Introduction
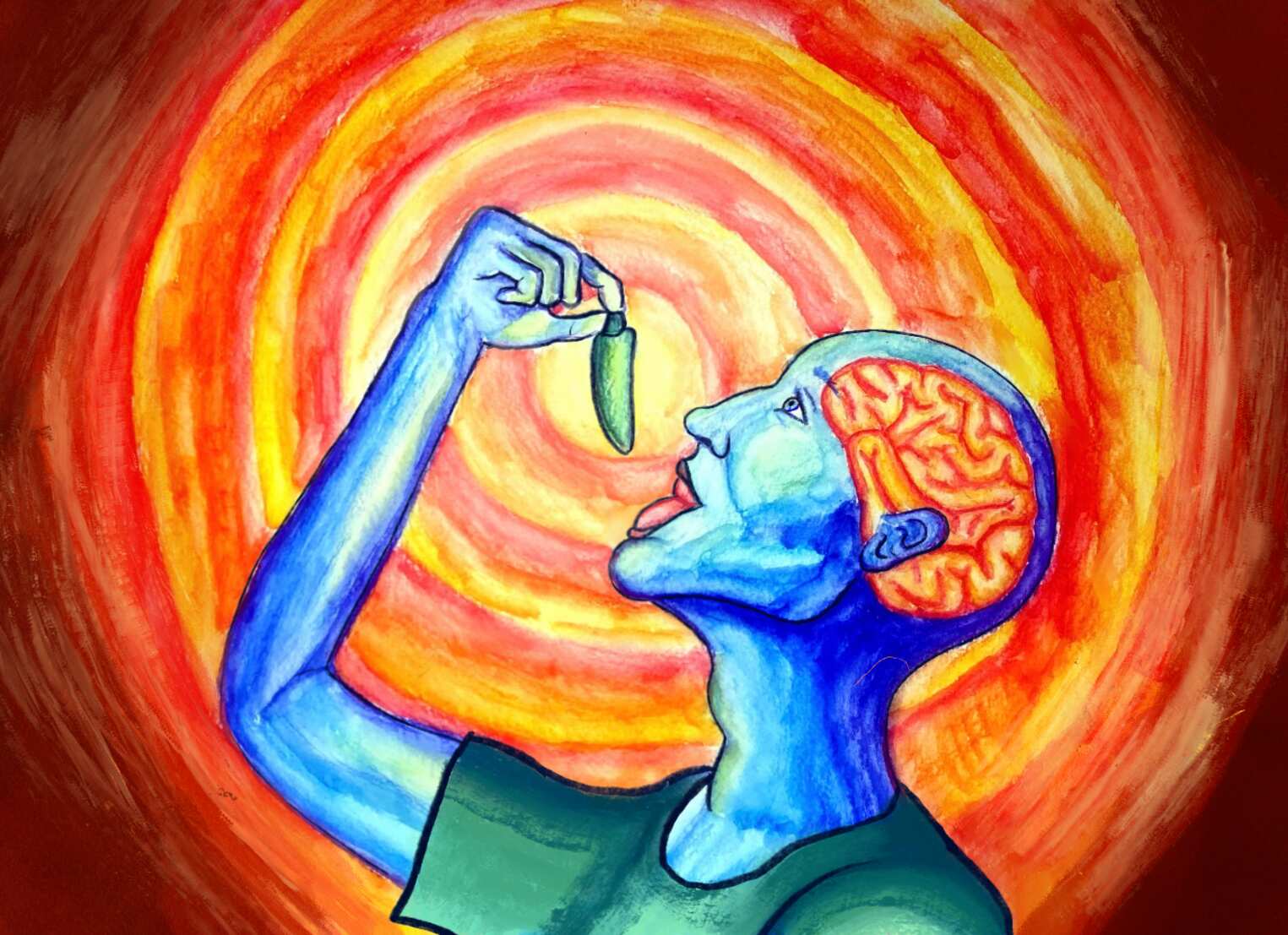
Imagine you’re out at dinner with a friend, excitedly awaiting your dish. Your food comes, and you take a big bite. Suddenly, you feel your throat heat up, your eyes fill with tears, and your hands become super sweaty. You manage to squeeze out the words “too spicy” before chugging down your entire glass of water in hopes of washing the burning sensation away. Your friend then tries your food, but somehow, they’re perfectly fine. People react differently to spices due to factors such as cultural diets. Different cultures use varying resources to achieve a range of spice levels: European dishes favor spices like oregano and saffron, Indian meals are rich in turmeric and chili powder, South American cuisine makes use of a wide variety of peppers, from sweet banana peppers to fiery jalapeños. However, these spices don’t just boost the taste factor of the food we eat. Evidence suggests that food with spices improves brain cell longevity and delays symptoms of cognitive disease. Understanding how spices impact the body is one way in which we can increase our knowledge of what a healthy diet looks like.
