Tenuous Times are a Great Time to Get “Rolling”
Our ever-changing socio-political landscape creates many feelings of uneasiness, and individual experiences of war, terrorism, or sexual abuse only corroborate these feelings. If left unabated, these feelings can manifest as a condition called post-traumatic stress disorder (PTSD), where these feelings cripple one’s own way of life, or even drive us to end it. About 4 percent of all individuals worldwide will experience PTSD. In the United States alone, 8 percent of individuals have been diagnosed with PTSD [1]. PTSD, along with other mental health disorders, now poses a significant threat to global health in our modern world.
Enter MDMA, commonly known as molly, ecstasy, or “E”. The drug has been associated with hard-partying rave culture and is often sold as a street drug. It gives the user intense feelings of euphoria, arousal, enhanced mood, increased sociability, and heightened perceptions, symptoms that are attributed to amplified effects of the neurotransmitters serotonin and norepinephrine and the hormones oxytocin and cortisol [2]. There have been no approved medical uses for MDMA, and its effects have contributed to numerous deaths [2]. This has led to its criminalization for use and sale across the world. However, despite its reputation as a party drug and its long-restricted legal status, researchers are now studying MDMA’s promising uses in treating PTSD by exploiting its euphoric psychological and neurobiological effects, which could lead to a new breakthrough therapy to a debilitating and costly mental disorder.
The Mind, Hijacked By Fear
After the experience of a traumatic event, PTSD manifests itself in three major ways: sustained elevated psychological arousal and hypervigilance, disturbing flashbacks of traumatic events, and/or persistent avoidance of fear-inducing or stress-inducing stimuli. These symptoms can cause major lifestyle complications, including suicide [3]. Around the world, PTSD commonly develops after war, rape, sexual abuse, or traffic collisions, but it can develop after any event traumatic enough as to threat or cause severe injury or death.
When we are subjected to a traumatic or stressful event, our bodies undergo an instinctive stress response, which is driven by the amygdala in the brain. You may know this as your “fight or flight” response—it keeps us safe by telling us what is dangerous by causing us to experience fear [3]. The amygdala is one of the first structures to react to a threat due to its fast-tracked neural pathways that bypass our cortex, the center for complex cognitive functions like personality and critical thinking, and its reaction is signaled and interpreted by other brain structures and organs to either fight ferociously or flee rapidly [3]. In a brain-imaging study of 200 military veterans with and without PTSD in a VA hospital in North Carolina, researchers found smaller amygdala volumes in veterans with PTSD as opposed to their non-PTSD counterparts, suggesting an association between PTSD and smaller amygdala volumes [4]. Brain-imaging studies of PTSD patients have also shown hypersensitivity in the amygdala in response to fear-inducing cues and fear-conditioning experiments [5]. In essence, a smaller amygdala could interfere with the normal processing of fear and stress, which could explain the sustained elevated arousal levels and hypervigilance of PTSD patients.
The amygdala signals numerous brain regions in response to stress and trauma, including the hippocampus and prefrontal cortex. The hippocampus houses our brain’s declarative memory capability. Any memory that you can name and describe is housed here, from the capital of your home state, to your first time in Disneyland. The interpretation of fear and stress in the amygdala is directly signaled to the hippocampus, for which a declarative memory of that stressful event is made and stored in the hippocampus. Through this signalling pathway we can see the link between the amygdala and memory: the hippocampus forms memories of any event, but the amygdala gives it the cognitive label of danger [3]. In a large-scale brain-imaging research study of 1,868 PTSD and non-PTSD patients across five countries with a variety of trauma ranging from war, child abuse, and sexual abuse, researchers have found that PTSD patients have smaller hippocampal volume than their non-PTSD counterparts. Taken together with the smaller amygdala volumes in PTSD patients found in the VA study, the smaller hippocampal volumes in PTSD patients indicate possible flaws in fear-processing, retrieval, and response in PTSD patients, which can explain the persistent avoidance of fear-related stimuli and recurring flashbacks of the corresponding traumatic event [3].
