regarding Huntington’s Disease also displays the importance of Purkinje cells in the brain. Purkinje cells are neural cells specific to the cerebellum, which is the part of the brain responsible for receiving information from the body and sending signals to the rest of the brain to enable proper coordination of movement [9]. Purkinje cells have many branch-like extensions called dendrites that receive impulses and send signals down the axon of the neuron. These cells are different from other neuronal cells in that they have larger, flatter, and more intricate branching, allowing them to process large quantities of information simultaneously. Through this branching, cells can remodel the dendrites when the brain learns.
One study revealed that Purkinje cell function was disrupted prior to Huntingtin accumulation [10]. In the past, HD was primarily attributed to neurodegeneration in the striatum, so this shift in understanding allows scientists to explore how other parts of the brain are impacted by the disease. Researchers used an HD mouse model and conducted a series of experiments over the course of four weeks. The first experiment consisted of training the mice on a computer-controlled treadmill for 60 seconds per trial. This test was done to measure how often the mice would fall during each trial to quantify their motor deficits. The second experiment involved placing the mice in a square field with infrared beams for one-minute intervals to determine total movement and distance crossed in the time allotted. At the end of the two experiments, the mice were euthanized so that their brain tissue could be analyzed before the presentation of typical HD symptoms. The results of these analyses showed that the total Purkinje cell count in the normal mice stayed consistent over the 12-week period, while in the HD mice, it decreased by 55%. Furthermore, the scientists found that a reduction in mouse motor function was correlated with decreased firing rate in Purkinje cells. They hypothesized that increased mutant Huntingtin in the cell caused their decreased firing [10]. Such cell loss in the cerebellum is uncommon, and combined with the Purkinje cell dysfunction, it suggests that the cerebellum plays an important role in the development of HD. This means that the Purkinje cells of HD patients may be related to the progression of their symptoms, and further studies can be done to determine how this information can be applied to the treatment of the disease.

In other developmental conditions such as Autism Spectrum Disorder (ASD), researchers are already looking at drugs to preserve the health and function of Purkinje cells. This suggests that such treatments could be possible for HD. A Purkinje cell deficit can be reversed through rapamycin, a type of drug used for preventing the rejection of organ transplants and for treating some types of cancerous tumors [11]. In a study at the Boston Children’s Hospital, pluripotent stem cells, capable of differentiating into many specialized cells, were collected from individuals who had tuberous sclerosis, epilepsy, or cortical tubers. The stem cell lines were reprogrammed into Purkinje cells and monitored for 24 days. The cells were then treated with mutations to model tuberous sclerosis, a genetic disease that causes benign tumors to grow in the brain, resulting in the loss of Purkinje cells. The stem cells were then treated for either 7 or 14 days with rapamycin. The study found that rapamycin treatment decreased the threshold of the membrane voltage needed to cause an action potential, meaning that the cells had higher excitability and reacted more easily. Rapamycin also increased the spontaneous activity of the cells and helped repair damaged synapses. These results suggest that rapamycin treatments could be used in treating diseases that cause deficits in Purkinje cells [11]. However, it’s important to keep in mind that this study had no subjects with HD; tuberous sclerosis is associated with a different protein than Huntington’s disease. Therefore, additional experiments would have to be conducted to determine whether the same treatment could work for HD patients. Nonetheless, the results of this study are encouraging because they demonstrate that cures could potentially be developed to preserve Purkinje cells. Localizing the cells that are involved in HD will allow scientists to learn which specific treatments will be most effective for curing the disease.
CRISPR-Cas9 Gene Editing
Another potential approach to HD treatment is gene editing, a method that could be used to alter the genes that cause mutant proteins. One gene editing tool used in microbiology is modeled on the defense mechanism of bacterial cells against a virus [12]. The bacterial host cell incorporates a part of the viral DNA into its own genome so that the bacteria can effectively recognize the virus in the future. This natural system of gene editing has been studied by researchers to incorporate or cut out selected DNA fragments into research subjects. This is called the CRISPR-Cas9 system because it relies on sections of DNA called Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR), and on the enzyme Cas-9. CRISPR sequences are transcribed into RNA molecules that guide Cas-9 to a specific target sequence of DNA. The enzyme acts like scissors; it cuts a part of DNA to allow for editing of the gene. CRISPR-Cas9 editing can be done in one of three ways: it can be used to disrupt and inactivate a gene, to delete a chunk of DNA, or to correct a gene by insertion of new nucleotides. CRISPR-Cas9 gene editing is very powerful and may be effective in not only suppressing HD symptoms, but also eliminating the mutant proteins altogether.