So what exactly counts as a spice? A spice is a seasoning ingredient that comes from a seed, fruit, root, or bark of a plant. Seasonings made from leaves are termed herbs, though they fall under the spice umbrella when dried and grounded [1]. Apart from adding to the flavor of a meal, these spices may be used for medical purposes in the future. Recent research demonstrates where exactly the brain detects spice, how the properties of spice impact the microbes that connect the gut and the brain, and what effects spices have on cognitive function.
Spice and the Autonomic Nervous System
When molecules of spicy food are detected by receptors on the tongue, they send a signal to the brain to activate the autonomic nervous system, a component of the body’s response mechanism responsible for involuntary actions involving heart rate and blood flow [2]. These processes result in reactions such as red cheeks, teary eyes, and sweaty hands. The parts of a cell responsible for receiving these and other signals are called receptors. One of these receptors, transient receptor potential vanilloid 1 (TRPV1), detects pain [2]. Molecules of capsaicin, which gives chili peppers their spice, bind to TRPV1, and the signal is passed through neural pain circuitry to the brain. Researchers at Osaka University and the National Institute of Physiological Sciences in Japan performed a study in 2016 determining where in the brain spice is processed and what role it plays in bodily reactions [2]. In the study, 20 subjects between the ages of 20 and 36 were presented with three different solutions in separate tubes: capsaicin, artificial saliva, and a salty solution made of sodium chloride (NaCl). An fMRI scanner was used to measure brain response to stimuli during each trial. These scans measure the changes in blood flow as a correlate of brain activity. They showed that the gustatory cortex, the part of the brain that processes taste, was activated by the capsaicin. The reason your body has this aversive reaction to capsaicin is because it triggers the pain pathway. The body thinks the mouth is burning, so it thermoregulates and protects sensitive membranes, resulting in sweaty palms and watery eyes, respectively, to save itself from danger. Evidently, the gustatory cortex is involved in the perception of spice-induced pain, even though spice itself is not a taste. The researchers also measured fingertip temperature to investigate the dilation of blood vessels, which has been shown to occur as a part of autonomic activity. Specifically, they found that fingertip temperature was higher after tasting capsaicin than after tasting either the artificial saliva or the NaCl solution [2]. After analysis of the fingertip temperatures, researchers concluded that capsaicin plays a role in autonomic responses, causing the typical reactions to spice. In conjunction with the fMRI data, researchers concluded that spice is first processed in the gustatory cortex and results in subsequent activation of autonomic activity, suggesting a link between the two [2]. Discovering where in the brain we detect spicy foods and how they stimulate the autonomic nervous system allows a deeper understanding of the role of spice in physiological responses throughout the entire body.