The prefrontal cortex (PFC), can be thought of as the overseer of all higher-level cognitive functions and reasoning. Responsible for decision-making, personality, and keeping stress-related and emotional reactions under control, the PFC is one of the last targets that receives signaling from the amygdala [5][3]. Functional imaging studies of the prefrontal cortex in patients with PTSD have also shown smaller PFC volumes compared to their non-PTSD counterparts [5]. Not only are PFC volumes smaller in cases of PTSD, but their activation when exposed to fear-provoking and emotion-provoking stimuli like combat scenes and trauma anecdotes are lower than in non-PTSD counterparts. This indicates that normal stress-inhibitory functions of the PFC may be compromised, allowing primitive fear-responses and elevated arousal and stress levels to go unabated. Taken altogether, research has shown that there are many differences in brain circuitry in patients with PTSD, and these differences are of special note when it comes to getting around treating it.
Our nervous system is not only a group of organs comprised of special tissue and cells, but also a complex network of biochemical pathways that influence our every function. In addition to physiological differences in cases of PTSD, biochemical differences have also been observed. The amygdala’s signals excite the hypothalamic-pituitary-adrenal (HPA) axis, the primary endocrine pathway that responds to stressors. In response to stress, the HPA axis secretes a series of hormones, most notably cortisol. The release of cortisol activates our sympathetic nervous system, which is responsible for symptoms of stress such as increased heart rate and blood pressure, increased breathing rates, and the release of epinephrine and norepinephrine [5]. The release of cortisol also provides negative feedback to the HPA axis, meaning that the more cortisol present, the less the HPA axis will be stimulated until the body is at rest again. In cases of PTSD, this negative feedback property in the HPA axis is compromised, either by lower-than-normal amounts of cortisol or flaws in the negative feedback mechanism, which explains the sustained elevated arousal states of PTSD patients. Decreased production of cortisol in some individuals have also been stated as a risk factor for those who have not yet developed PTSD [5].
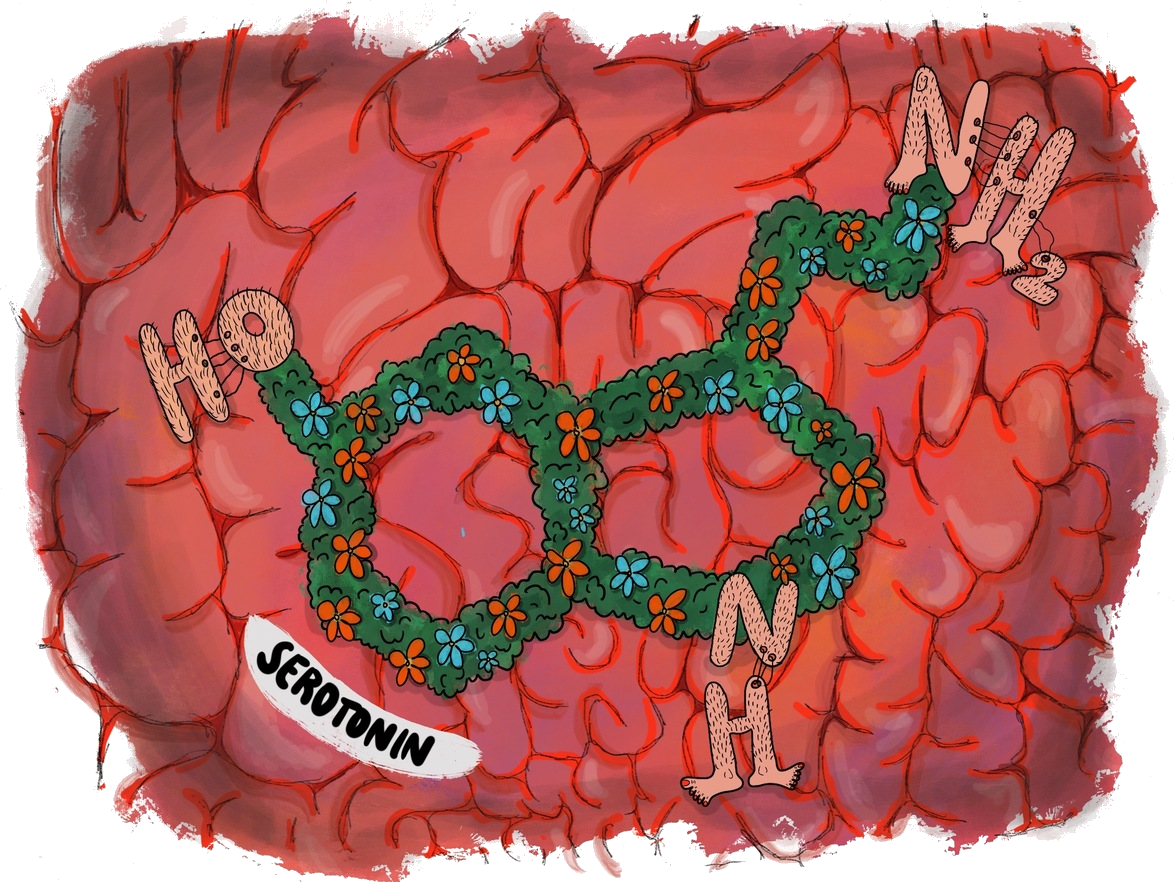
In addition to stress hormones, PTSD affects the release of neurotransmitters, chemicals that excite or inhibit other neurons to relay messages. These include neurotransmitters like dopamine, the neurotransmitter providing feelings of happiness and reward, and norepinephrine, the neurotransmitter responsible for stress responses such as increased blood pressure and heart rate. In cases of PTSD, both of these neurotransmitters are produced in higher-than-normal levels [5]. The increase of dopamine production likely interferes with the fear-conditioning and memory labelling between the amygdala and hippocampus, and the increased production of norepinephrine is responsible for