Although the World Health Organization (WHO) recently declared the end of the international public health emergency for the Zika virus (ZIKV), ZIKV remains a public health challenge requiring effective action [1]. As of October 2016, ZIKV infections occurred in 67 countries with 56 individual countries reporting outbreaks since 2015. What is more concerning is that 22 countries have reported microcephaly and other central nervous system (CNS) disorders that may be related to ZIKV [1]. Scientific investigations have concluded that ZIKV causes microcephaly and Guillain-Barre syndrome, which are debilitating neurological disorders characterized by a smaller-than-average head and severe muscle weakness, respectively [2]. Much is still unknown about ZIKV and how it causes these disorders, but there is evidence suggesting ZIKV targets the nervous system preferentially [2]. While our knowledge of ZIKV will increase as more research is published, there is vast uncertainty about the virus and it may be years before its mechanisms are unraveled, despite being discovered decades ago.
Background
ZIKV was first identified in the analysis of a blood sample from a rhesus monkey that contracted a fever while living in the Zika Forest of Uganda in 1947 [3]. A year later, ZIKV was isolated from a group of Aedes africanus mosquitoes in the same forest, confirming the transmission from mosquito to primate [3]. In the ensuing years, ZIKV spread across middle Africa to Asia, and in 1966, ZIKV was isolated from Aedes aegypti mosquitoes in Malaysia in the first known sighting in Southeast Asia [4]. Before 2007, ZIKV was contained within tropical African and Asian countries near the equator, and only 13 human cases of ZIKV infection were reported, likely due to the inaccuracy of ZIKV detection tests during this time period [5].
ZIKV was first identified outside of Africa and Asia in the state of Yap, part of Micronesia in the western Pacific Ocean, with 49 confirmed ZIKV infections in 2007 [5]. The first documented case of the sexual transmission of ZIKV occurred in August 2008, when an infected U.S. scientist working in Senegal returned home and his wife subsequently became sick with ZIKV symptoms. This marked the first time that ZIKV was confirmed not to have been transmitted by a bite from an infected mosquito [5]. Another method of transmission was discovered in 2013 when ZIKV was found in two newborn infants in French Polynesia during an outbreak [6]. These two cases provided evidence for mother-to-child transmission of ZIKV while the infant was in the womb or through breastfeeding [6]. Sexual transmission and vertical, or mother-to-child, transmission were further supported by viral samples found in both semen and amniotic fluid in various cases [5]. ZIKV has also been detected in blood from blood donors, and infections via blood transfusion have been reported in Brazil [7]. The most notable outbreak occurred in March of 2015 in Brazil, when ZIKV was identified in patients experiencing an illness characterized by fever and muscle and joint pain [8]. Analysis of the virus showed 99% compatible identity with nucleotide sequences from an isolated sample of ZIKV from French Polynesia, confirming its spread from Micronesia to Brazil [8]. Since these first reported cases, ZIKV has infected hundreds of thousands of people in Brazil and spread to countries across Latin America up to Mexico and the U.S. [1]. Unfortunately, the spread of ZIKV does not show signs of slowing due to its method of transmission.