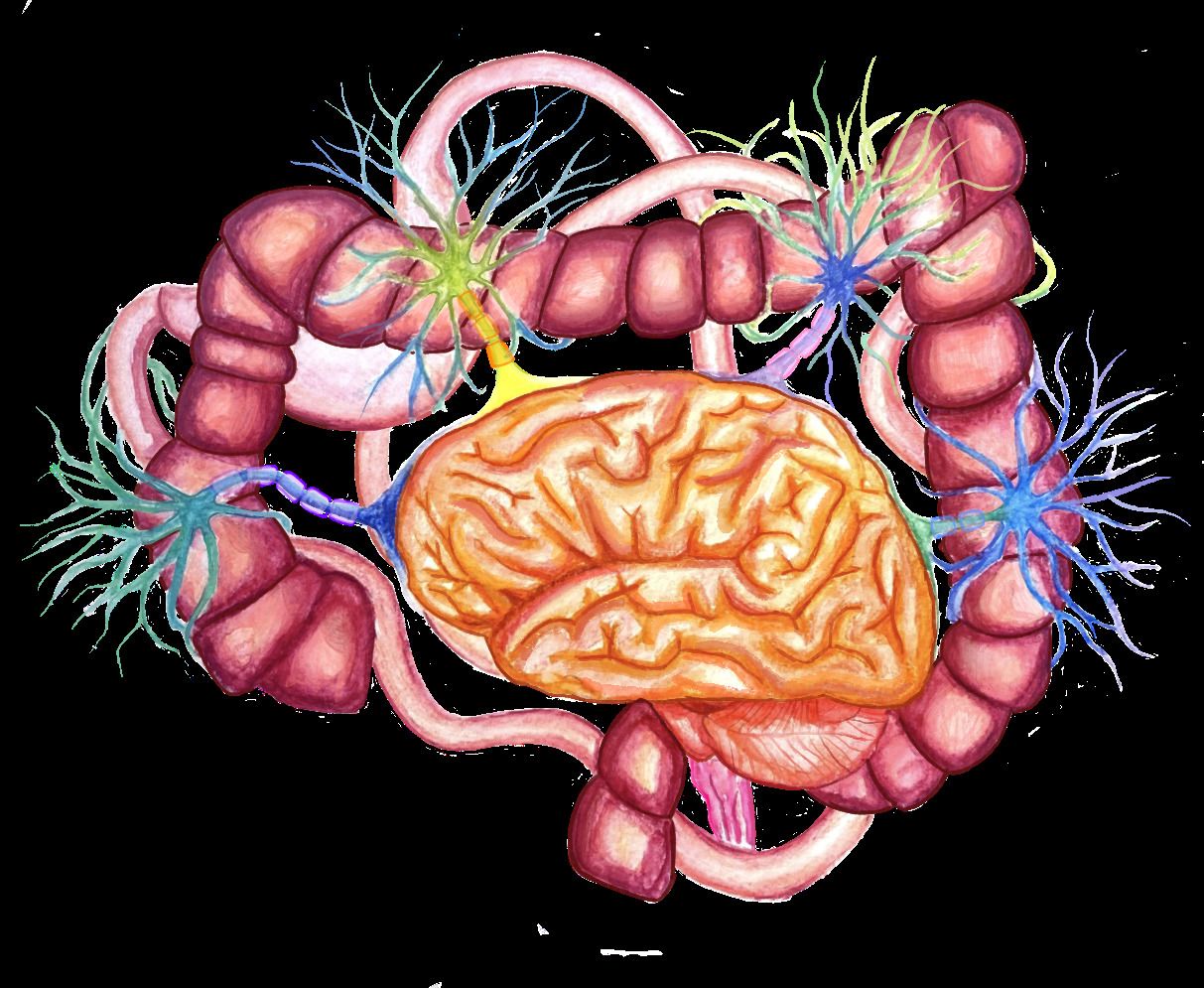
Spice and the Gut-Brain Axis
One such region that is impacted by spice is the gut. Bacteria, viruses, yeast, and fungi are jointly known as the gut microbiome. While some bacteria in the gut are helpful in fighting off infections and controlling inflammation in the body, there are many types of harmful bacteria that can be detrimental to the health of organs, including the brain. The gut and the brain are directly connected through the gut-brain axis, which is the network of signaling pathways that connects the nervous system and the gastrointestinal tract [3]. Nerves, hormones, and immune cells traveling along this axis transmit information between the brain and digestive system. This suggests inflammation and infection of the gut are connected to many mental, behavioral, and neurological problems because bacteria alter nutrient levels and influence the release of proteins that stimulate neurotransmitters within the digestive tract. Then, these neurotransmitters send signals to the brain that stimulate the release of hormones related to sleep, stress, pain reception, and blood regulation, ultimately altering behavior. Harmful bacteria release toxins that target the brain during infection by blocking the neurotransmission of a signal and altering neural circuits [4]. If neurons aren’t able to transmit signals properly, the nervous system can’t function well. Antibiotics combat harmful bacteria by blocking processes in the bacteria to stop their replication. However, bacteria can evolve and develop defense mechanisms against antibiotics, becoming antibiotic resistant. Fortunately, spices have antimicrobial properties that prevent the growth of harmful bacteria which could damage the gut-brain axis, making spices beneficial for not just the gut, but also the brain.
Many studies have been conducted to test the abilities of different spices on various strands of bacteria. One such study at Monastir University in Tunisia tested the effects of carvacrol and thymol, the primary oils in oregano and thyme, respectively, on bacterial strains [5]. Oregano and thyme are herbal spices added to foods to give them a more aromatic flavor; some of their most common uses are tomato-based pizza and pasta sauces, vinaigrettes, and meat marinades. Researchers found that these spices enhance the susceptibility of harmful bacteria to antibiotics by inhibiting the transport proteins that move bacteria into the host cell. Bacterial strains were incubated at a controlled temperature, after which thymol and carvacrol were dissolved and added in increasing concentrations. The researchers used an ethidium bromide (EtBr) efflux assay, a method that measures the fluorescence