the hyperarousal, startle response, and higher blood pressure and heart rate when faced with fear-inducing stimuli. PTSD also affects levels of another related neurotransmitter, called serotonin (5HT), which is also responsible for happiness and reward, as well as regulating hippocampus-to-amygdala communication [5]. PTSD patients have been found to have decreased 5HT levels, which may disrupt hippocampus-to-amygdala communication and contribute to heightened anxiety and fear responses [5].
Through research involving brain-imaging and neurochemical analysis, we can now see the plethora of effects that PTSD has on our brain: it affects one’s livelihood by modifying his or her brain structure and circuitry, as well as their nervous and endocrine system chemistry. These modifications manifest themselves as visible psychological symptoms, such as hyperarousal and hypervigilance, sustained elevated stress responses, and persistent avoidance toward fear-inducing stimuli.
The current consensus in treating PTSD is using psychotherapy and prescribing selective serotonin reuptake inhibitors (SSRIs). Psychotherapy methods may vary, but they all are centered around the traumatic event itself. SSRIs are medications that block the reuptake of serotonin, the neurotransmitter responsible for feelings of happiness, learning, and satisfaction, and amplifies its effect [5]. The issue with these methods is that they have high dropout rates and have a low effective response rate from the patient’s body. Traditional trauma-focused psychotherapy methods have a dropout rate of about 30 percent, which is attributed to a lack of trusting connections between patients and therapists [6]. On the other hand, SSRIs have only a 20-30 percent effective response rate in PTSD patients who’ve taken them, making SSRIs relatively ineffective as a treatment method [6].
“But the Doctor Says Drugs Are Bad”
Enter 3,4-Methylenedioxymethamphetamine (MDMA): a recreational drug popular among clubbers, music festivals, and rave culture. It is listed under Schedule I as part of the Controlled Substances Act, the strictest substance designation in the United States. Using MDMA to treat PTSD is controversial, but it has shown to be a promising breakthrough treatment method and is on the way to be approved for widespread use.
Studies on lab animals and humans have found MDMA’s effects to include increased feelings of happiness, euphoria, dissociation, friendliness, talkativity, and other general prosocial effects [7][8]. Adverse effects include muscle spasms, abnormally high heart rates, and seizures [7]. The prosocial effects can be attributed to the biochemical effects that MDMA has on our nervous system. The main effect of MDMA is the increase in serotonin levels in the brain [7]. Experiments conducted on frequent club-goers have also found drastic increases in cortisol and oxytocin levels after taking MDMA compared to clubbers who did not [9][10]. Serotonin and cortisol levels in PTSD patients are lower compared to non-PTSD patients; the administration of MDMA directly addresses this shortage.