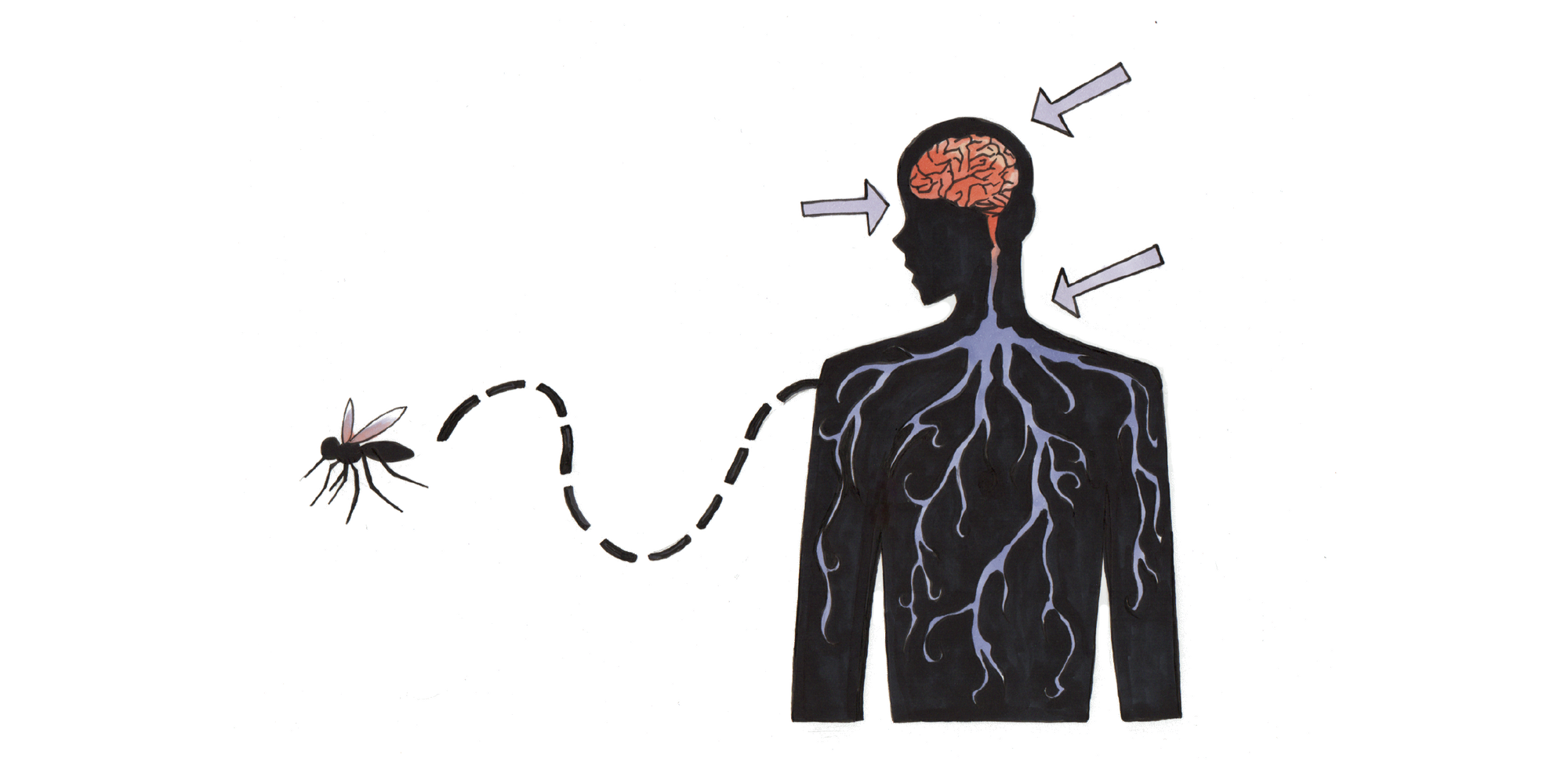
ZIKV is a member of the Flavivirus genus and consists of an encapsidated single-stranded RNA genome surrounded by a spherical envelope [9]. ZIKV is spread mainly by mosquitoes of the genus Aedes across tropical regions of the world, where they thrive. A mosquito becomes a carrier of ZIKV by biting an infected person, and transmission to another individual can occur if the infected mosquito bites an uninfected person. Some of the ways ZIKV spreads from region to region are when infected people move to areas that do not have ZIKV or an infected mosquito is carried into a new area [9].
Many people who are infected do not realize they carry ZIKV, as a significant majority do not experience any symptoms [9]. Those who experience mild symptoms typically have some combination of fever, fatigue, rash, and red eyes. There are no unique symptoms of ZIKV, which often leads to misdiagnosis with other related flaviviruses, an important explanation for the low numbers of reported cases before 2007. Unfortunately, ZIKV has been shown to cause two neurological disorders called microcephaly and Guillain-Barre syndrome in infants and adults, respectively. This connection makes ZIKV a source of major concern for the World Health Organization since these disorders lead to severe neurological impairments [9].
Neurological Disorders
Microcephaly is a birth condition that manifests as a reduction in infantile skull size relative to normalized standards for the infant’s age [2]. The literal meaning of microcephaly translates to “small head,” and is often used in the same context as microencephaly, a condition that causes newborn infants to have smaller-than-average brains. In ZIKV-related cases, both microcephaly and microencephaly occur at the same time rather than independently [9]. Through unknown mechanisms, ZIKV hinders normal brain development while a fetus is in the womb. Since the head develops in proportion to brain size, a smaller head is the result of a smaller brain [9].
