Introduction
Medications have long been one of mankind's best ways of treating diseases. Imagine you are feeling nauseous, so you go to a doctor and they prescribe you some medication. You take it, and within hours you start feeling better. You might think, “wow that medicine worked great!” What if I told you that the medicine was not an anti-nausea treatment at all, but rather Ipecac, a medication that induces vomiting? But wait, you might be wondering, how could a medication that causes nausea cure the exact same condition? This paradox was studied by Stewart Wolf from Cornell University Medical College in 1950 [1]. Much like in our hypothetical situation, in his study, Wolf gave a nauseous patient Ipecac and told them it would alleviate their symptoms. Soon after taking the medication, the patient felt better, and all symptoms of their nausea vanished [1].
The results of the study were due to a phenomenon known as the placebo effect. The placebo effect occurs when rather than the treatment itself, the expectations around receiving a treatment cause beneficial effects [2]. When people are given a treatment, such as a pill, the context of receiving a medical treatment can lead to an alleviation of symptoms, even if the pill was just a sugar pill [2]. The placebo effect influences the treatment of many conditions, including mental health illnesses such as one of the clinical forms of depression, major depressive disorder (MDD). MDD is a chronic mental disorder which disrupts typical social or occupational functioning [3]. Common symptoms of MDD include loss of interest in pleasurable activities, changes in sleep patterns and appetite, fatigue, feelings of worthlessness, and suicidal ideation. MDD is characterized by having recurring episodes of symptoms, with each episode lasting more than 2 weeks [3]. Since about 20.6% of people in the US have had MDD during the course of their lifetime, developing effective treatment methods is critical [4]. In order to test the effectiveness of a new antidepressant treatment, studies need to know how much the medication itself alleviates depressive symptoms, but because the placebo effect can also alleviate these symptoms, this can be challenging to determine.
Depression and Antidepressants
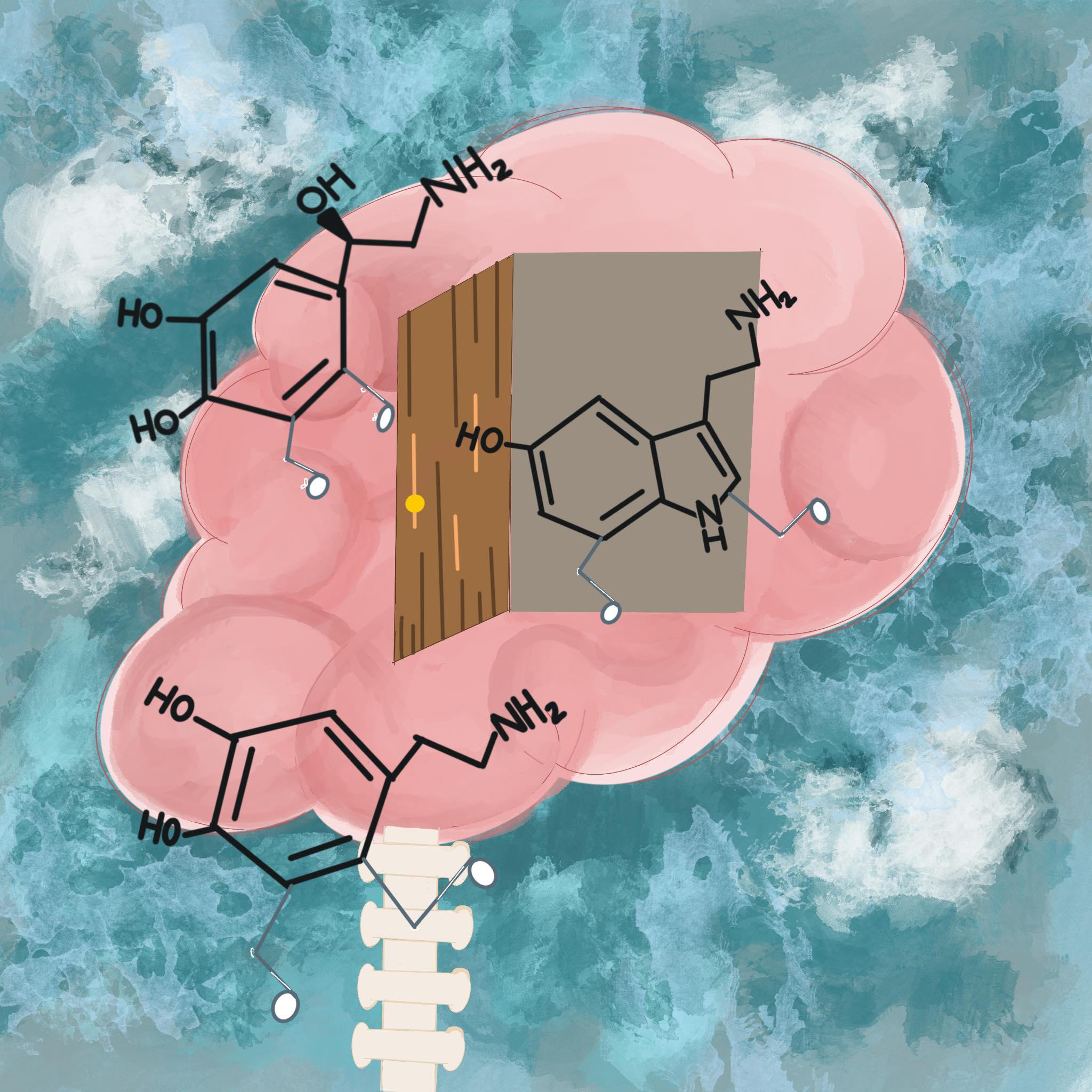
Antidepressant development is a field that has been expanding, particularly as more research is conducted in trying to understand the underlying neurological causes for MDD. Much is still unknown about what causes MDD, but many changes in neuronal functioning have been associated with the disorder. One of the changes observed in patients diagnosed with MDD is low concentrations of serotonin, norepinephrine, and/or dopamine [3]. These chemicals are known as monoamine neurotransmitters: molecules essential for many