Cultures and traditions continue to transcend borders as our world becomes more connected. With an increasing flow of novel practices, alternative medical treatments have become a popular choice for many people. Around the world, demand for acupuncture treatment is on the rise, and North America is no exception. Considered by the World Health Organization as a viable treatment for over 40 disorders, acupuncture has gained acceptance in the West [1]. Even so, the effectiveness and legitimacy of this form of treatment still raises questions in the scientific world. Practitioners and some scientists claim acupuncture has notable neurological and physiological effects, while other scientists have reservations due to poorly conducted research and the significant role of the placebo effect. With such polarizing views, there is a need for a better understanding of acupuncture’s history, benefits, and opposing skepticism.
Background on Acupuncture
Acupuncture has a rich history in traditional medicine. In China, it has been practiced for over 2,500 years, and there is historical evidence that this practice could date back even further [1][2]. The traditional Chinese rationale behind acupuncture draws from nature, burying its roots deep in spirituality [3]. Traditional theories view the human body as a vessel containing invisible meridians, through which qi–the life force–flows [2]. Acupuncture points, or acupoints, are openings to these meridians where needles can be inserted to affect the flow of energy [2]. In delivering acupuncture, practitioners either use manual needle manipulation or electroacupuncture, which involves electrical stimulation through inserted needles [4]. While the two techniques differ in their stimulatory modes, they are both considered acupuncture due to their common purpose: exciting acupoints.