Researchers propose that therapists exploit the prosocial and biochemical effects of MDMA to supplement existing trauma-focused psychotherapy methods. Not only does MDMA act as a supplement to the shortage of serotonin and cortisol in PTSD patients, the increased release of oxytocin after taking MDMA can help allay the patient-therapist mistrust which results in high dropout rates in psychotherapy, as it is attributed to facilitating social bonding and attachment [10][6].
Getting the Ball “Rolling” and the Cost of Relief
MDMA-assisted psychotherapy follows a series of fifteen therapy sessions, of which two to three involve the administration of MDMA. A three-session preparatory stage follows normal psychotherapy protocol, and is followed by one MDMA-assisted session lasting six to eight hours. A second and third MDMA-assisted session may take place at the therapist’s and patient’s discretion, but they must be spaced six to eight weeks apart with a few non-assisted sessions in between to avoid patients building a tolerance toward the drug. Each MDMA-assisted session has the patient be administered a 125 milligram dose of MDMA. This dose is relatively low compared to the average ecstasy dose taken by recreational users, where one to four ecstasy pills containing anywhere from 66 to 465 milligrams per pill are taken [2].
MDMA-assisted sessions always have extra precautions taken and emergency staff on hand. Sessions typically take place in a homely, calming area, with patient vitals constantly being monitored and cardiac life support ready in the case of overdose [6].
The first clinical trials using MDMA for PTSD happened in Spain in 2008, studying a small sample of female sexual assault victims with chronic, treatment-resistant PTSD, yielding positive results for the effectiveness of MDMA-assisted therapy [11]. The first U.S. study followed in 2011, and subsequent studies yielded positive results as well. In a study ran in 2013, sixteen PTSD patients who have undergone MDMA-assisted psychotherapy were assigned monthly follow ups for seventy-four months. All patients reported feeling relief from their symptoms and felt no adverse side effects, which is a testament to the long-term effectiveness of MDMA-assisted psychotherapy [12].
Though clinical trials have yielded promising results, the safety of MDMA-assisted psychotherapy is still under review. MDMA is a known teratogen, a biochemical agent that can cause birth defects and developmental difficulties. Studies involving mice embryos have found that MDMA use during early pregnancy can affect a child’s cardiac and neural development, making MDMA-assisted psychotherapy not a viable option for pregnant women [13].
Self-administration studies among rats and monkeys have shown that it is possible to build a dependence for MDMA [14][15]. This type of study involves a subject that must perform a specific behavior, like pushing one of two levers, for a certain dose MDMA to administered. In both rat and monkey experiments, rats and monkeys were quick to discriminate which of two levers would and would not administer MDMA, and progressively pulled MDMA-connected levers more frequently and with less time in between pulling, with the amount and frequency of pulls increasing with higher doses of MDMA [14][15]. This shows that patients undergoing MDMA-assisted psychotherapy are susceptible to MDMA dependence and drug-seeking behavior, which can in itself cause numerous added complications.
Another complication surrounding MDMA-assisted psychotherapy lies in its nomenclature. Though MDMA and “ecstasy” are commonly used interchangeably, they are not always the same thing. MDMA refers to a single chemical compound which is the focus of research, while the more colloquial “ecstasy” can refer to pure MDMA or drugs that contain MDMA and other compounds. Studies of the ecstasy market conducted in Europe have found that over fifty percent of ecstasy pills are not composed of pure MDMA and are combined with other drugs like amphetamine, ketamine, and mephedrone [16]. This raises concerns over drug purity and safety when conducting therapy sessions and makes it imperative that well-manufactured MDMA and not common “ecstasy” is used at all times.