functions of the brain including neural signaling as well as regulating mood, circulation, and attention [3][5]. Many commonly prescribed classes of antidepressants try to increase the concentration of these neurotransmitters [3]. These classes of medication include: Selective Serotonin Reuptake Inhibitors (SSRIs), Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs), Monoamine Oxidase (MAO) inhibitors, and tricyclic antidepressants [3]. Each of these classes differ in how and which monoamine neurotransmitters they target.
While these antidepressants treat this deficiency in monoamine neurotransmitters, some patients who take them do not experience any remission of depressive symptoms [3]. One possible explanation for this is that the decreased concentration of monoamine neurotransmitters is not a direct cause of MDD. This is supported by results showing that lowering the concentrations of monoamine neurotransmitters in people without MDD does not cause them to develop depressive symptoms [3][6]. Additionally, when monoamine neurotransmitter concentrations are lowered in unmedicated patients with MDD, their symptoms do not worsen [3][7]. Because these antidepressants targeted at monoamine neurotransmitters are an effective treatment for some patients, they are still used today. However, since these treatments are ineffective for a significant portion of MDD patients, there is a need for antidepressants which target different biological mechanisms involved in depression [3].
Additional symptoms that have been connected to MDD that could be a target for antidepressant drugs include irregular levels of glutamate as well as increased activity in the inflammatory immune response [8]. Glutamate is a major neurotransmitter which contributes to over half of all chemical messages in the brain [3]. Glutamate is produced through a cyclic process in which glutamate and glutamine, an amino acid, are exchanged [3][9]. Studies have indicated that patients with MDD have irregular levels of glutamate/glutamine exchange happening within many areas of the brain [3]. For example, it has been found that in patients with MDD there are decreased levels of glutamate/glutamine exchange occurring within the hippocampus, which is involved in regulating memories [3] [10]. Within patients with MDD, decreased levels of glutamate/glutamine exchange have also been found within the anterior cingulate cortex, which is associated with regulating emotions and memory [3][11][12]. Many antidepressants are currently being developed that aim to affect the glutamate/glutamine cycle [3]. Furthermore, there has been a growing amount of research connecting increases in inflammatory immune responses to MDD [13]. As a result, the use of anti-inflammatory treatments in treating depression is a growing research area [8].
