Chronic stress affects many Americans. Most recently, a major cause of stress in the United States has been the COVID-19 pandemic, with nearly eight in ten Americans reporting that the pandemic is “a significant source of stress” in their lives, according to the APA’s 2020 report [1]. Stress causes a number of physiological and psychological effects, including cold sweat, indigestion, restlessness, weakened immune system, increased heart rate, faster breathing, and poor concentration and memory [2]. These effects can feel intangible and overwhelming, but by understanding the mechanisms underlying stress, we can gain control over it.
When we talk about stress, we often describe it as an abstract force affecting us, but the stress response is a function of our nervous system to help us survive dangerous situations [3]. It prioritizes sending resources to the areas that are critical at that moment, decreasing resources used for long-term processes. Over the millennia, stressors have changed significantly from the threat of a predator to the constant pressure of deadlines. However, our stress response hasn’t evolved to keep up with the stress we experience, so the functions that are meant to keep us alive are actually maladaptive to modern stress. Modern stress tends to be less intense but longer lasting. Instead of having a physically dangerous situation lasting for hours, we have deadlines or stressful social situations that can last for days, months, or even years without break. This is what's known as chronic stress, which may cause serious damage like heart disease, diabetes, and the atrophy of certain brain areas. There is hope, however, as several methods of stress release have been shown to help reduce the effects of long-term stress [3].
Two of the main structures that make up the stress response are the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). These are two separate branches of the autonomic nervous system (ANS), which is responsible for involuntary functions like regulating heart rate and digestion [4]. Generally speaking, the SNS is involved in stressful situations like taking an exam and the PNS is involved with daily activities like digestion [2]. As seen in the diagram of the PNS and SNS, the two systems act on many of the same organs but cause a variety of effects. You’ll also notice that the PNS branches out from the spinal cord earlier than the SNS. This is because it’s more important for SNS signals to travel quickly. The two nervous systems also use different neurotransmitters: the SNS uses norepinephrine while the PNS uses acetylcholine. The two neurotransmitters can bind to different receptors that can then cause opposite effects in the cells they are part of. This is how the two nervous systems can act on many of the same organs and cause different effects [2].
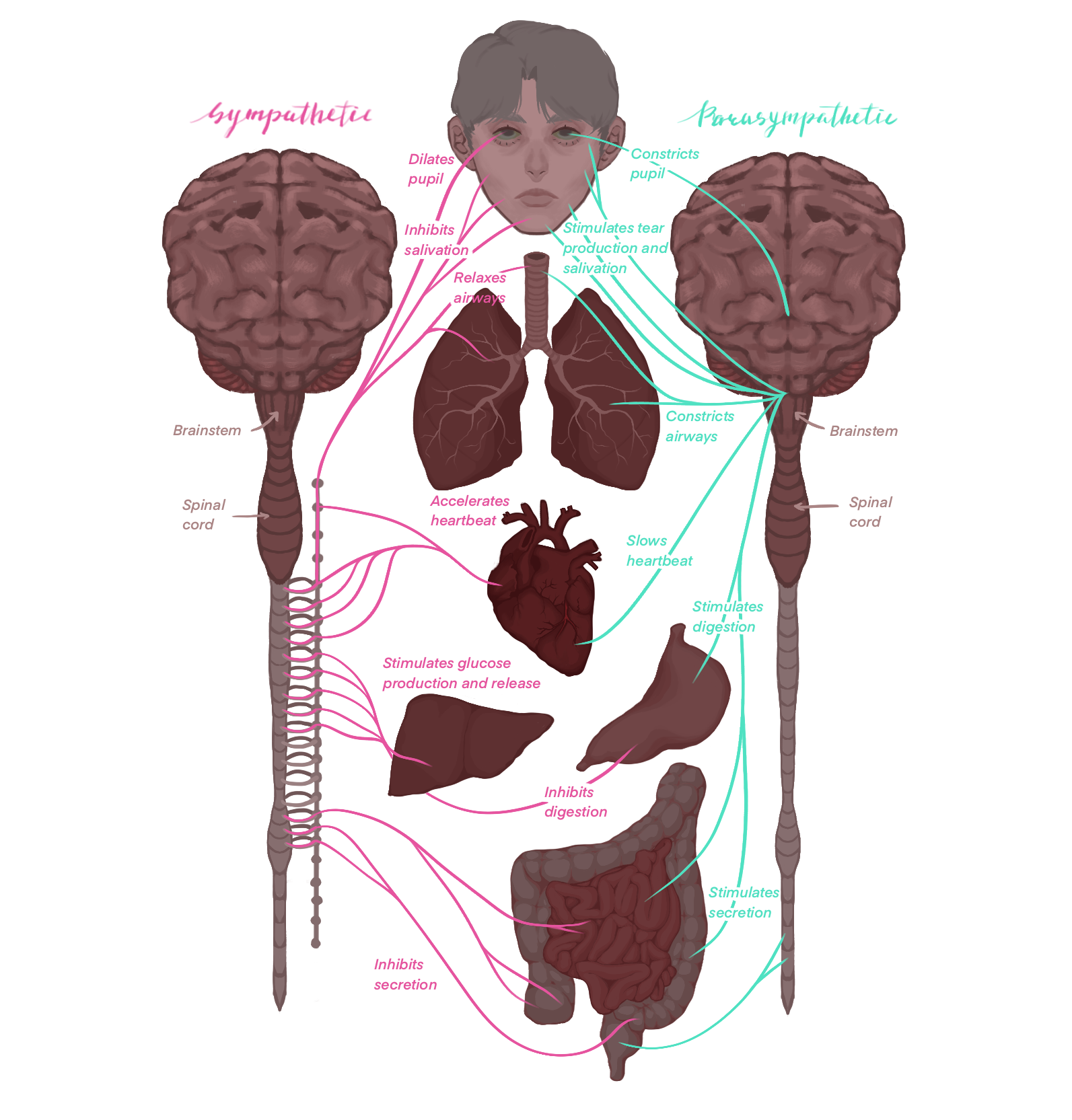