Beyond the Chinese border, acupuncture has been leaving its mark in America since the early 1800s. Benjamin Franklin’s great-grandson, Benjamin Bache, published a translation by a French physician titled “Memoir on Acupuncture” and conducted his own successful experiments with acupuncture [5]. However, acupuncture failed to appeal to Americans until Nixon’s visit to China in 1971, when it was used to treat a member of the U.S. press corps who had undergone an appendectomy [2]. After the incident, interest in acupuncture surged as researchers began considering the treatment and physicians, as well as non-physicians, traveled abroad for training. Acupuncture steadily gained acceptance in parts of the American medical society [2].
In our current world, acupuncture research has come a long way, and the debate surrounding its efficacies is more interesting than ever. Analyses of acupuncture research have determined that acupuncture cannot treat every condition, and within the conditions it can treat, there are limits to what it can do [6]. For instance, a comprehensive review of acupuncture pain research shows acupuncture is effective for treating chronic back pain and headaches, but shows no benefit for treating cancer-related pain or labor pain, among many others [6]. A clear understanding of acupuncture’s effectiveness and limitations is important for avoiding unnecessary treatments, potentially adverse effects, or a waste of time and money.
Promising Effects
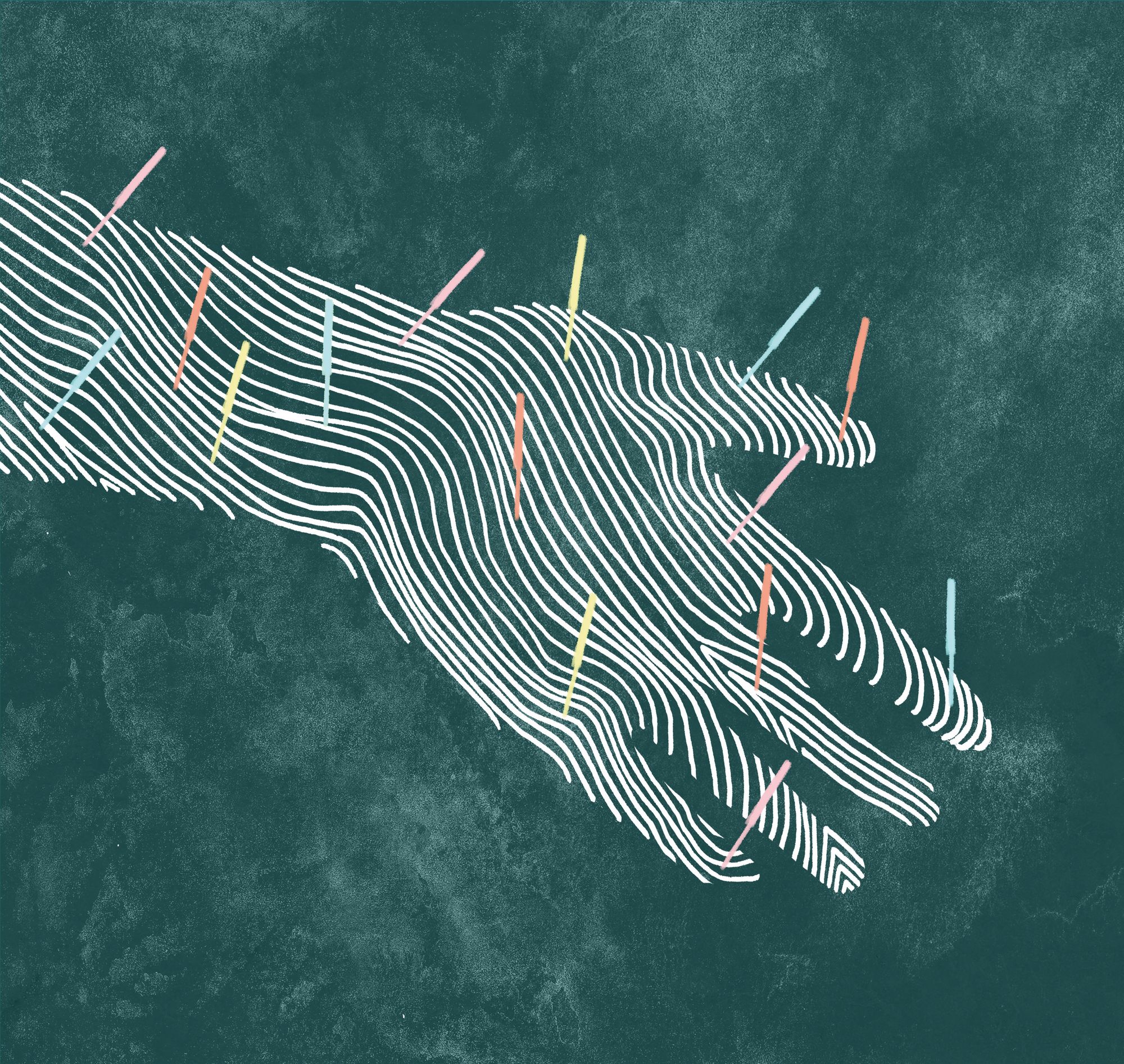
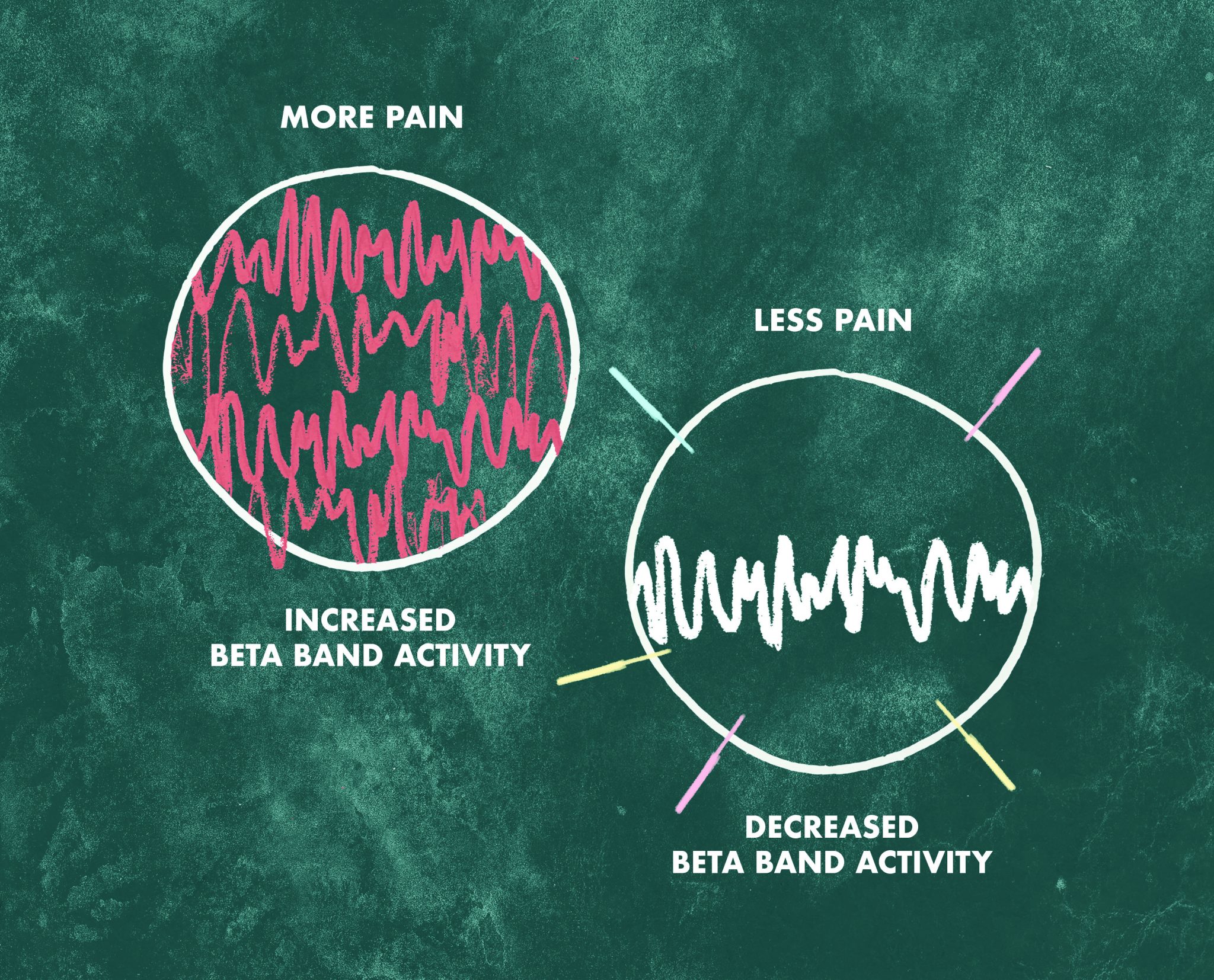
If acupuncture does not work to treat every condition, which ones does it benefit? Indeed, acupuncture has been shown to be effective in many cases. A study measuring the effects of acupuncture on the beta band, a type of brain wave associated with pain stimuli, showed a decrease in its power in several locations [7]. An increase in pain response is accompanied by elevation in beta band power, so observing the opposite effect suggests a mechanism through which acupoint stimulation can decrease pain [7].