The Placebo Effect
Two main theories about the mechanisms of the placebo effect are known as the expectancy theory and classical conditioning. These theories are both believed to contribute to the placebo effect seen in antidepressant clinical trials [14]. According to the expectancy theory, treatments create a conscious expectation in the patient about how the treatment will affect them, and as a result, the patient’s symptoms improve [14]. Because people will often associate medical treatment with their symptoms improving, people expect that improvement is the most likely outcome after having a treatment. As a result of someone expecting their symptoms to improve with treatment, the act of taking a sugar pill can make that expectation a reality.
Classical conditioning attributes the improvement in symptoms to unconscious learning processes in patients caused by their association of certain stimuli with symptom improvement [14]. Influencing factors such as seeing a doctor’s white coat, having a good relationship with the doctor, and being told that the treatment will help all serve as cues to the brain that symptoms are going to be alleviated [2]. How the brain interprets these signals is similar to how it connects sight to context, memory, and decision making. The process by which the brain interprets contextual information involves many complex neural systems. The hippocampus is responsible for processing and storing memories as well as understanding contextual information. The lateral orbitofrontal cortex is responsible for creating an expectation of what the result of events will be. Integrating all of these signals is done by the ventromedial prefrontal cortex. These parts of the brain work together to allow people to connect what they are currently perceiving to what they have experienced previously and predict what might happen in the future. Research is still being conducted to determine the neural basis of the placebo effect as well as how neural responses caused by the placebo effect differ depending on what is being treated, such as using a placebo to treat pain versus using a placebo to treat MDD. In the case of when patients used placebos with the expectation that the placebo would alleviate pain, reduced pain-related activity occurred in the areas of the brain associated with pain response, such as the dorsal anterior cingulate cortex [2][15]. In patients with Parkinson’s Disease receiving a placebo, an increased release of dopamine was found within the striatum, an area of the brain associated with movement control and rewards processing [16][17]. In regards to the treatment of MDD, much is still unknown about how the placebo effect can improve symptoms and what areas of the brain it would affect to do so.

Antidepressant Clinical Trials
Clinical trials are studies which evaluate the effects of medications or other health-related treatments on people. Most antidepressant clinical trials compare the extent to which depression symptoms improve in one treatment group receiving the antidepressant with the improvement in another group receiving a placebo (a medication which has no active ingredients in it). In antidepressant clinical trials, the placebo rate of improvement has often been close to the antidepressant rate of improvement [14]. In a study conducted in 2016, Dr. Papakostas from Harvard Medical School and his team evaluated the results of 196 placebo-controlled antidepressant clinical trials of MDD. They recorded the response rate of the studies, where the response rate was determined as being the percentage of patients that had a 50% or greater reduction in depressive symptoms as defined by a depression rating scale [18]. They found that the response rate for the antidepressant trials they studied was 52.7% and the response rate for the placebo trials was 37.5% [18]. In order to determine more about the effectiveness of commonly used antidepressants, Dr. Ciprini and her team from the University of Oxford conducted a study which evaluated the results of 522 antidepressant clinical trials examining 21 total antidepressants [19]. They found that all of the antidepressants were more effective than the placebos [19]. While the antidepressants proved more effective than the placebos in Dr. Ciprini’s study, the placebo effect is still very prominent in antidepressant clinical trials. Dr. Irving Kirsch from Harvard Medical School conducted a meta-analysis on multiple antidepressant clinical trials and concluded that about 82% of the improvement observed in patients receiving antidepressant medications was also observed in the patients receiving a placebo [20].