ZIKV is neurotropic, or has an affinity for nervous tissue, as determined by the isolation of ZIKV samples within the neonatal brain [10]. This finding is further supported by evidence that shows viral replication occurs within the brains in those infected with ZIKV. Furthermore, in neonatal cases, calcification, or a buildup of calcium salts that resembles destroyed neuronal structures, has been found within the placenta. This suggests ZIKV may have destroyed neural structures during their formation, leading to the arrested development of the cerebral cortex [10].
In another case study, three babies who died after birth in Brazil were autopsied. The infants’ tissue was examined after their mothers, who had contracted ZIKV during their pregnancies, gave consent [11]. Abnormal brain development was identified in these infants, and microcephaly was diagnosed with an ultrasound examination while in the womb. Other causes of microcephaly, such as alcohol and drug use, were eliminated, and tests for viruses related to ZIKV came back negative. The ZIKV genome was identified in two infants within postmortem brain tissue, and one infant also had viral copies in the cerebellum, spinal cord, and lung. In addition, scientists observed severe cerebral atrophy, or destruction of neurons and their connections, and postmortem analysis showed enlarged ventricles as well as clusters of calcification within the brain. Cerebral atrophy may be explained by an interference in the formation and migration of neural cells during brain development due to ZIKV infection; however, there is currently no significant evidence identifying this mechanism [11].
In cases where ZIKV causes microcephaly, abnormal brain development leads to an undersized cerebral cortex, resulting in severely impaired language and motor development that produces varying degrees of intellectual impairment throughout life [9]. Treatment will never fully reverse impairments, as these conditions are permanent, which is why various health organizations around the world issued an advisory for pregnant women to avoid travelling to areas with current ZIKV infections [12]. Additionally, ZIKV-caused microcephaly has proven fatal, as many infants have died from complications arising from the condition [9].
Currently, there is no known explanation as to why ZIKV causes Guillain-Barre syndrome. This relationship was first established by the comparison of Guillain-Barre incidence rates during a ZIKV outbreak [13]. In French Polynesia, 42 patients who developed Guillain-Barre all had prior ZIKV infections during the 2013 outbreak. Proof of previous ZIKV infection was based off of the finding that all patients specifically had neutralizing antibodies against ZIKV [13]. Another case study was done in Colombia during an outbreak from November 2015 to March 2016 [14]. 68 patients with Guillain-Barre syndrome were evaluated clinically, and 42 of these patients underwent a virologic study. ZIKV symptoms were reported for 97% of the patients, with a median of 7 days between the appearance of the symptoms and the onset of Guillain-Barre syndrome. Furthermore, 40% of the 42 patients who underwent laboratory testing had positive results for ZIKV as assessed by RT-PCR assays [14]. RT-PCR has been used extensively as an identification test for ZIKV, as ZIKV-specific primers that can bind to unique parts of the ZIKV genome have been developed and used since the 2007 Yap Island outbreak [15]. While ZIKV continues to spread at an alarming rate, tests like RT-PCR have made identification of ZIKV infection simple, allowing researchers to make connections between ZIKV and neurological disorders in areas of ZIKV infection.