While pain relief is one of acupuncture’s many applications, there is evidence that it can also help with a number of disorders [5]. One study in mice suggested that electroacupuncture might be useful in protecting neurons against MPTP toxicity [8]. A neurotoxic compound mimicking biochemical effects of Parkinson’s disease, MPTP can be used as a measure of acupuncture’s effectiveness against Parkinson’s in an experimental setting [9]. Mice injected with MPTP and treated with electroacupuncture stimulation for two weeks showed a decrease in a type of oxidative toxin as well as effective rescue of MPTP-affected neurons [8]. Electroacupuncture could be effective in retarding Parkinson’s onset at a mechanistic level. Furthermore, manual acupuncture has been shown to be extremely beneficial in improving motor functions when used as an addition to current medication [8][10].
In another study, researchers electrically targeted head and face acupoints to determine if there was any possibility of enhancing the efficacy of antidepressants [11]. They determined that acupuncture can augment antidepressants’ effectiveness, which could make it a good accompaniment to existing treatments for depressive disorders [11]. In a healthcare setting, this could expand treatment options for patients.
A study exploring acupuncture’s effects on Alzheimer’s disease and mild cognitive impairment (MCI) compared activity patterns of patients’ brains before acupuncture, during acupuncture, and ten minutes after needle removal [12]. During the initial resting state scans, MCI patients exhibited more activity in brain regions relating to cognition and memory than control patients, which was believed to be a compensative effect of their condition. MCI patients showed decreased activity in their resting state scans in areas associated with their mild cognitive impairment and disruptions in neuronal activity. During acupuncture, MCI patients showed more activation in regions with disruptions as well as additional activation in memory-related areas such as the frontal and temporal lobes. In contrast, patients with Alzheimer’s did not show activation in locations directly involved with Alzheimer’s disease. Through unknown mechanisms, acupuncture seemed to reverse the effect of MCI in certain disrupted brain regions while the same effect was not as clearly shown in the Alzheimer’s patients [12].