Getting the “OK” to Get Patients High
MDMA-assisted psychotherapy is now under phase III clinical trials as of 2016, with current testing surrounding treatment efficacy and safety across a broad range of patients [6]. MDMA-assisted psychotherapy has also been granted “breakthrough therapy” status by the United States Food and Drug Administration (FDA), giving it priority for medical review and expedited treatment development [6]. This means that there is a great chance that we can see MDMA-assisted psychotherapy being offered to anyone who needs it in the near future. It is safe to say that MDMA has fought past its hard-partying reputation and social stigma. On a broader scale, the promise of MDMA-assisted psychotherapy for PTSD can pave the way for policy changes regarding other currently illegal drugs as more and more are showing promise in treating mental disorders. Psilocybin mushrooms, commonly known as “shrooms”, have been long demonized among contemporary society but have shown promise in treating clinical depression and are currently in phase II clinical trials [17]. Lysergic acid diethylamide (LSD), commonly known as “acid”, played a pivotal role in the Hippie counterculture movement and was thought to have mind-controlling properties that were tested illegally by the CIA in Project MKUltra [20]. Despite its troubled past, LSD has also recently shown promise in treating clinical depression [17][18]. MDMA itself has also found other potential applications in treating autism spectrum disorder and alcoholism [19]. With all the promise that many psychoactive drugs have, there is renewed interest in research regarding these drugs. However, with such tight regulations put forth by world governments, research is heavily restricted, which can be a huge missed opportunity in the world of medicine. It is very plausible for our current drug policies to change and allow more research, and we should make the effort to bring this issue to our policymakers’ attention. With such promising applications, it’s almost hard to keep telling our children that drugs are bad.
Before we all get our hopes too high, by no means is MDMA now deemed a “safe” substance, nor does its potential application in psychotherapy warrant recreational use. We should not all start taking MDMA thinking that it is good for us. Like any other psychoactive drug, MDMA has side effects and is unsafe in high doses. If MDMA-assisted psychotherapy passes as a bona fide medical treatment, we shouldn’t expect MDMA to be fully legalized either. The promise of MDMA for PTSD implies clinical use under professional supervision only and should not be undertaken by anyone else.
In regards to its use as PTSD treatment, some inquiries surrounding MDMA do appear. In research surrounding the neurochemical imbalances in PTSD patients and how some of those imbalances are compensated for by administering MDMA, the current MDMA-for-PTSD treatment model does little to maintain neurochemical balance. Future research could involve finding an adjunct to MDMA-assisted psychotherapy to maintain neurochemical balance in order to directly address physiological changes. Other future research could include finding alternatives to MDMA-assisted psychotherapy for pregnant women with PTSD who can’t take MDMA, and finding other mental disorders to apply MDMA-related treatment. Who would have known of the vast potential of certain substances in treating mental illness that has remained hidden under a shroud restrictive international policy, bad reputations, and social stigma. It is purely fallacious to take a “guilt by association” approach to MDMA. We are living in tenuous times, and as our world continues to change and our uneasiness continues to build, our perspectives must also change.
References
- Mithoefer, M. C., Feduccia, A. A., Jerome, L., Mithoefer, A., Wagner, M., Walsh, Z., et al. (2019). MDMA-assisted psychotherapy for treatment of PTSD: study design and rationale for phase 3 trials based on pooled analysis of six phase 2 randomized controlled trials. Psychopharmacology, 236(9), 2735–2745. doi:10.1007/s00213-019-05249-5.
- Meyer J. S. (2013). 3,4-methylenedioxymethamphetamine (MDMA): current perspectives. Substance abuse and rehabilitation, 4, 83–99. doi:10.2147/SAR.S37258
- W. Victor R. Vieweg, Demetrios A. Julius, Antony Fernandez, Mary Beatty-Brooks, John M. Hettema, Anand K. Pandurangi, Posttraumatic Stress Disorder: Clinical Features, Pathophysiology, and Treatment, The American Journal of Medicine, Volume 119, Issue 5, 2006, Pages 383-390, ISSN 0002-9343, https://doi.org/10.1016/j.amjmed.2005.09.027. (http://www.sciencedirect.com/science/article/pii/S0002934305008715)
- Morey, R. A., Gold, A. L., LaBar, K. S., Beall, S. K., Brown, V. M., Haswell, C. C., et al. (2012). Amygdala volume changes in posttraumatic stress disorder in a large case-controlled veterans group. Archives of general psychiatry, 69(11), 1169–1178. doi:10.1001/archgenpsychiatry.2012.50
- Sherin, J. E., & Nemeroff, C. B. (2011). Post-traumatic stress disorder: the neurobiological impact of psychological trauma. Dialogues in clinical neuroscience, 13(3), 263–278.