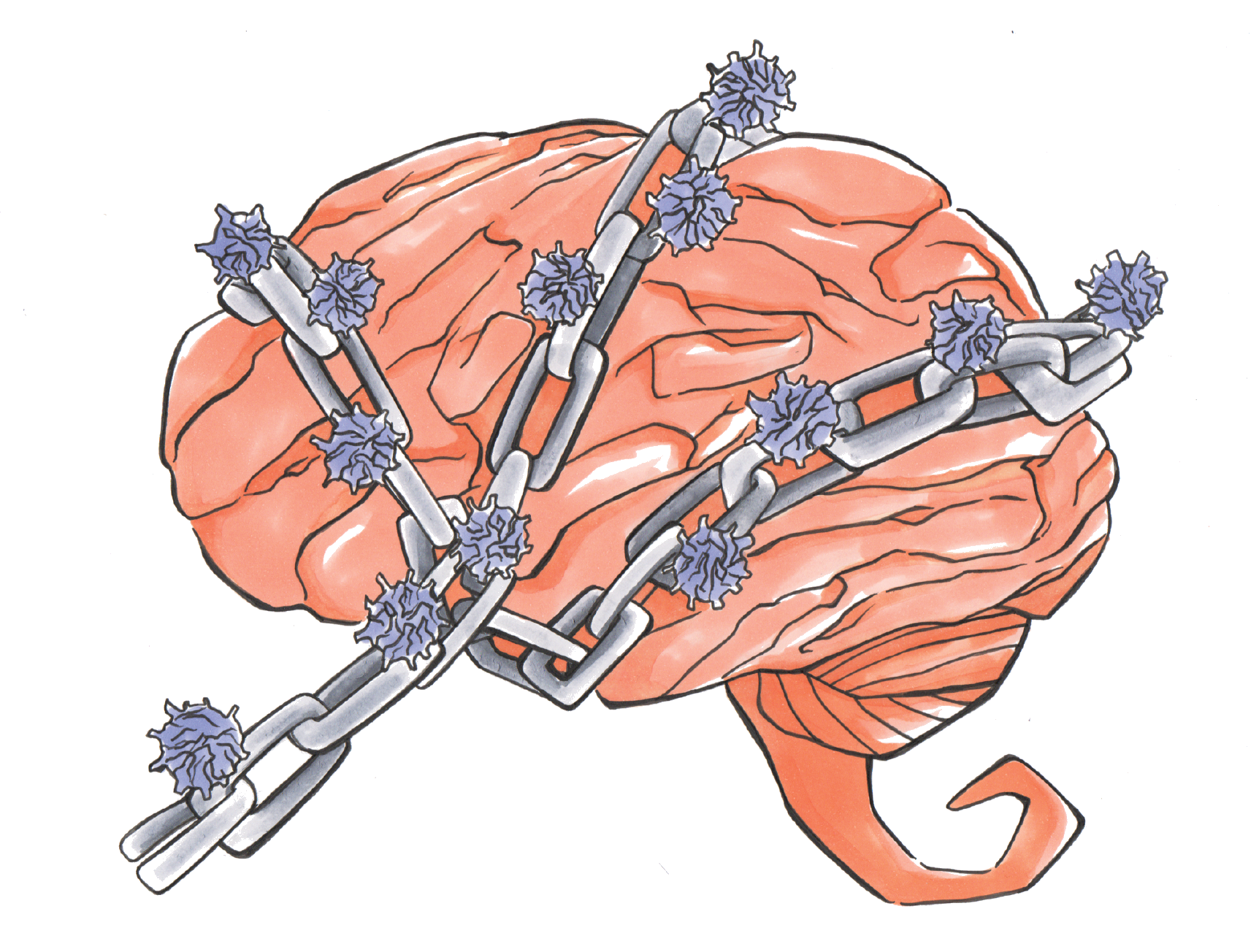
While microcephaly results in permanent neurological consequences for infants, recovery is possible for patients with Guillain-Barre syndrome [16]. This syndrome is an autoimmune disorder in which the immune system of an affected patient attacks the peripheral nervous system, the part of the nervous system that does not consist of the brain and spinal cord. The patient’s immune system slowly degrades the myelin sheath around nerve axons, causing lower conduction speeds of electrical signals to and from the brain and spinal cord. Since myelin helps to propagate signals faster along axons, longer travel times for electrical signals result in severe muscle weakness. The onset of this disorder can be rapid, ranging from a few days to a few weeks. Fortunately, it is possible to recover through two methods treatment, immunoglobulin (Ig) therapy and plasmapheresis, although the death rate is still about 7.5%. Ig therapy involves flooding the body with immunoglobulins, or antibodies, pooled from donors without Guillain-Barre syndrome to decrease the immune system’s attack on the nervous system. With plasmapheresis, patients have their blood separated into its components, and the red and white blood cells are returned to the body without the plasma, or the colorless liquid portion of the blood. The reason why these treatments work is unknown, but they have proven to be effective in relieving muscle weakness [16].
Conclusion
Because ZIKV does not show any symptoms in a significant portion of human infections, it is unlikely that people will know they are infected. This means the ZIKV epidemic will continue as long as mosquitoes capable of carrying ZIKV are present and modern travel allows infected people to move to unaffected areas around the globe in a matter of hours. Fortunately, ZIKV is not inherently dangerous in terms of mortality, but people should still follow WHO or Centers for Disease Control guidelines for ZIKV and avoid traveling to areas with ZIKV if pregnant, as incidence of microcephaly and Guillain-Barre syndrome in infants whose mothers contract ZIKV is a major concern [12].
