A coworker slurps chicken-noodle soup. A classmate refuses to stop coughing. A friend gulps down their coffee as if it were the last cup on earth. Many people find these sounds unpleasant, even irritating, but few experience an overwhelming, aggressive impulse to silence the source of the noise. This constitutes the sentiments of individuals suffering from the little-known, but growing condition known as misophonia.
Introduction: Overview of Misophonia
As revisions to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) continue to be proposed among clinicians and researchers, a growing topic of discussion concerns the potential inclusion of a condition known as misophonia. From the Greek “miso,” meaning hatred, and “phonic,” pertaining to or having the nature of sound, misophonia quite literally means “hatred of sound.” However, for individuals suffering from this condition, a specific set of sounds disproportionately triggers negative reactions. Specifically, human sounds of chewing, loud breathing, and throat clearing as well as external, nonhuman sounds such as engine noises, cause intense anxiety, aggression, and consequent avoidance behavior [1]. Misophonia also differs from other auditory disorders due to its emphasis on an individual’s emotional response. In contrast with phonophobia, in which fear serves as the dominant emotional response to a sound, misophonia primarily induces feelings of annoyance, revulsion, and agitation. Individuals suffering from this psychiatric condition often experience dysfunction in their personal, academic, and social lives depending on the severity of their symptoms.
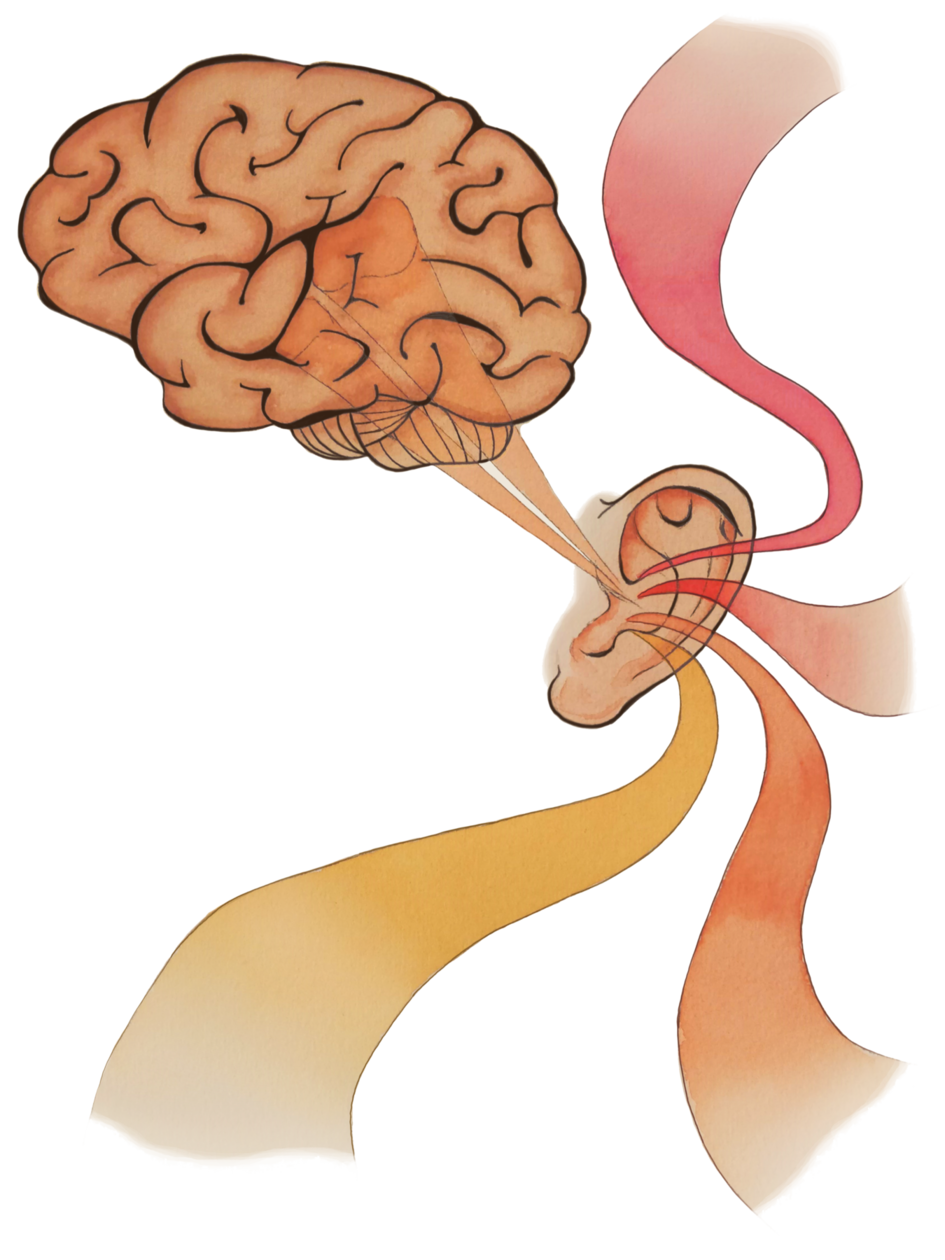
Although there is currently no neurophysiological indicator of misophonia, the symptoms of this condition typically manifest in autonomic arousal, which controls the fight-or-flight response, and emotional discomfort. Many researchers speculate that misophonia may involve problems with the cochlea, the spiral cavity of the inner ear that produces nerve impulses in response to sound vibrations. Other researchers have noted the possible overlap of misophonia with anxiety disorders, such as Obsessive-Compulsive Disorder (OCD), which also tends to provoke avoidance behavior, suggesting that misophonia may be an indicator of other psychiatric disorders rather than a separate mental illness [2].