Factors Influencing Clinical Trials
The strength of the placebo effect in antidepressant clinical trials has led to questions about the different factors that affect the results of antidepressant clinical trials. These factors can include clinical trial length, patient expectations, and even the physical appearance of the patients [21][22][23]. Dr. Fenghua Li and his team from the Yale University School of Medicine examined the relationship between trial circumstances and the extent of the placebo effect [21]. They found that in antidepressant medications studies, having a longer study length was associated with smaller placebo symptom improvement. This may imply that the placebo effect is larger in early stages of studies and then decreases as the study continues. Moreover, Dr. Li’s study found that conducting a study in more locations and having larger sample sizes are associated with having a larger placebo symptom improvement. This may be due to how these factors allow for less control over the procedures in conducting the study [21].
In addition, a patient’s prior history with medical treatments may affect how much of a placebo effect they experience [24]. If a patient has had good experiences with medical treatments in the past, then the strength of their placebo effect may be high due to their positive expectations for the treatment. Alternatively, if a patient has had bad experiences with medical treatments in the past, then the strength of their placebo effect may be low due to their negative expectations for the treatment. Having negative associations with treatments can additionally lead to nocebo effects, where a patient’s negative expectations lead to the occurrence of adverse events in which their condition worsens [24][14]. In addition, patient expectations of clinical trials can also be affected by the chance of receiving a placebo [22]. For example, a 100% chance of receiving an antidepressant can lead to more positive expectations in patients than a 50% chance of receiving a placebo [22]. It is believed that placebo effects and medication effects can have an additive relationship where the placebo effect plus the medication effect results in the overall change in symptoms, although the exact relationship between placebo effects and medication effects is still being researched [24][14]. As a result, differences in expectations for a treatment can affect how much the symptoms of patients improve when they take antidepressants [22][25]. This can make it difficult to determine the effectiveness of antidepressants when measuring symptom improvement in studies.
Another reason why the placebo group and antidepressant group have close response rates may be due to challenges in gathering an accurate reflection of how severe each patient’s depression is. The most common system used to try to quantify the severity of a person’s depression is called the Hamilton depression rating scale [14]. This scale associates scores with the core symptoms of MDD, with people with more drastic symptoms scoring higher numbers. One issue with this scale is that if an antidepressant improves things such as sleep, agitation, and appetite, but not the underlying depression, then it can appear, using this scale, that their depression did improve, when in fact it did not [14].
Additionally, sometimes other factors can affect how a clinician perceives the severity of depression. Dr. Hélèna Delmas and her team from the Centre Hospitalier Guillaume Régnier, France conducted a study in which they had psychiatrists rate the severity of the patient’s depression in normal clothes as well as when the patients were wearing blue pajamas, which are associated with staying in French psychiatric hospitals [23]. The study found that psychiatrists rated the patients' depression as being more severe when they were wearing blue pajamas compared to regular clothes [23]. This showed that subtle changes in the circumstances of patients, such as their appearance, can affect how their depression is scored. With all these outside factors influencing how a patient’s depression is scored in antidepressant clinical trials, researchers must go to greater lengths to keep studies unbiased to assess the real difference between the effect of antidepressants and the effect of placebos.
Conclusion
MDD is a global issue which affects more than 264 million people worldwide [26]. For this reason, gaining a better understanding of the overall causes and mechanisms of MDD is a critical area of research. Additionally, because many patients do not respond to current commonly used antidepressants, the development of new kinds of antidepressants is needed. Recently, a form of the drug ketamine was approved by the FDA for the treatment of depression [27]. Ketamine is used to treat glutamate dysregulation, as opposed to many currently used antidepressants which treat deficiencies in monoamine neurotransmitters. This makes ketamine a promising treatment for patients who have not improved after taking other antidepressants [27]. In order for new antidepressants, including ketamine, to be approved by the FDA, their effectiveness must be proven. As a result, more research needs to be conducted into understanding how the placebo effect can alter clinical trials and how researchers can better account for it. One potential change that has been suggested to reduce the placebo effect in clinical trials is collecting data with electronic questionnaires, which would prevent any interactions between the participants and the administrators from affecting studies [21]. Learning more information about MDD and the placebo effect will hopefully lead to new and effective ways to treat depression and better the lives of millions of people worldwide.