One particularly clear example of this phenomenon is how the two systems affect heart rate. When the SNS stimulates the heart, it increases heart rate and the force of contraction, whereas the PNS reduces heart rate and force of contraction [6]. Heart rate is thought to be controlled by the sinoatrial (SA) node, also known as the pacemaker, through what's called a funny current. The funny current is the flow of positive ions into the cell. Over time, the positive ions in the cell accumulate until they reach a certain threshold. Once the cell reaches threshold it triggers an action potential that spreads to the rest of the heart, causing it to beat. Once the action potential ends, the cell is back to its initial state and the positive ions start to accumulate again. The time it takes to reach threshold is what controls heart rate and can be affected by several different mechanisms. The PNS modulates heart rate by releasing acetylcholine, which binds to receptors that open potassium channels. Opening these channels generates an outward potassium current that works against the normal inward current that regulates the heart rate, increasing the time it takes for the cell to reach threshold and slowing down the heart rate [6]. Less is known about the mechanism of SNS on heart rate, although studies suggest that epinephrine increases heart rate by binding to a receptor which causes either the speed at which the positive ions accumulate in the cell to increase, or the threshold they must reach to decrease, causing the heart to beat more frequently [6].
The immediate physiological response to stress is created by an increase in the release of epinephrine from the SNS [7]. This response can occur in less than a second, something that can easily be observed by watching a horror movie, where a jump scare can cause your heart rate and breathing to increase almost instantly. After the initial phase of the stressor, there is the activation of another system called the hypothalamic-pituitary-adrenal axis [8]. The system is a chain of activation, traveling from the hypothalamus in the forebrain to the pituitary gland right below it, and finally to the adrenal glands located above the kidneys, where a hormone called cortisol is produced and released [8]. This release of cortisol continues for several hours, even after the stressor is no longer present. Numerous cortisol receptors are located all over the body, allowing a wide range of effects, but they generally affect metabolism by increasing the production of glucose and the breakdown of proteins to provide more resources for critical areas [9]. Cortisol also inhibits hormones for growth and reproduction, functions that might take up resources needed for the stress response [10][11]. The combination of the initial SNS activation and subsequent release of cortisol work together to produce the stress response.