Despite an increasing number of patients describing experiences with misophonia, the uncertainties of its neurological basis due to the lack of research on this condition prevent the DSM from proposing any official diagnostic criteria. Nonetheless, building interest in the psychological condition of misophonia has led researchers to investigate its neural basis and discuss whether misophonia should be regarded as a distinct brain disorder or as simply a symptom of related psychiatric disorders, such as OCD.

Neuroscience Behind Misophonia
One study led by Arjan Schröder of the University of Amsterdam investigated the potential link between misophonia and impairment in auditory processing by measuring the N1 response in patients with misophonia during an auditory oddball paradigm [3]. The N1 response or “peak” is a measurable sensory component involved in auditory stimulation and indicates the brain’s recognition of a sudden change in sensory stimuli. As an element of the electroencephalogram (EEG) signal, the N1 peak is used in tracking large scale brain activity in awake behaving patients. N1 peaks are often measured using an oddball paradigm, in which subjects watch a silent movie while listening to repetitive “standard” sounds and randomly-occurring, atypical “oddball” sounds. Researchers have found a reduced N1 peak in patients with schizophrenia and bipolar disorder, indicating a possible link between this sensory signal and psychiatric dysfunction. Schröder’s study reported a decreased N1 response in patients with misophonia, noting significantly lower peaks to the atypical tones in misophonia patients than in the control patients. In other words, the patients with misophonia did not attribute as much attention to the “oddball” tones as the control patients did [3].
This suggests that the patients with misophonia may experience a low-level neurological impairment during auditory processing. The researchers offered one explanation for this, noting that the misophonia patients were already in a state of heightened arousal compared to the control patients, as indicated by their respective responses to standard mood questionnaires. As a result, the patients with misophonia may not have recognized as distinct of a difference between typical and atypical tones as the control patients did, reinforcing a possible neurobiological hindrance in auditory processing [3].
A similar, more comprehensive, study looked at the neural basis as well as the physiological responses of misophonia. Researchers exposed misophonic and control subjects to misophonia trigger sounds, common unpleasant sounds, and neutral sounds. They collected fMRI data as well as behavioral data linked to autonomic response, such as heart rate and galvanic skin response, which measures electrical activity in the skin [4]. The results reported hyperactivity of the anterior insular cortex (AIC) in misophonic patients during the trigger sounds. The AIC acts as an integral part of the brain’s salience network, which directs attention to relevant stimuli specific to the individual. The study’s report of hyperactivity in this area suggests that patients with misophonia attribute a higher importance to trigger sounds. Moreover, the AIC is known to be a central hub for integrating sensory information and emotional response, which could explain the impulsive aggression that many individuals with misophonia report. Physiologically, when listening to trigger sounds, the misophonia patients exhibited an increased heart rate and galvanic skin response compared to the control patients. This makes sense, as individuals with misophonia typically engage in avoidance behavior, due to heightened autonomic arousal, to any situations, people, or environments that may present the trigger sounds. If the individual is unable to stop the noise or escape it, feelings of anxiety, aggression, and distress intensify. The mediation analysis performed in this study further suggests that the AIC contributed to this response in misophonic subjects [4].
The researchers also described greater functional connectivity of the AIC with other regions of the brain, including the hippocampus, amygdala, and areas of the cortex, in misophonic patients when exposed to the trigger sounds. The specific areas of the cortex that were observed constitute a network of brain regions thought to be primarily involved in inward thoughts and memories which may suggest that patients with misophonia negatively respond to trigger sounds due to their potential emotional association with certain memories [4]. The stronger connections among the AIC, hippocampus, and amygdala in misophonic patients reinforces the possible emotional salience misophonic patients may attribute to specific sounds.