References
- Wolf, S. (1950). Effects of suggestion and conditioning on the action of chemical agents in human subjects; the pharmacology of placebos. The Journal of Clinical Investigation, 29(1), 100-109. doi: 10.1172/JCI102225.
- Wager, T.D., & Atlas, L.Y. (2015). The neuroscience of placebo effects: connecting context, learning and health. Nat Rev Neurosci, 16(7), 403–418 . doi:10.1038/nrn3976
- Hillhouse, T. M., & Porter, J. H. (2015). A brief history of the development of antidepressant drugs: from monoamines to glutamate. Experimental and clinical psychopharmacology, 23(1), 1–21. doi: 10.1037/a0038550
- Hasin, D.S., Sarvet, A.L., Meyers, J.L., Saha, T.D., Ruan, W.J., Stohl, M., & Grant, B.F. (2018). Epidemiology of Adult DSM-5 Major Depressive Disorder and Its Specifiers in the United States. JAMA Psychiatry. 75(4), 336–346. doi: 10.1001/jamapsychiatry.2017.4602
- Ng, J., Papandreou, A., Heales, S. J., & Kurian M. A. (2015). Monoamine neurotransmitter disorders—clinical advances and future perspectives. Nat Rev Neurol. 11(10), 567–584 . doi: 10.1038/nrneurol.2015.172
- Salomon, R. M., Miller, H. L., Krystal, J. H., Heninger, G. R., & Charney, D. S. (1997). Lack of behavioral effects of monoamine depletion in healthy subjects. Biological psychiatry, 41(1), 58–64. doi: 10.1016/0006-3223(95)00670-2
- Berman, R. M., Sanacora, G., Anand, A., Roach, L. M., Fasula, M. K., Finkelstein, C. O., Wachen, R. M., Oren, D. A., Heninger, G. R., & Charney, D. S. (2002). Monoamine depletion in unmedicated depressed subjects. Biological psychiatry, 51(6), 469–473. doi: 10.1016/s0006-3223(01)01285-9
- Kaltenboeck, A., & Harmer, C. (2018). The neuroscience of depressive disorders: A brief review of the past and some considerations about the future. Brain and Neuroscience Advances. doi: 10.1177/2398212818799269
- Cruzat, V., Macedo Rogero, M., Noel Keane, K., Curi, R., & Newsholme, P. (2018). Glutamine: Metabolism and Immune Function, Supplementation and Clinical Translation. Nutrients, 10(11), 1564. doi: 10.3390/nu10111564
- Block, W., Träber, F., von Widdern, O., Metten, M., Schild, H., Maier, W., Zobel, A., & Jessen, F. (2009). Proton MR spectroscopy of the hippocampus at 3 T in patients with unipolar major depressive disorder: correlates and predictors of treatment response. The international journal of neuropsychopharmacology, 12(3), 415–422. doi: 10.1017/S1461145708009516
- Auer, D. P., Pütz, B., Kraft, E., Lipinski, B., Schill, J., & Holsboer, F. (2000). Reduced glutamate in the anterior cingulate cortex in depression: an in vivo proton magnetic resonance spectroscopy study. Biological psychiatry, 47(4), 305–313. doi: 10.1016/s0006-3223(99)00159-6
- Rolls E. T. (2019). The cingulate cortex and limbic systems for emotion, action, and memory. Brain structure & function, 224(9), 3001–3018. doi: 10.1007/s00429-019-01945-2
- Hashmi, A. M., Butt, Z., & Umair, M. (2013). Is depression an inflammatory condition? A review of available evidence. JPMA. The Journal of the Pakistan Medical Association, 63(7), 899–906.