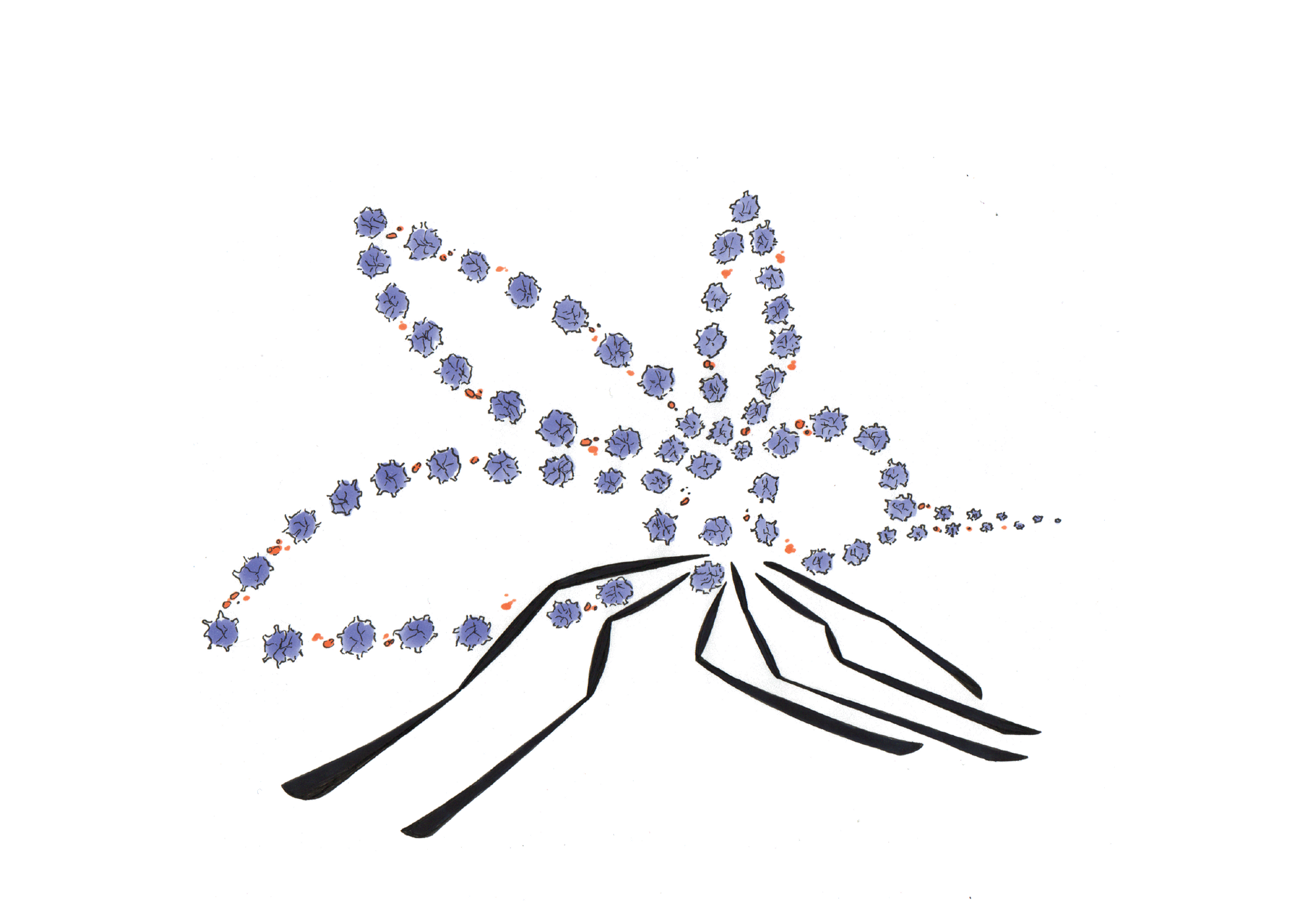
It is important for more research to be conducted as there is still great uncertainty surrounding ZIKV’s mechanisms, and the recent outbreak has resulted in millions of infections worldwide [1]. Currently, there is a ZIKV vaccine called VRC 319 in development that could prevent future infections; VRC 319 is presently in a Phase I clinical trial [17]. However, it will take months of extensive testing to determine the safety and efficacy of the vaccine, and even more time if the vaccine fails to be widely distributed [17]. There is also a promising antibody called C10 that binds to ZIKV surface proteins and locks their structure, preventing structural arrangement. This may stop ZIKV from infecting host cells by blocking its fusion with the cell, though it is important to note that C10 has only recently been identified and the mechanism is speculative [18]. While it may take years for a preventative treatment to be developed, research is needed to discover exactly how ZIKV causes microcephaly and Guillain-Barre syndrome. Once the mechanism is known, treatments can be designed to specifically target ZIKV and prevent it from harming nervous tissue.