In a 2017 study, CRISPR-Cas9 gene editing successfully decreased neurotoxicity in a mouse model of HD [13]. Mice are a good model for HD because they demonstrate motor and behavioral dysfunctions similar to those seen in humans. In the study, regular HTT genes in mice were replaced with 140 CAG repeats from human Huntingtin DNA, causing the mice to express HD. Researchers designed a guide RNA (gRNA) molecule to target DNA regions coding for Huntingtin. Half of the mice were treated with gRNA, while the other mice served as the control group. Levels of the proteins were calculated in the striatum of the mice, which is a region of the brain associated with the preparation, initiation, and execution of movements. Since mutant Huntingtin forms clusters that alter movement abilities, measuring protein levels in the striatum indicates how well the gRNA reduces motor deficits. The mice that were injected with the virus and the guide RNA showed significantly lower accumulations of the mutant proteins [13]. Therefore, using CRISPR-Cas9 editing could decrease the expression of Huntingtin in HD patients, which may slow the onset of symptoms.
Another study conducted in 2019 further revealed the benefits of CRISPR-Cas9 gene editing in relation to HD [14]. This study demonstrated that gene editing increases the lifespan while decreasing motor deficits in a mouse model of HD. Researchers disrupted the expression of Huntingtin by designing gRNA to target the section of DNA that comes before the CAG repeats. The purpose of this was to trigger the Cas9 enzyme to cut the DNA strand before the repeat sequences were made into protein, thereby preventing the overproduction of Huntingtin. Similarly to the previous experiment, the mice were injected with an adeno-associated virus, which was used to insert the gRNA for the experimental group, while the control group received only a virus. Motor function was measured on a weekly basis; the mice injected with the guide RNA had a 15% increase in survival when compared to the control mice. In a disease with no cure like HD, even a small margin of survival increase is promising, especially in light of ongoing research that could raise this percentage in the future. However, it is noteworthy that the weight of the mice was the same for the experimental and control groups, which could pose a limitation to the study because weight loss is a strong indicator of disease onset [14]. One possible explanation for the constant weight is that the injections of the virus were done too long after mutant Huntingtin had already started forming, so further testing is necessary to fully understand the impact of the guide RNA on the lifespan of mice.
Further Implications and Conclusion
Approaching Huntington’s Disease from the angles of prion similarities, Purkinje cells, and gene editing are all innovative methods with the potential to cure a disease that impacts so many. These studies have demonstrated that it is possible to significantly decrease the number of mutant Huntingtin proteins, and an effective and sustainable cure may be on the horizon. Yet, these approaches don’t come without limitations. Prions have their own properties that don’t apply to HD and could generate misleading results. Adapting cures to Purkinje cells when HD has been historically thought to originate predominantly in the striatum implies a significant change in the biomedical understanding of HD, which needs to be tested further before strong conclusions are made. Additionally, the gene editing approach in particular creates wide debate due to certain bioethical issues that must be taken into consideration when considering CRISPR-Cas9 for HD. The most controversial usage of CRISPR-Cas9 is the replacement of DNA in human embryos [15]. This is because altering the genes of a zygote may lead to side effects that won’t be known until birth. Since it is unclear what the HTT gene does, editing it could result in many unknown secondary symptoms. It is also argued that altering genes to create a “normal” child detracts from their dignity as a human being and shouldn’t be done until the individual is old enough to make an informed decision and consent to gene editing [15]. Lastly, there is also the issue of safety. Researchers are still discovering which cells are impacted by HD, as discussed with the studies on Purkinje cells. Potentially, editing could be dangerous because it could cause mosaicism, where some cells carry out the edits but others do not, which can be harmful to the brain and other organs.
Regardless of these obstacles, it is evident that gene editing has the potential for curing HD, especially if it is combined with the recent developments in Purkinje cell and prion research. On top of that, there are many other diseases that could be treated with similar approaches, such as hereditary blindness, cystic fibrosis, and muscular dystrophy. These studies offer hope for those struggling with all kinds of genetic disorders, as they demonstrate how molecular biology and technology can work together to improve the lives of millions.
