Obsessive-compulsive disorder (OCD) is an anxiety disorder in which a person experiences excessive unwanted thoughts, urges, or impulses that may or may not be followed by repetitive, compulsive behaviors [1]. In the most severe cases, the compulsive behaviors, such as excessive grooming, checking, or cleaning, can seriously disrupt one’s daily activities and routines. Even though patients with OCD understand that their fears are irrational, they still perform such actions because they make them less anxious and distressed [1]. In the U.S., one in 100 adults have this disorder [2]. While notable progress has been made in uncovering cellular mechanisms and creating pharmacological and psychological therapies, the causes of OCD still remain elusive. Nonetheless, over the past few decades, researchers have found a link between the maladaptive immune system and observed OCD symptoms. This newly discovered link could lead to the development of new treatment methods [3].
Biological Basis of OCD
In order to develop effective treatments for OCD, a better understanding of the disorder’s biological mechanisms is needed. OCD research studies have revealed structural abnormalities in four regions of the brain: the orbitofrontal cortex (OFC), basal ganglia, anterior cingulate cortex (ACC), and thalamus [4]. These brain areas form cortico-striatal-thalamo-cortical (CSTC) neural circuits, which are overactive in patients with OCD [5, 6] . In the CSTC pathway, the OFC and the ACC usually send the “worry input” messages to the thalamus through the basal ganglia. Normally, the basal ganglia inhibits this input, filtering out unnecessary worries. In a neuroimaging study of OCD, researchers discovered increased neuronal activity in the CSTC pathway, particularly in OFC and caudate nucleus of the basal ganglia [7]. To test how the OCF affects OCD, another group of researchers stimulated the medial OFC in mice and observed increased grooming behavior similar to the compulsions observed in OCD [8]. Furthermore, the overly active basal ganglia in OCD makes people feel that something is wrong, which leads them to perform compulsive behaviors [9]. Disruption of the structures in the CSTC pathway in people with OCD also correlates with deficits in cognitive functions, such as decision making, attention, and memory.
Neuroinflammation
Even though studies have shown that dysfunctional OFC and basal ganglia lead to observed compulsive behaviors, no one knows why those structures are disrupted in the first place. However, one discovery suggests that a dysfunctional immune system might be a possible cause of some cases of OCD [11]. The study showed that children with autoimmune neuropsychiatic disorders caused by a strep infection developed sudden-onset OCD symptoms. The infection causes the immune system to attack the hosts’ own tissues in the basal ganglia, the region that is affected in patients with OCD [12][13]. This autoimmune attack disrupts the function of brain structures that may result in the development of OCD. Since then, researchers have started to explore the immunological basis of OCD [5].
When the immune system detects foreign bodies such as viruses, infections, or injuries, it produces antibodies to tag them for destruction. One of the side effects of this immune response is inflammation. Researchers discovered that brain inflammation is 32% higher in individuals with OCD than those without the disorder [3]. In another study, researchers detected the presence of the anti-basal ganglia antibodies in OCD-affected individuals, suggesting that the immune system might be targeting the basal ganglia [14][15].
Role of Microglia
Microglia, a type of immune cell located in the brain, have been found to play an important part in causing the inflammation associated with the onset of OCD symptoms. Although these cells are found in the brain, a subpopulation of microglia are actually produced in the bone marrow [17]. In his studies on mice, one researcher noted that mutations in microglia’s Hoxb8 gene cause compulsive grooming behaviors. This pathological behavior in the mutant Hoxb8 mice could be stopped with normal bone marrow transplantation. This finding suggests possible implications for potential therapies, such as bone marrow transplantation in humans, for the treatment OCD. Normally, Hox genes help position body parts in the developing embryo, and it is currently unknown how mutations in Hoxb8 genes in microglia cause repetitive compulsive behaviors in mice or humans [17].