References
- “Zika Virus Situation Report.” World Health Organization. Web. <http://www.who.int/emergencies/zika-virus/situation-report/24-november-2016/en/>
- Costello A., Dua T., Duran P., Gulmezoglu M., Oladapo O.T., Perea W., Pires J., Ramon-Pardo P., Rollins N., and Saxena S. (2016). Defining the Syndrome Associated with Congenital Zika Virus Infection. Bulletin of the World Health Organization. 94: 406-406A.
- Dick, G.W., Kitchen, S.F., and Haddow, A.J. Zika virus. I. Isolations and serological specificity. (1952). Transactions of the Royal Society of Tropical Medicine and Hygiene. 46:509–520.
- Marchette, N.J., Garcia, R., and Rudnick, A. Isolation of Zika virus from Aedes aegypti mosquitoes in Malaysia. (1969). The American Journal of Tropical Medicine and Hygiene. 18:411–415.
- Wikan N and Smith D.R. Zika Virus: History of a newly emerging arbovirus. (2016). Lancet: Infectious Diseases. 16:119-126.
- Bernard M, Lastere S, Teissier A, Cao-Lormeau VM, and Musso D. Evidence of perinatal transmission of Zika virus, French Polynesia, December 2013 and February 2014. (2014). Eurosurveillance. Epub.
- Motta, I.J.F. et al. Evidence for Transmission of Zika Virus by Platelet Transfusion. (2016). New England Journal of Medicine. 375: 1101-1103.
- Campos, GS, Bandeira, AC, and Sardi, SI. Zika virus outbreak, Bahia, Brazil. (2015). Emerging Infectious Disease. 21: 1885–1886.
- Paixao E.S., Barreto F., Teixeira, M.G., Costa M., and Rodrigues L.C. History, Epidemiology, and Clinical Manifestations of Zika Virus: A Systematic Review. (2016). American Journal of Public Health. 106: 606-612.
- Mlakar J. et al. Zika Virus Associated with Microcephaly. (2016). New England Journal of Medicine. 374: 951-958.
- Oliveira Melo A.S., Aguiar R.S., and Amorim M.M.R. Congenital Zika Virus Infection: Beyond Neonatal Microcephaly. (2016). JAMA Neurology. Epub.
- “Information for travellers visiting Zika affected countries.” World Health Organization. Web. < http://www.who.int/csr/disease/zika/information-for-travelers/en/>
- Cao-Lormeau V.M. et al. Guillain-Barre Syndrome Outbreak Associated with Zika Virus Infection in French Polynesia: A Case-Control Study. (2016). Lancet. 387: 1531-1539.
- Parra B. et al. Guillain-Barre Syndrome Associated with Zika Virus Infection in Colombia. (2016). New England Journal of Medicine. Epub.
- Pyke A.T., Daly M.T., Cameron J.N., Moore P.R., Taylor C.T., Hewitson G.R., Humphreys J.L. and Gair R. Imported Zika Virus Infection from the Cook Islands into Australia, 2014. (2014). PLoS Currents. Epub.
- “Guillain-Barre Syndrome Fact Sheet.” National Institute of Neurological Disorders and Stroke. Web. <http://www.ninds.nih.gov/disorders/gbs/detail_gbs.htm>
- "Safety and Immunogenicity of a Zika Virus DNA Vaccine, VRC-ZKADNA085-00-VP, in Healthy Adults.” National Institutes of Health. Web. <https://clinicaltrials.gov/ct2/show/NCT02840487>
- Zhang S. et. al. Neutralization Mechanism of a Highly Potent Antibody Against Zika Virus. (2016). Nature Communications. 7: 13679.