Increased brain connectivity in misophonic patients was also observed in a study that measured neural activity during three different conditions that included both auditory and visual components [5]. These conditions followed a symptom provocation paradigm, in which patients were exposed to misophonia related triggers (e.g. lip smacking), common aversive cues (violent movie scenes), and neutral cues. Neural responses were then measured using an fMRI scanner. Both groups exhibited increased neural activity in the visual cortex, auditory cortex, and amygdala when exposed to the aversive and misophonia conditions. However, during the latter condition, misophonia patients showed increased activity in the auditory cortex, specifically in the right superior temporal cortex and left amygdala. These results indicate a possible association between misophonia and heightened activity in these areas. The researchers explained, however, that it remains unclear whether this response is due to an increased vigilance towards misophonic cues or a general higher level of stress, which may be an indication of misophonia’s relation to other anxiety disorders [5]. Overall, recent research suggests that abnormal auditory processing coupled with increased emotional salience towards specific trigger sounds potentially play a role in misophonia.
Symptoms or Disorder?
Instances of comorbidity, or the simultaneous presence of, OCD and related disorders lead researchers to question whether misophonia is a distinct disorder or simply a symptom of other established psychiatric disorders. One case report examined the presence of misophonia in an adolescent with comorbid OCD and Tourette’s Syndrome (TS) [6]. In addition to the behavioral symptoms common in OCD and TS, this adolescent reported substantial distress towards specific auditory stimuli that cause her to engage in confrontational and avoidant behavior, which are typical types of coping mechanisms for misophonia patients. The researchers noted the similarities in coping mechanisms between OCD and misophonia as both involve certain avoidant behavior towards the stimuli that provokes emotional distress. They also proposed the notion that there may be an overlap in the neurocircuitry of OCD, TS, and misophonia, specifically in areas involved in emotion, learning, and memory. Consequently, the researchers regarded this comorbidity of OCD spectrum disorders and misophonia as an indicator that the assessment of the potential presence of misophonia in patients already diagnosed with an anxiety disorder, such as OCD, may prove beneficial to the recognition and classification of this condition [6].
The high comorbidity rates of misophonia and similar anxiety disorders suggest that misophonia may simply be a symptom of other psychiatric illnesses. For example, one study documented that 52.4 percent of observed misophonic patients met the criteria for obsessive-compulsive personality disorder (OCPD), prompting researchers to discuss the possibility of OCPD as a predisposing or consequent factor of misophonia [7]. One study that surveyed 828 participants online found that there was a strong relation between misophonia and the obsessive behavior typically seen with OCD [8]. Furthermore, the study reported similarities between misophonia and anxiety sensitivity, emphasizing the overlap that exists between misophonia and other anxiety disorders. However, evidence of a distinct phenotype for misophonia is prompting researchers to discuss its classification as a separate disorder. For instance, the aforementioned study of N1 peaks in misophonic patients suggested an identifiable neurobiological indicator that separates misophonic patients from controls. The authors of this study also discussed how future research should attempt to precisely and separately define misophonia from other disorders. Overall, from a symptomatic perspective, researchers note that the diagnostic criteria for existing psychiatric disorders that resemble misophonia do not wholly encapsulate its symptoms. For example, while avoidant behavior is common with both OCD and misophonia, the aggressive impulses of misophonia are rarely seen with OCD patients [7].
Treatment
The perspective on misophonia as either a separate disorder or a manifestation of other illnesses directly affects the proper course of treatment for patients experiencing such symptoms. If this condition is a symptom of comorbid disorders related to OCD, then they may share a neural basis. Thus, treatments of misophonia should be modeled after treatments that have proven effective with OCD related disorders [9]. The comorbidity with OCD offers researchers hope that cognitive-behavioral therapy (CBT) that emphasizes exposure therapy and response prevention may prove extremely beneficial in helping misophonic patients overcome their extreme discomfort and anxiety [6]. Similarly, pharmacological treatment used for anxiety disorders, such as selective serotonin reuptake inhibitors (SSRIs) may be an effective treatment approach for patients who may not respond to CBT. However, there have been no studies conducted specifically investigating the pharmaceutical treatment of misophonia.