With this new understanding of how the stress response works, we can view the symptoms of stress as the efforts of our body to help us survive a physically dangerous situation. Generally, they involve moving resources like blood to high-priority areas or decreasing the activity of low-priority areas [2]. The SNS dilates vessels that supply the skeletal muscles and constricts vessels to nonessential areas like the skin and stomach. This helps to move more blood and the resources it carries to the large muscles in your arms and legs, providing the maximum force possible to help you survive. As a result, less blood flows to other areas, causing other symptoms. Becoming pale is due to the flow of blood away from your skin, a non-critical area. Indigestion is caused by the reduced activity of the smooth muscles in the digestive tract– because digesting your lunch isn’t as important as making sure it’s not your last meal. Increased cortisol also decreases appetite. Apart from prioritizing resources, symptoms can also come from the stress response trying to increase the resources available, namely by increasing heart rate, the strength of the heart contraction, and breathing [2].
Long-term damage due to chronic stress
Stress can be uncomfortable in the moment, but when the stress response is extended over long periods of time, as with chronic stress, it starts to cause serious damage. One of the major systems vulnerable to damage from chronic stress is the cardiovascular system. As previously discussed, the stress response causes a number of effects, including increasing blood pressure and increasing the strength of the heartbeat [2]. This can damage the heart and arteries, leading to an increased risk of cardiovascular failure or disease. A massive study with over 20,000 participants from 52 countries found that participants who reported higher stress during the previous year were at a greater risk for a heart attack [12]. This increased risk remained even after adjusting for the risk factors of cardiovascular disease like activity, diet, and other conditions. Another analysis that combined the results of four individual studies found that perceived stress was associated with an increased chance of stroke, including fatal strokes [13].
Stress can also harm the immune system. Generally, studies suggest that acute stress causes a temporary increase in the activity of the innate immune system, but in chronic stress, the extended stress response appears to suppress the immune system [3]. This weakened immune system can cause those suffering from chronic stress to be more vulnerable to illness, which can be anecdotally observed in populations like college students.
Another concerning effect of chronic stress is its potential to damage the brain. A study at the Stockholm Brain Institute found that subjects who had long-term occupational stress had atrophy in their basal ganglia and certain areas of the prefrontal cortex, both of which are involved in higher-level functions like cognitive control and voluntary behavior [14]. This atrophy is suggested to be caused by the high levels of cortisol involved in chronic stress. Researchers found that when cortisol levels are high, a protein they labeled REDD1 was produced and inhibited protein synthesis in neurons, which could cause atrophy. The deletion of the REDD1 gene reduced the stress response in mice, further supporting the production of this protein as the mechanism by which high levels of cortisol during chronic stress can cause atrophy in certain areas of the brain [15]. Similar patterns of atrophy in the basal ganglia and prefrontal cortex were seen in clinically depressed patients who were examined postmortem, suggesting the atrophy could be the mechanism underlying the depressive symptoms seen in chronic stress [14].
Ways to use your understanding of the SNS and PNS to reduce stress
As we have seen, stress can be not only uncomfortable but also detrimental to health, so it's critical to understand how we can limit its effects. The most obvious solution would be to remove the external stressor. However, this may not always be possible if the stressor comes from a larger socioeconomic or institutional issue. Fortunately, methods to relieve stress do exist and many are already popular, but they can sometimes feel ineffective or time-consuming [source]. A study at Emory University showed that eight weeks of guided slow breathing, one of the most commonly recommended treatments for stress, reduced the sympathetic activity of muscles, which is used as a marker for general SNS activation. Lowered SNS activity can indicate a reduced stress response and a reduction in the negative effects of stress [16].
Another common piece of advice is to take a walk or spend some time in nature. This may sound simple, but a study by the EMGO Institute for Health and Care Research found that subjects who viewed photos of green spaces had a greater increase in their respiratory sinus arrhythmia, a cardiac marker of parasympathetic activity, after an induced stress response. This suggests that exposure to nature increases PNS activity, reducing the stress response [17]. Another study found that PTSD patients who hiked in natural environments showed a greater improvement in their symptoms than those who hiked in urban environments [18].