of the bacteria to determine efflux pump function in cells. Researchers chose to use EtBr in this specific study because it is a fluorescent dye and therefore provides a clear visual of the functionality of bacterial pumps. A higher fluorescence indicates more EtBr molecules are trapped within the cell, meaning lower cell function caused by EtBr damaging the mitochondrial DNA. Analysis revealed that the presence of carvacrol and thymol increased fluorescence, suggesting they prevented the bacteria from regulating their internal environment [5]. By blocking pumps in bacteria, carvacrol and thymol trap waste molecules in bacterial cells, reducing their viability and causing them to die off. Taking advantage of carvacrol and thymol’s ability to decrease bacterial cell counts can help fight off harmful bacteria in the gut. Because this study was conducted in vitro, meaning in a dish rather than a living organism, it’s hard to know the exact impact carvacrol and thymol would have on the gut-brain axis. However, this research demonstrates the fundamental anti-bacterial properties of spices that can be used as foundations for further testing within living organisms [5]. Another spice with antibacterial properties is clove, a versatile spice that is used to prepare a variety of foods and beverages such as meat, chai, mulled wine, pumpkin pie, and fruit pastries. In addition to adding flavor, clove is useful in fighting off bacteria [6]. Clove increases lysozyme activity in rats injected with different bacterial strains to expedite bacterial cell death [6]. Lysosomes are organelles that remove waste and break down toxins in a cell, so by increasing their function, clove increases the rate at which bacteria can be killed. In one study, researchers injected different bacterial strains to 40 rats, treated them with clove, and analyzed their blood samples over the course of four weeks [6]. The scientists concluded that clove increases lysosome function, which reduces the capability of harmful bacterial cells to damage a host cell. This gives the immune system more time to react and kill the bacteria in a localized area of the body before it spreads and impacts multiple organs and neurons. These antimicrobial properties of spices are relevant because with increasing antibiotic resistance, natural remedies like spice consumption are more and more advantageous in preventing and curing infections in the gut. While these treatments are promising, the amount of spice needed to produce desired results is yet to be determined [6]. Overall, spices have properties that combat harmful bacteria by stopping their growth, which is likely to preserve the gut-brain axis and protect the brain in humans.