- Fountoulakis, K. N., McIntyre, R. S., & Carvalho, A. F. (2015). From Randomized Controlled Trials of Antidepressant Drugs to the Meta-Analytic Synthesis of Evidence: Methodological Aspects Lead to Discrepant Findings. Current neuropharmacology, 13(5), 605–615. doi: 10.2174/1570159x13666150630174343
- Geuter, S., Eippert, F., Hindi Attar, C., & Büchel, C. (2013). Cortical and subcortical responses to high and low effective placebo treatments. NeuroImage, 67, 227–236. doi: 10.1016/j.neuroimage.2012.11.029
- Lidstone, S. C., Schulzer, M., Dinelle, K., Mak, E., Sossi, V., Ruth, T. J., . . . Stoessl, A. J. (2010). Effects of Expectation on Placebo-Induced Dopamine Release in Parkinson Disease. Archives of General Psychiatry, 67(8), 857-865. doi: 10.1001/archgenpsychiatry.2010.88
- Báez-Mendoza, R., & Schultz, W. (2013). The role of the striatum in social behavior. Frontiers in neuroscience, 7, 233. doi: 10.3389/fnins.2013.00233
- Papakostas, G. I., Martinson, M. A., Fava, M., & Iovieno, N. (2016). Demographic variables, design characteristics, and effect sizes of randomized, placebo-controlled, monotherapy trials of major depressive disorder and bipolar depression. The Journal of clinical psychiatry, 77(5), e619–e624. doi: 10.4088/JCP.14r09767
- Cipriani, A., Furukawa, T. A., Salanti, G., Chaimani, A., Atkinson, L. Z., Ogawa, Y., . . . Geddes, J. R. (2018). Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: A systematic review and network meta-analysis. The Lancet (British Edition), 391(10128), 1357-1366. doi: 10.1016/S0140-6736(17)32802-7
- Kirsch, I. (2014). Antidepressants and the Placebo Effect. Zeitschrift fur Psychologie, 222(3), 128–134. doi: 10.1027/2151-2604/a000176
- Li, F., Nasir, M., Olten, B., & Bloch, M.H. (2019) Meta-Analysis of Placebo Response in Adult Antidepressant Trials. CNS Drugs, 33(10), 971–980. doi: 10.1007/s40263-019-00662-y
- Rutherford, B. R., Wall, M. M., Brown, P. J., Choo, T. H., Wager, T. D., Peterson, B. S., Chung, S., Kirsch, I., & Roose, S. P. (2017). Patient Expectancy as a Mediator of Placebo Effects in Antidepressant Clinical Trials. The American journal of psychiatry, 174(2), 135–142. doi: 10.1176/appi.ajp.2016.16020225
- Delmas, H., Batail, J. M., Falissard, B., Robert, G., Rangé, M., Brousse, S., Soulabaille, J., Drapier, D., & Naudet, F. (2017). A randomised cross-over study assessing the "blue pyjama syndrome" in major depressive episode. Scientific reports, 7(1), 2629. doi: 10.1038/s41598-017-02411-x
- Colagiuri, B., Schenk, L.A., Kessler, M.D., Dorsey, S.G, & Colloca, L. (2015). The placebo effect: From concepts to genes. Neuroscience, 307, 171-190. doi: 10.1016/j.neuroscience.2015.08.017
- Krell, H. V., Leuchter, A. F., Morgan, M., Cook, I. A., & Abrams, M. (2004). Subject expectations of treatment effectiveness and outcome of treatment with an experimental antidepressant. The Journal of clinical psychiatry, 65(9), 1174–1179. https://doi.org/10.4088/jcp.v65n0904
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. (2018). Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. The Lancet (British Edition), 392(10159), 1789-1858. doi: 10.1016/S0140-6736(18)32279-7
- Corriger, A., & Pickering, G. (2019). Ketamine and depression: a narrative review. Drug design, development and therapy, 13, 3051–3067. doi: 10.2147/DDDT.S221437