- Thal, S. B., & Lommen, M. (2018). Current Perspective on MDMA-Assisted Psychotherapy for Posttraumatic Stress Disorder. Journal of contemporary psychotherapy, 48(2), 99–108. doi:10.1007/s10879-017-9379-2
- Karlsen SN, Spigset O, Slørdal L. The dark side of ecstasy: neuropsychiatric symptoms after exposure to 3,4-methylenedioxymethamphetamine. Basic & Clinical Pharmacology & Toxicology. 2008 Jan;102(1):15-24. DOI: 10.1111/j.1742-7843.2007.00159.x.
- Bedi, Gillinder, & Kamilar-Britt, Philip. (2015). The prosocial effects of 3,4-methylenedioxymethamphetamine (MDMA): Controlled studies in humans and laboratory animals. Neuroscience and Biobehavioral Reviews., 57, 433-446.
- Wolff, K, Tsapakis, EM, Pariante, CM, Kerwin, RW, Forsling, ML, Aitchison, KJ (2012). Pharmacogenetic studies of change in cortisol on ecstasy (MDMA) consumption. J Psychopharmacol 26: 419–428.
- Wolff K, Tsapakis EM, Winstock AR, Hartley D, Holt D, Forsling ML, Aitchison KJ.Vasopressin and oxytocin secretion in response to the consumption of ecstasy in a clubbing population. J Psychopharmacol. 2006 May;20(3):400-10. doi: 10.1177/0269881106061514. PubMed PMID: 16574714.
- Bouso, C., Doblin, R., Farré, M., Alcázar, Á., & Gómez-Jarabo, G. (2008). MDMA-Assisted Psychotherapy Using Low Doses in a Small Sample of Women with Chronic Posttraumatic Stress Disorder. Journal of Psychoactive Drugs, 40(3), 225–236.
- Mithoefer, M. C., Wagner, M. T., Mithoefer, A. T., Jerome, L., Martin, S. F., Yazar-Klosinski, B., … Doblin, R. (2013). Durability of improvement in post-traumatic stress disorder symptoms and absence of harmful effects or drug dependency after 3,4-methylenedioxymethamphetamine-assisted psychotherapy: a prospective long-term follow-up study. Journal of Psychopharmacology, 27(1), 28–39. https://doi.org/10.1177/0269881112456611
- Meamar, R., Karamali, F., Sadeghi, H. M., Etebari, M., Nasr-Esfahani, M. H., & Baharvand, H. (2010). Toxicity of ecstasy (MDMA) towards embryonic stem cell-derived cardiac and neural cells. Toxicology in vitro : an international journal published in association with BIBRA, 24(4), 1133–1138. doi:10.1016/j.tiv.2010.03.005
- Fantegrossi, W., Woolverton, W., Kilbourn, M. et al. Behavioral and Neurochemical Consequences of Long-Term Intravenous Self-Administration of MDMA and Its Enantiomers by Rhesus Monkeys. Neuropsychopharmacol 29, 1270–1281 (2004). https://doi.org/10.1038/sj.npp.1300442
- Trigo, J.M., Panayi, F., Soria, G. et al. A reliable model of intravenous MDMA self-administration in naïve mice. Psychopharmacology 184, 212–220 (2006). https://doi.org/10.1007/s00213-005-0229-7
- Brunt, T. M., Poortman, A., Niesink, R. J., & van den Brink, W. (2011). Instability of the ecstasy market and a new kid on the block: mephedrone. Journal of Psychopharmacology, 25(11), 1543–1547. https://doi.org/10.1177/0269881110378370
- Schenberg, E. E. (2018). Psychedelic-Assisted Psychotherapy: A Paradigm Shift in Psychiatric Research and Development. Frontiers in Pharmacology, 9. doi:10.3389/fphar.2018.00733
- Liechti, M. Modern Clinical Research on LSD.Neuropsychopharmacol 42, 2114–2127 (2017). https://doi.org/10.1038/npp.2017.86
- Sessa, B., Higbed, L., & Nutt, D. (2019). A Review of 3,4-methylenedioxymethamphetamine (MDMA)-Assisted Psychotherapy. Frontiers in psychiatry, 10, 138. doi:10.3389/fpsyt.2019.00138
- Central Intelligence Agency. (1984, December 23). MK-Ultra/Mind control experiments | CIA FOIA (foia.cia.gov). Retrieved from https://www.cia.gov/library/readingroom/document/cia-rdp91-00901r000500150005-5