The Impact of Spices on Cognitive Diseases and Tumors
Due to their ability to inhibit bacterial cell growth, spices may also improve cognitive function and delay symptoms of cognitive diseases. One such disorder is Parkinson’s Disease (PD), a disease in which the brain cells that make dopamine slowly lose function. This results in muscular dysfunction, tremors in the limbs, slowed movements, and cognitive deficiencies such as slower mental processing, memory issues, and language abnormalities. Dopamine is a neurotransmitter that controls flow of information in the front parts of the brain, so the decline of dopamine leads to cognitive disorders. A 2016 study at the Central Food Technology Research Institute in India using the rotenone (ROT) model of PD tested how cinnamon and cumin affected the onset of symptoms in flies [7]. Rotenone is a compound that causes oxidative damage and leads to neuron death, producing symptoms like those of PD. Flies are used for rotenone models of PD because they have distinct dopamine-related neuronal clusters, and they exhibit dopamine-dependent behaviors similar to humans. The flies, which had ROT-induced neurotoxicity, were fed food with cinnamon or cumin. Their movements and oxidative stress were measured by calculating the total count of reactive oxygen species like nitric oxide and superoxide dismutase, which are markers of oxidative stress because they cause damage to DNA, RNA, and cells as a whole. Scientists chose to measure these quantities because PD results in loss of movement control and can lead to higher oxidative stress, so monitoring how cinnamon and cumin affected these symptoms in flies can be useful in advancing ongoing research on PD. In an experiment testing the tendency of flies to move against gravity and an experiment measuring the time it took for flies to cross a certain distance, both the cinnamon and cumin treatments showed a significant delay in the onset of movement loss. Additionally, both spices reduced oxidative stress in the flies by supplying flies with antioxidants, compounds that remove the harmful reactive oxidative species [7]. This suggests that cinnamon and cumin delay symptoms of PD that cause neurotoxicity. There is currently no cure for PD, so the possibility of discovering a cure based on spice usage will open a gateway to potential alternative therapies.
Equally important are studies of spices on Alzheimer’s Disease (AD), a disorder that damages brain cell connections and results in memory loss and confusion. Both PD and AD are progressive disorders, meaning symptoms get worse over time, and both diseases are associated with brain cell damage in the hippocampus, the region of the brain that plays a role in learning and memory [8]. A 2020 study also at the Central Food Technology Research Institute in India tested the neuroprotective effect of spice oleoresins on memory and cognitive impairment in rats [9]. Oleoresins are a combination of spice and oil, with a flavor many times stronger than the original spice. The study used rats with induced AD caused by scopolamine, which is a drug that decreases learning and memory in behavioral studies. Rats were divided into six groups and each group was given a different drug treatment. Three of the groups were the control group, scopolamine alone, and scopolamine with donepezil group, which represented the current AD treatment medication. The other three treatment groups were scopolamine with an assortment of spices, namely pepper, turmeric, and chili. Treatments were administered for two weeks. Behavioral abilities were tested twice during the two-week period by putting the rats in a water maze, a test of memory where rats are placed into a four-quadrant pool of water and swim to a hidden escape platform. In this test, both the escape time as well as time per quadrant were measured. After two weeks, the brain tissue of the rats were harvested for analysis. Neuronal loss and degeneration of the hippocampus region of the brain were reported throughout the study. Moreover, in both the behavioral and neurological observations, treatments with spice oleoresins showed neuroprotection and improvement in hippocampal damage. The chili oleoresin was the most effective in reducing water maze escape time, suggesting enhanced memory, while the pepper oleoresin protected against hippocampal damage most significantly. The researchers concluded that chili, pepper, and turmeric were all impactful on the behavioral and neurological capabilities of the rats [9]. Therefore, eating foods with pepper, chili, and turmeric may be beneficial for the brain. The oleoresins of these spices can potentially be used in the treatment of neurological diseases like AD and PD, as it reduces symptoms of these disorders in animal testing models that mirror the onset of symptoms in humans.