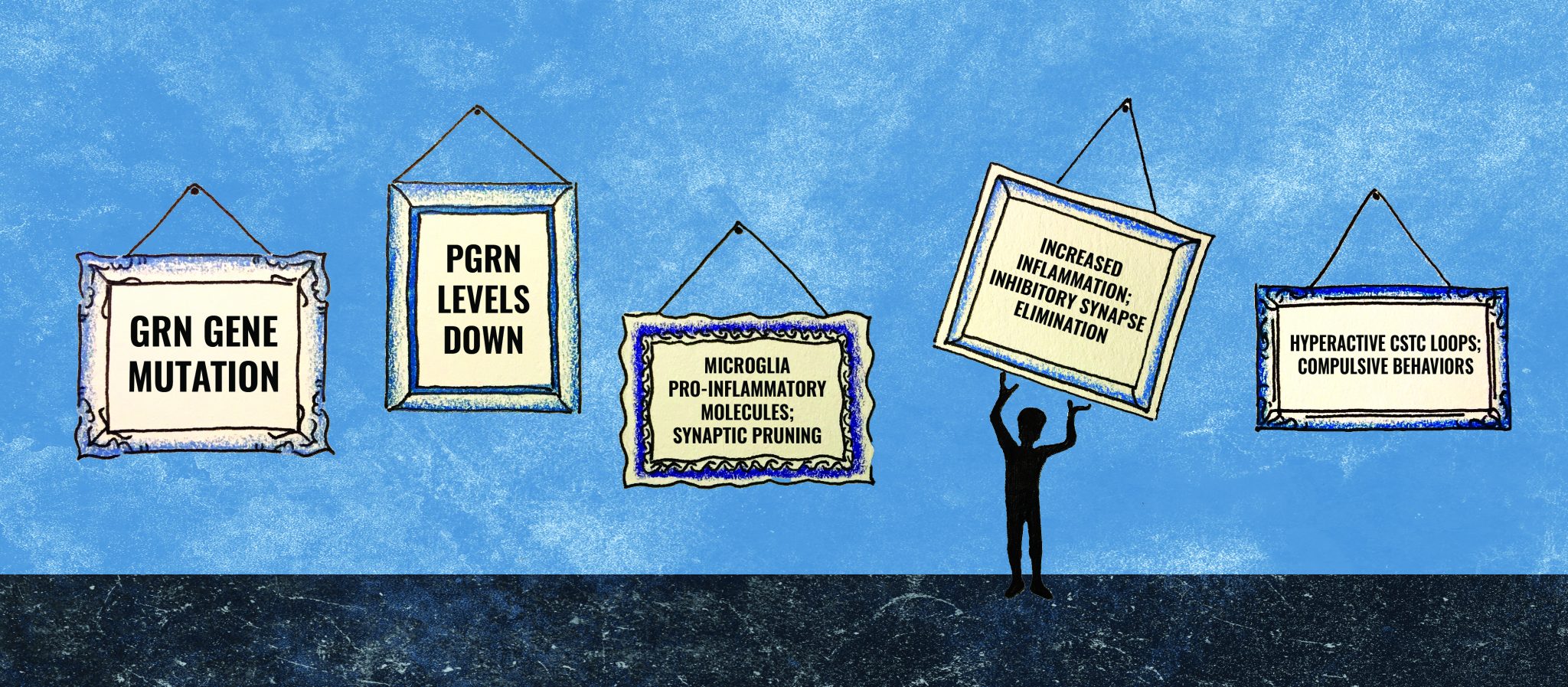
Another mutation in the microglia’s progranulin (GRN) gene might explain the development of both inflammation of the cortex and the hyperactivity of the CSTC loop [18]. Progranulin (PGRN) is a key regulator of inflammation in the brain. Studies on mice have shown how a mutation in the GRN gene drastically decreases PGRN protein levels. When this protein is deficient in microglia, the production of pro-inflammatory molecules increases, which could possibly explain the increased levels of inflammation in people with OCD. Loss of PGRN also causes microglia to be more efficient at synaptic pruning. If mutated microglia eliminated the inhibitory synapses in the thalamus, they could cause hyperactivity in the CSTC loop and subsequent compulsive behaviors [18]. Understanding how microglia become harmful to the host is crucial to the development of new treatments that target microglia activity and thus potentially relieve OCD symptoms.
Treatments
In addition to talk therapies, there are a few medical and surgical treatments considered to be the current standard of care for OCD. Even though these treatments relieve OCD symptoms considerably, around 30% of patients do not respond to such treatments [19]. Usually, when OCD is diagnosed, doctors first prescribe selective serotonin reuptake inhibitors (SSRIs), which partially relieve OCD symptoms in 40-60% of patients. SSRIs are found to reduce anxiety levels in OCD; however, SSRIs do not always work, and they have a variety of side effects including gastrointestinal distress, restlessness, and insomnia [19].