A few studies demonstrate the potential success of CBT as a treatment approach. A 2017 study assessed the effectiveness of CBT on 90 patients with misophonia utilizing basic exercises, such as task concentration (focusing on other non-triggering stimuli), counterconditioning (associating the triggering stimuli with a positive image), stimulus manipulation (controlling sounds on a computer), and relaxation techniques [10]. In 48 percent of the patients that received the CBT treatment, a significant reduction of symptoms occurred. A case study of two adolescent patients suffering from misophonia also reported significant diminishment of symptoms through treatment that incorporated techniques also used in CBT [11]. In their treatment of the two youths, researchers used prolonged exposure and response prevention exercises to try to increase the patients’ tolerance to trigger sounds. Undoubtedly, further research into effective treatment of patients with misophonia is an integral part in working towards a more comprehensive understanding of this condition.
Conclusion
Though past studies provide a solid foundational understanding of the neural basis behind misophonia, the appropriate psychiatric classification of it still requires extensive research. Much of this future research will likely aim towards determining how best to categorize the condition—as a symptom or disorder? Consequently, studies need to focus on establishing a more precise mapping of the specific neural mechanisms and pathways driving misophonic symptoms [12]. Limitations of previous studies consist mainly of small sample sizes, lack of research replications, and an inability to dissociate misophonia from other comorbid anxiety or OCD-related disorders.
Unfortunately, part of the problem researchers face when attempting to examine this phenomenon is simply a lack of people that report experiencing misophonic symptoms, despite a recent increase in anecdotal instances of misophonia. Due to this current absence of clear diagnostic protocol, individuals suffering from misophonic symptoms hesitate to report such experiences as many are afraid of the stigma attached to the ambiguous condition. Acknowledgement by the DSM of misophonia as either a distinct disorder or a symptom of other psychiatric disorders would mean a step towards certainty for patients and will heavily affect their evaluation, treatment, and personal perspective of the condition.
References
- Cavanna, A. E., & Seri, S. (2015). Misophonia: current perspectives. Neuropsychiatric disease and treatment , 11 , 2117–2123. doi:10.2147/NDT.S81438
- Bruxner, G. (2016). ‘Mastication rage’: a review of misophonia–an under-recognized symptom of psychiatric relevance?. Australasian Psychiatry , 24 (2), 195-197.
- Schröder, A., van Diepen, R., Mazaheri, A., Petropoulos-Petalas, D., Soto de Amesti, V., Vulink, N., & Denys, D. (2014). Diminished n1 auditory evoked potentials to oddball stimuli in misophonia patients. Frontiers in behavioral neuroscience , 8 , 123. doi:10.3389/fnbeh.2014.00123
- Kumar, S., Tansley-Hancock, O., Sedley, W., Winston, J. S., Callaghan, M. F., Allen, M., … & Griffiths, T. D. (2017). The brain basis for misophonia. Current Biology , 27 (4), 527-533.
- Schröder, A., San Giorgi, R., Van Wingen, G., Vulink, N., & Denys, D. (2015). P. 1. i. 015 Impulsive aggression in misophonia: results from a functional magnetic resonance imaging study. European Neuropsychopharmacology , (25), S307-S308.
- Webber, T. A., Johnson, P. L., & Storch, E. A. (2014). Pediatric misophonia with comorbid obsessive–compulsive spectrum disorders. General hospital psychiatry , 36 (2), 231-e1.
- Schröder A, Vulink N, Denys D (2013) Misophonia: Diagnostic Criteria for a New Psychiatric Disorder. PLoS ONE 8(1): e54706. https://doi.org/10.1371/journal.pone.0054706
- Cusack, S., Cash, T., & Vrana, S. (2018). An examination of the relationship between misophonia, anxiety sensitivity, and obsessive-compulsive symptoms. Journal of Obsessive-Compulsive and Related Disorders, 18 , 67-72.
- Like Nails on a Chalkboard: A Misophonia Overview. (n.d.). Retrieved from https://iocdf.org/expert-opinions/misophonia/.
- Schröder, A. E., Vulink, N. C., van Loon, A. J., & Denys, D. A. (2017). Cognitive behavioral therapy is effective in misophonia: an open trial. Journal of affective disorders , 217 , 289-294.
- McGuire, J. F., Wu, M. S., & Storch, E. A. (2015). Cognitive-behavioral therapy for 2 youths with misophonia. The Journal of clinical psychiatry , 76 (5), 573-574.
- Brout, J. J., Edelstein, M., Erfanian, M., Mannino, M., Miller, L. J., Rouw, R., … & Rosenthal, M. Z. (2018). Investigating misophonia: A review of the empirical literature, clinical implications, and a research agenda. Frontiers in neuroscience , 12 , 36.