Along with neurodegenerative disorders, another type of disease that spices may be useful for is certain types of cancer, like medulloblastoma (MB), the most common type of cancerous brain tumor in children. A study by researchers at the Medical College of Wisconsin demonstrated that curcumin, the active compound in turmeric, inhibited the ability of MB cells to clone themselves [10]. Researchers acquired the cells that form the MB tumors. They were seeded and treated with different concentrations of curcumin, and cell proliferation was assessed after four days. The results showed that curcumin induced apoptosis, meaning cell death, in two ways. First, the spice stops the function of genes that block apoptosis and allow cancer cells to survive. Additionally, curcumin increases the activity of caspase-3, an enzyme that controls cell death. By prohibiting the genes and increasing enzyme activity, curcumin significantly contributed to the death of the tumor cells [10]. Medulloblastoma tumors are only one type of brain tumor, but understanding how spices could be effective against them could be beneficial in treating other types of cancers as well.
A prior study in 2013 at the Changhua Christian Hospital testing capsaicin’s effect on KB cancer cells showed the same results [11]. A similar approach was utilized and showed that exposure of cells to capsaicin inhibited cell growth. Cells were given concentrations of capsaicin, and the number of living versus dead cells was calculated after 24, 48, and 72 hours, with an overall decrease in the number of cells throughout the study. This experiment showed that spices stimulated a typically inactive molecule called procaspase, which can damage mitochondrial membranes by creating holes in them, preventing proper regulation of what can flow in and out of the mitochondria. The study revealed that just like curcumin, capsaicin induced cell death by permeabilizing the mitochondrial membrane and activating caspase enzymes [11]. In both the medulloblastoma tumor and KB cancer cell studies, the spices functioned similarly in that they both increased caspase activity to promote apoptosis. Throughout both of these studies, spices have consistently demonstrated that their ability to reduce cognitive impairment symptoms and kill harmful cells in different types of tumors makes them worth researching in relation to human health.
Conclusion
With the results obtained in these studies, we can better comprehend the therapeutic implications of spice. Knowing where in the brain spice is detected is groundbreaking in recognizing how different food stimuli activate the brain and autonomic nervous system. These physiological responses reveal how what we eat can impact the gut-brain axis and what role spices could play in cognitive diseases. Future research can build off of these studies as scientists continue to test how traditional health practices like spice usage can come together with modern medicine to create optimal treatments. With the potential usage of spices in healthcare, it’s important to be mindful of the ethical ramifications that come with it. For instance, while a spice-based treatment could help patients with cognitive diseases, it could also negatively impact people living in countries that produce the spices because of increased global demand for the plant being used and higher prices of once-abundant products. Additionally, legal parameters like medical patents could come into play if pharmaceutical companies start to compete over limited spice resources, which could happen at the expense of people who had used spices for traditional purposes beforehand. The potential application of spice to particular medical treatments is full of research opportunities as well as ethical boundaries that must be considered while testing and utilizing the spices. But for now, the next time you enjoy food with any sort of spice, whether it be a bowl of Cinnamon Toast Crunch cereal or firecracker chicken with a side of Carolina Reaper peppers, you can think about what’s going on in your brain.
References:
- Sherman, P.W., Billing, J. (1999). Darwinian Gastronomy: Why We Use Spices: Spices taste good because they are good for us. BioScience, 49(6), 453–463. https://doi.org/10.2307/1313553.