References
- Huntington’s Disease: The Pryce Sisters’ Story. (n.d.). https://www.hopkinsmedicine.org/psychiatry/patient_information/patient-stories/huntingtons-disease-the-pryce-sisters-story
- Nopoulos, P. C. (2016). Huntington disease: a single-gene degenerative disorder of the striatum. Dialogues in Clinical Neuroscience, 18(1), 91-98. doi: 10.31887/DCNS.2016
- Bruzelius, E., Scarpa, J., Zhao, Y., Basu, S., Faghmous, J. H., Baum, A. (2019). Huntington’s Disease in the United States: Variation by demographic and socioeconomic factors. Movement Disorders, 34(6), 858-865. doi: 10.1002/mds.27653
- Roos, R.A.C. (2010). Huntington’s disease: a clinical review. Orphanet Journal of Rare Diseases, 5(40). doi: 10.1186/1750-1172-5-40
- Reynaud, E. (2010). Protein Misfolding and Degenerative Diseases. Nature. 3(9), 28. nature.com/scitable/topicpage/protein-misfolding-and-degenerative-diseases-14434929/
- Alpaugh, M., Denis, H. L., Cicchetti, F. (2022). Prion-like properties of the mutant huntingtin protein in living organisms: the evidence and the relevance. Molecular Psychiatry, 27(1), 269-280. doi: 10.1038/s41380-021-01350-4
- Pearce, M. M. P., Kopito, R. R. (2018). Prion-Like Characteristics of Polyglutamine-Containing Proteins. Cold Spring Harbor Perspectives in Medicine, 8(2). doi: 10.1101/cshperspect.a024257
- Bartl, S., Xie, Y., Potluri, N., Gordon, B., Willenberg, A., Balash, K., Oueslati, A., Parth, M., Salhat, N., Siddu, A., Smrzka, O., Cicchetti, F., Straffler G., Hayden, M. R., Southwell, A. L. (2021). In vivo mtHTT protein reduction in the CNS and periphery by passive immunization with the monoclonal antibody C6-17. Journal of Neurology, Neurosurgery, & Psychiatry, 92(51). doi: 10.1136/jnnp-2021-EHDN.123
- Paul, M. S., Limaiem, F. (2022). Histology, Purkinje Cells. StatPearls. www.ncbi.nlm.nih.gov/books/NBK545154/
- Dougherty, S. E., Reeves, J. L., Lucas, E. K., Gamble, K. L., Lesort, M., Cowell, R. M. (2012). Disruption of Purkinje cell function prior to huntingtin accumulation and cell loss in an animal model of Huntington Disease. Experimental Neurology, 236(1), 171-178. doi: 10.1016/j.expneurol.2012.04.015
- Sundberg, M., Tochitsky, I., Buchholz, D. E., Winden, K., Kujala, V., Kapur, K., Cataltepe, D., Turner, D., Han, M., Woolf, C. J., Hatten, M. E., Sahin, M. (2018). Purkinje cells derived from TSC patients display hypoexcitability and synaptic deficits associated with reduced FMRP levels and reversed by rapamycin. Molecular Psychiatry, 23(11), 2167-2183. doi: 10.1038/s41380-018-0018-4
- Asmamaw, M., Zawdie , B. (2021). Mechanism and Applications of CRISPR/Cas-9-Mediated Genome Editing. Biologics, 15. 353-361. doi: 10.2147/BTT.S326422
- Yang, S., Chang, R., Yang, H., Zhao, T., Hong, Y., Kong., Sun, X., Qin, Z., Jin, P., Li, S., Li, X. (2017). CRISPR/Cas9-mediated gene editing ameliorates neurotoxicity in mouse model of Huntington’s disease. (2017). Journal of Clinical Investigation, 127(7), 2719-2724. doi: 10.2147/BTT.S326422
- Ekman, F., Ojala, D. S., Adil, M. M., Lopez, P. A., Schaffer, D. V., Gaj, T. (2019). Crispr-Cas9-Mediated Genome Editing Increases Lifespan and Improves Motor Deficits in a Huntington’s Disease Mouse Model. Molecular Therapy, 17(72), 829-839. doi: 10.1016/j.omtn.2019.07.009
- Ayanoglu, F. B., Elcin, A. E., Elcin, Y. M. (2020). Bioethical issues in genome editing by CRISPR-Cas9 technology. Turkish Journal of Biology, 44(2), 110-120. doi: 10.3906/biy-1912-52