Scientific Skepticism
Despite the vast amount of research conducted on acupuncture, skepticism for the alternative treatment exists among the scientific community. One of the largest confounding factors is the placebo effect and treatment expectation. A study exploring the consequence of positive expectation found that both real acupuncture and the placebo treatment, where patients believed they were getting the real treatment, activated brain regions relating to the reward system [13]. Real acupuncture also showed effects in a region linked to emotions and internal equilibrium, as well as regions on the same side of the body as the site of needle insertion [13]. Most studies include a sham control trial of “fake” acupuncture, but the sham controls often fail to elucidate the role of placebo within the real treatment [14].
Critics also call into question the effect of publication biases on existing acupuncture research [15]. An analysis of publication origin relating to favoring results showed that studies from countries such as China, Taiwan, and Japan have a 100% publication preference toward acupuncture [15]. Despite being published in 1998, the article highlights an important trend that could impact how future research is viewed. Moreover, when it comes to improving quality, conducting a double-blind experiment in which neither participants nor researchers have knowledge of the participants’ experimental groups can be difficult. Even if the patient is blinded, practitioners would have knowledge of the treatment administered because of the physical nature of acupuncture, which is the case for sham versus real acupuncture control trials.
There is also a lack of consistency in research methods and reported results [16]. Acupuncture is used to treat a myriad of conditions, and for each condition, different practitioners use different combinations of acupoints. For example, investigations looking into acupuncture as a treatment for anxiety have used anywhere from one to 34 acupoints in their stimulation paradigms [17]. On top of that, there is also a range when it comes to the number of acupuncture sessions for each study [17]. With inconsistent methodologies, it becomes difficult to separate the effect of acupuncture from the effects of other experimental variables.
Beginning of an Exploration
As a form of treatment, acupuncture has survived centuries of societal and technological developments all while continuing to spread its influence. For such an intriguing mode of healing, there is still a great unknown when it comes to a definitive, generally agreed upon mechanism. Having thorough knowledge of acupuncture’s supporting evidence as well as critical skepticism is the first step in developing common ground from which future research can be conducted. While acupuncture is not an effective treatment for every illness, it is used to treat a wide range of conditions [6]. Acupuncture is cost-effective, easy to use, and its holistic views may appeal to many patients [17]. It is important, however, for future research to adopt better methodologies, address current criticisms, and fill in the gaps with current information on acupuncture. As of now, there are still many questions to answer: How does acupuncture work? What can it do and what can’t it do? Ultimately, how can it benefit patients seeking a complementary, alternative treatment? A better understanding of acupuncture will clarify not only how the procedure works but also refine the application of acupuncture for improving treatment options for patients and hopefully result in better healthcare outcomes.
References
- Chiu, JH. (2014) History of Acupuncture. In: Lin YC., Hsu EZ. Acupuncture for Pain Management. Springer, New York, NY. Retrieved from https://link.springer.com/chapter/10.1007/978-1-4614-5275-1_1
- Ernst, E., White, A. (May 1, 2004) A Brief History of Acupuncture . Rheumatology, Volume 43, Issue 5, 662-663. Retrieved from https://academic.oup.com/rheumatology/article/43/5/662/1788282/A-brief-history-of-acupuncture
- Lorenz K.Y. (November 3-5, 1997) What is Acupuncture? In: NIH Consensus Development Conference on Acupuncture, pages 19-23. Retrieved from https://www.liveoakacupuncture.com/wp–content/uploads/2015/09/NIHacupuncture.pdf#page=25