When OCD symptoms get worse over time and become too severe, patients may resort to surgery. Doctors drill the skull and destroy one of two regions in the brain: the anterior cingulate cortex (ACC) or the anterior limb of the internal capsule. The destruction of the ACC and the anterior limb of the internal capsule reduces anxiety by decreasing transmission from “worry” input messages. However, these methods have only proven successful for 40-50% of patients with OCD [20]. Moreover, this surgery has been associated with substantial side effects, such as fatigue, apathy, and weight gain [21].
Another surgical treatment for OCD is called deep brain stimulation (DBS), where a thin metal electrode is implanted into the basal ganglia. Once implanted, pulses of energy are emitted to decrease abnormal activity in the brain and, in this case, relieve OCD symptoms [22]. However, it is still not known how DBS is able to modulate the neural circuit implicated in OCD [23]. Previous research studies demonstrated that 61% of patients respond well to this treatment. Unlike in other surgeries, brain tissue is not destroyed in the process, so the functions of those cells are not lost [24].
New types of treatments could potentially target inflamed regions of the brain and microglial activity to relieve OCD symptoms. However, scientists still do not know the exact mechanism of inflammation, and more research needs to be done before producing anti-inflammatory drugs [25]. To target microglial activity, researchers hope to develop a method to transplant wild-type microglia from bone marrow into the brain safely and efficiently. Microglia transplantation has been found to alleviate OCD symptoms in mice, but the current procedure is not yet safe to conduct in human clinical trials [17]. Microglial activity can also be controlled by an antibiotic called minocycline [26]. Minocycline has not been used to treat OCD symptoms, but may be a potential candidate because it reduces microglial proliferation as well as pro-inflammatory molecule production in stroke and Huntington’s disease [26]. These emerging treatments have a great potential to reduce OCD symptoms.
Conclusion
OCD was once considered rare, but now it is one of the most common neurological disorders in the U.S., where 2-3% of the population have this disorder [27]. Although it might be surprising at first, the immune system seems to affect the activity of the CSTC neural circuit, contributing to the development of OCD. Researchers have discovered that microglia remove the inhibitory synapses in the ventral thalamus, which disrupts the balance between excitatory and inhibitory signals. As a result, the CSTC loop becomes more active than usual, which may explain the repetitive compulsory behaviors in patients with OCD. This discovery opens doors to the development of new medications that target neuroinflammation and microglia to counteract the loss of inhibitory signals. Great progress has been made in understanding the biological mechanisms of OCD, and each discovery helps the development of better treatment for this widespread disorder.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5. Washington, D.C: American Psychiatric Association.
- Kessler RC, Chiu WT, Demler O, Walters EE. (2005). Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R). Archives of General Psychiatry. 62: 617-27.
- Attwells S., Setiawan E., Wilson A. (2017). Inflammation in the Neurocircuitry of Obsessive-Compulsive Disorder. JAMA Psychiatry. 74: 833-840.
- McGuire PK, Bench CJ, Frith CD, Marks IM, Frackowiak RS, Dolan RJ. (1994). Functional anatomy of obsessive-compulsive phenomena. Br. J. Psychiatry. 164: 459-68.
- Ting J, Feng G. (2011). Neurobiology of obsessive–compulsive disorder: insights into neural circuitry dysfunction through mouse genetics. Current Opinion in Neurobiology. 21: 842-848.
- Nakao T, Okada K, Kanba S. (2014). Neurobiological model of obsessive–compulsive disorder: Evidence from recent neuropsychological and neuroimaging findings. Psychiatry and Clinical Neurosciences. 68: 587-605.
- Nakao T, Okada K, Kanba S. (2014). Neurobiological model of obsessive-compulsive disorder: evidence from recent neuropsychological and neuroimaging findings. Psychiatry Clin Neurosci. 68:587-605
- Ahmari S, Spellman T, Douglass N, Kheirbek M, Simpson B, Deisseroth K, Gordon J, Hen R. (2013). Repeated Cortico-Striatal Stimulation Generates Persistent OCD-Like Behavior. 6137: 1234-1239
- Mulders A, Plantinga B, Schruers K, Duits A, Janssen M, Ackermans L, Leentjens A, Jahanshahi A, Temei Y. (2016). Deep brain stimulation of the subthalamic nucleus in obsessive-compulsive disorder: Neuroanatomical and pathophysiological considerations. European Neuropsychopharmacology. 26: 1909-1919.