- Kawakami, S., Sato, H., Sasaki, A.T., Tanabe, H.C., Yoshida, Y., Saito, M., Toyoda, H., Sadato, N., Kang, Y. (2016) The Brain Mechanisms Underlying the Perception of Pungent Taste of Capsaicin and the Subsequent Autonomic Responses. Frontiers in Human Neuroscience, 9(720). doi: 10.3389/fnhum.2015.00720.
- Cryan, J.F., O'Riordan K.J., Cowan, C.S.M., Sandhu, K.V., Bastiaanssen, T.F.S., Boehme, M., Codagnone, M.G., Cussotto, S., Fulling, C., Golubeva, A.V., Guzzetta, K.E., Jaggar, M., Long-Smith, C.M., Lyte, J.M., Martin, J.A., Molinero-Perez, A., Moloney, G., Morelli, E., Morillas, E., O'Connor, R., Cruz-Pereira, J.S., Peterson, V.L., Rea, K., Ritz, N.L., Sherwin, E., Spichak, S.,Teichman, E.M., van de Wouw, M., Ventura-Silva, A.P., Wallace-Fitzsimons, S.E., Hyland, N., Clarke, G., Dinan, T.G. (2019). The Microbiota-Gut-Brain Axis. American Physiological Society, 99(4), 1877-2013. Doi: 10.1152/physrev.00018.2018.
- Yang, N.J., Chiu, I.M. (2017). Bacterial Signaling to the Nervous System through Toxins and Metabolites. Journal of Molecular Biology, 429(5), 587-605. doi: 10.1016/j.jmb.2016.12.023.
- Miladi, H., Zmantar, T., Chaabouni, Y., Fedhila, K., Bakhrouf, A., Mahdouani, K., Chaieb, K. (2016). Antibacterial and efflux pump inhibitors of thymol and carvacrol against food-borne pathogens. ScienceDirect, 99(15), 95-100. doi : 10.1016/j.micpath.2016.08.008.
- Nassan, M.A., Mohamed, E.H., Abdelhafez, S., Ismail, T.A. (2015). Effect of clove and cinnamon extracts on experimental model of acute hematogenous pyelonephritis in albino rats: Immunopathological and antimicrobial study. International Journal of Immunopathology and Pharmacology, 28(1), 60-68. doi: 10.1177/0394632015572075.
- Sriranjini, V., Rao, S.V., Muralidhara, M., Rao, G.M., Rajini, P.S., Muralidhara, P.S., Rajini, P. (2016). Neuromodulatory Potential of Aqueous Extracts of Cumin, Cinnamon: Evidence from Rotenone Model in Drosophila: Implications to Parkinson's Disease. International Journal of Neurology Research, 2(3), 1-11. Doi: 10.17554/j.issn.2313-5611.2016.02.60.
- Rao, Y.L., Ganaraja, B., Murlimanju, B.V., Joy, T., Krishnamurthy, A., Agrawal, A. (2022). Hippocampus and its involvement in Alzheimer's disease: a review. 3 Biotech, 12(55). doi: 10.1007/s13205-022-03123-4.
- Rajashri, K., Mudhol, S., Serva, P. M., Borse, B.B. (2020) Neuroprotective Effect of Spice Oleoresins on Memory and Cognitive Impairment Associated with Scopolamine-Induced Alzheimer's Disease in Rats. ACS Omega, 5(48), 30898-30905. doi: 10.1021/acsomega.0c03689.
- Bangaru, M.L.Y., Chen, S., Woodliff, J., Kansara, S. (2010). Curcumin (Diferuloylmethane) Induces Apoptosis and Blocks Migration of Human Medulloblastoma Cells. Anticancer Research, 30(2) 499-504.
- Lin, C.H., Lu, W.C., Wang, C.W., Chan, Y.C., Chen, M.K. (2013) Capsaicin induces cell cycle arrest and apoptosis in human KB cancer cells. BMC Complementary Medicine and Therapies, 13(46). doi: 10.1186/1472-6882-13-46.