- Hai, H. (2013). Acupuncture : theories and evidence . Pages xvi, 16, 53-54. Retrieved from https://ebookcentral-proquest-com.offcampus.lib.washington.edu/lib/washington/reader.action?docID=1168154&ppg=1
- Dielh, D., Kaplan, G., Coulter, I., Glik, D., Hurwitz, E. (1997) Use of Acupuncture by American Physicians. In: The Journal of Alternative and Complementary Medicine, Volume 3, pages 119-126. Mary Ann Liebert, Inc. Retrieved from http://online.liebertpub.com.offcampus.lib.washington.edu/doi/pdf/10.1089/acm.1997.3.119
- Ma, Y., Dong, M., Zhou, K., Mita, C., Liu, J., Wayne, P. (December 14, 2016) Publication Trends in Acupuncture Research: A 20-Year Bibliometric Analysis Based on PubMed. PloS ONE, 11(12), e0168123. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5156436/
- Asghar, A., Johnson, R., Woods, W., Green, G., MacPherson, H., Lewith, G. (November 16, 2012) Oscillatory neuronal dynamics associated with manual acupuncture: a magnetoencephalography study using beamforming analysis . In: Frontiers on Human Neuroscience. Retrieved from http://europepmc.org/articles/PMC3522113
- Wang, H., Pan, Y., Xue, B., Wang, X., Zhao, F., Jia, J., Liang, X., Wang, X. (2011) The Antioxidative Effect of Electro-Acupuncture in a Mouse Model of Parkinson’s Disease. PLOS ONE 6(5): e19790. Retrieved from https://doi.org/10.1371/journal.pone.0019790
- Blum, D., Torch, S., Lambeng, N., Nissou, MF., Benabid, AL., Sadoul, R., Verna, JM. (October 2001) Molecular Pathways Involved in the Neurotoxicity of 6-OHDA, dopamine and MPTP: Contribution to the Apotopic Theory in Parkinson’s Diease. In: Progress in Neurobiology, Volume 65, Issue 2, pages 135-172. Retrieved from http://www.sciencedirect.com/science/article/pii/S030100820100003X
- Xiao, R. (December 2008) Fifty Cases of Parkinson’s Disease Treated by Acupuncture Combined with Madopar. In: Journal of Traditional Chinese Medicine, Volume 28, Issue 4, pages 255-257. Retrieved from: www.sciencedirect.com.offcampus.lib.washington.edu/science/article/pii/S0254627209600042
- Zhang. ZJ., Ng, R., Man, SC., Li, T., Wong, W., Tan, QR., Wong, K., Chung, KF., Wong, MT., Tsang, WK., Yip, K., Ziea, E., Wong, V. (January 6, 2012) Dense Cranial Electroacupuncture Stimulation for Major Depressive Disorder – A Single-Blind, Randomized, Controlled Study. In: PloS ONE, 7(2). Retrieved from http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0029651
- Wang, Z., Nie, B., Li, D., Zhao, Z., Han, Y., Song, H., Xu, J., Shan, B., Lu, J., Li, K. (August 20, 2012) Effect of Acupuncture in Mild Cognitive Impairment and Alzheimer Disease: A Functional MRI Study. In: PLOS ONE 7(8), e42730. Retrieved from http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0042730
- White, P., Pariente, J., Frackcowiak, R., Lewith, G. (March 2004) The Neurological Pathways Involved in the Treatment of Pain by Acupuncture in Different Belief and Expectancy Contexts. In: Focus on Alternative and Complementary Therapies, Volume 9, Issue s1, page 58. Retrieved from http://onlinelibrary.wiley.com.offcampus.lib.washington.edu/doi/10.1111/j.2042-7166.2004.tb04579.x/full
- Ernst, E., White, A, (November 9, 1998) Acupuncture for Back Pain: A Meta-analysis of Randomized Controlled Trials. Arch Intern Med. Retrieved from: https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/210231
- Vickers, A., Goyal, N., Harland, R., Rees, R. (1998) Do Certain Countries Produce Only Positive Results? A Systematic Review of Controlled Trials. Retrieved from: http://www.dcscience.net/Vickers_1998_Controlled-Clinical-Trials.pdf
- Riet, G., Kleunen, J., Knipschild, P. (March 22, 1990) Acupuncture and Chronic Pain: A Criteria-Based Meta-Analysis. In: Journal of Clinical Epidemiology, Volume 43, Issue 11, pages 1191-1199. Retrieved from: https://ac-els-cdn-com.offcampus.lib.washington.edu/089543569090020P/1-s2.0-089543569090020P-main.pdf?_tid=c48ae340-eced-11e7-adba-00000aab0f01&acdnat=1514589341_fa41b053305ad55c9fa1cd8525dc7e52
- Errington-Evans, N. (April 2012) Acupuncture for Anxiety. CNS Neuroscience & Therapeutics, Volume 18, Issue 4, pages 277-284. Retrieved from http://onlinelibrary.wiley.com.offcampus.lib.washington.edu/doi/10.1111/j.1755-5949.2011.00254.x/full