- Kamaradova D, Hajda M,Prasko J, Taborsky J, Grambal A, Latalova K, Ociskova M, Brunovsky M, Hlustik P. (2016). Cognitive deficits in patients with obsessive–compulsive disorder – electroencephalography correlates. Neuropsychiatr Dis Treat. 12: 1119–
- Swedo S, Leonard H, Garvey M, Mittleman B, Allen A, Perlmutter S, Dow S, Zamkoff J, Dubbert B, Lougee L. (1998). Pediatric Autoimmune Neuropsychiatric Disorders Associated With Streptococcal Infections: Clinical Description of the First 50 Cases. The American Journal of Psychiatry. 155: 264-271
- PANDAS-Questions and Answers. (n.d.). Retrieved October 30, 2017, from https://www.nimh.nih.gov/health/publications/pandas/index.shtml .
- PANDAS: Effects on the brain. (n.d.) Retrieved December 14, 2017, from http://www.pandasnetwork.org/understanding-pandaspans/effects-on-the-brain/
- Najjar S, Pearlman D, Alper K, Najjar A, Devinsky O. (2013). Neuroinflammation and psychiatric illness. Journal of Neuroinflammation. 10: 816.
- Hage A, Banaschewski T, Buitelaar J, Dijkhuizen R, Franke B, Lythgoe D, Mechler K, Williams S, Dittmann R. (2016). Glutamatergic medication in the treatment of obsessive compulsive disorder (OCD) and autism spectrum disorder (ASD) – study protocol for a randomised controlled trial. Trials. 17: 141.
- Chen SK, Tvrdik P, Peden E, Cho S, Wu S, Spangrude G, Capecchi MR. (2010). Hematopoietic origin of pathological grooming in Hoxb8 mutant mice. Cell. 141: 775-85.
- Lui H, Zhang J, Makinson S, Cahill M, Kelley K, Huang HY, Shang Y, Oldham M, Martens L, Gao F, Coppola G, Sloan S, Hsieh C,Kim C, Bigio E, Weintraub S, Mesulam MM, Rademakers R, Mackenzie I, Seeley W, Karydas A, Miller B, Borroni B, Ghidoni R, Farese R, Paz J, Barres B, Huang E. (2016). Progranulin Deficiency Promotes Circuit-Specific Synaptic Pruning by Microglia via Complement Activation. 165: 921–935.
- Harvard Health Publishing (n.d.). Treating obsessive-compulsive disorder. Retrieved October 31, 2017, from https://www.health.harvard.edu/mind-and-mood/treating-obsessive-compulsive-disorder .
- Brain Surgery for OCD. (2014). Retrieved October 31, 2017, from https://iocdf.org/about-ocd/treatment/brain-surgery-for-ocd/
- Rück C, Karlsson A, Steele D. (2008). Capsulotomy for Obsessive-Compulsive Disorder. Arch Gen Psychiatry . 65:914-922
- Zaehle T, Galazky I. (2017). Effects of deep brain stimulation of the subthalamic nucleus on perceptual decision making. Neuroscience. 343: 140-146.
- Greenberg B, Malone D, Friehs G, Rezai A, Kubu C, Malloy P, Salloway S, Okun M, Goodman W, Rasmussen S. (2006). Three-Year Outcomes in Deep Brain Stimulation for Highly Resistant Obsessive–Compulsive Disorder. Neuropsychopharmacology . 31: 2384–2393
- Deep Brain Stimulation for Highly Treatment-Resistant OCD. (2017). Retrieved October 31, 2017, from https://iocdf.org/expert-opinions/expert-opinion-dbs/
- CAMH researchers discover brain inflammation in people with OCD. (n.d.). Retrieved October 31, 2017, from http://www.camh.ca/en/hospital/about_camh/newsroom/news_releases_media_advisories_and_backgrounders/current_year/Pages/CAMH-researchers-discover-brain-inflammation-in-people-with-OCD.aspx
- Tikka T, Koistinaho J. (2001). Minocycline Provides Neuroprotection Against N-Methyl-d-aspartate Neurotoxicity by Inhibiting Microglia. J Immunol. 166: 7527-7533
- Ruscio A, Stein D, Chiu W, Kessler R. (2010). The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 15:53-63