Studies also suggest that social support can affect a person's response to stress. A study at UCLA looked at the effects of prosocial behaviors like helping others on the physiological response to stress [19]. They compared subjects who gave a gift card to a person of their choice, the prosocial behavior, to subjects who received a gift card or did a control activity. The researchers induced stress in all subjects with the Trier Social Stress Test, a standardized method to induce social stress that involves public speaking and a difficult math task. They found that participants who gave a gift card had a greater reduction in heart rate and blood pressure during their recovery from the induced stress than participants who received a gift card or did a control activity [19]. Researchers at the University of Pittsburgh performed a similar study, but instead had participants complete the prosocial behavior of writing a supportive note before the stressful task. They found that participants who engaged in prosocial behavior had lowered blood pressure and alpha-amylase, a marker of SNS activity, both during the task and during recovery [20]. Together, these findings suggest that prosocial behavior can both reduce the initial response to stress and increase recovery from the stressful event.
Listening to music has also been suggested as a way to reduce stress after a stressful event. One study compared university students who had listened to music after a stressful task to those who did nothing [21]. To induce stress, the researchers had participants complete difficult math and visual tests under time pressure and the sound of a ticking clock. After the stress induction, they asked half of the students to listen to music that the participants had preselected and used parts of the heart rate as markers for SNS and PNS activity. They found that the students who listened to music after the task had a greater decrease in the marker of SNS activity and a greater increase in the marker of PNS activity compared to the control group. This suggests that music helps rebalance the two systems after a stressful event [21].
Recent studies have also demonstrated the effect of meditation on the stress response. Researchers found that thirty hours of meditation training reduced the cortisol levels of participants. This reduction was seen both in response to a stressful task and in their base cortisol levels, measured right after they woke up. This shows that meditation can benefit those suffering from chronic stress [22]. Although certainly not extensive, these methods provide a snapshot of strategies commonly used to reduce stress, and show that we can gain control over our body’s stress response.
Overall, stress can feel overwhelming, but it is just our body’s response to a perceived threat that isn’t adapted to modern stress. While chronic stress can be damaging, there are many methods that have been shown to reduce the effects of stress. Although it’s great to understand the actions an individual can take to reduce the damaging effects of the stress they experience, it is important to also consider what can be done at a larger level to reduce the stress placed on the population. While one of the studies previously discussed suggested that exposure to green spaces can reduce stress, it also suggests that the loss of green spaces due to economic growth and urban expansion could be causing an increase in the damaging effects of stress [17]. This phenomenon, combined with the disparities in the number of green spaces between high and low-income areas could be contributing to socioeconomic health inequality. Green spaces are only one example– there are many areas where we need to address the stress people experience. Hopefully, through further understanding how the stress response works, and the ways we can reduce its effects, we can make progress towards reducing the burden of stress.
References:
- American Psychological Association. (2020, October). Stress in AmericaTM 2020: A National Mental Health Crisis. American Psychological Association. https://www.apa.org/news/press/releases/stress/2020/report-october
- Waxenbaum, J. A., Reddy, V., & Varacallo, M. (2023). Anatomy, Autonomic Nervous System. In StatPearls. StatPearls Publishing. https://pubmed.ncbi.nlm.nih.gov/30969667/
- McEwen B. S. (2007). Physiology and neurobiology of stress and adaptation: central role of the brain. Physiological reviews, 87(3), 873–904. https://doi.org/10.1152/physrev.00041.2006
- Wehrwein, E. A., Orer, H. S., & Barman, S. M. (2016). Overview of the Anatomy, Physiology, and Pharmacology of the Autonomic Nervous System. Comprehensive Physiology, 6(3), 1239–1278. https://doi.org/10.1002/cphy.c150037
- Gordan, R., Gwathmey, J. K., & Xie, L. H. (2015). Autonomic and endocrine control of cardiovascular function. World journal of cardiology, 7(4), 204–214. https://doi.org/10.4330/wjc.v7.i4.204
- Sohn, R., & Jenei-Lanzl, Z. (2023). Role of the sympathetic nervous system in mild chronic inflammatory diseases - focus on osteoarthritis. Neuroimmunomodulation, 30(1), 143–166. https://doi.org/10.1159/000531798
- DeMorrow, S. (2018). Role of the hypothalamic–pituitary–adrenal axis in health and disease. International Journal of Molecular Sciences, 19(4), 986. https://doi.org/10.3390/ijms19040986
- Chrousos G. P. (2000). The role of stress and the hypothalamic-pituitary-adrenal axis in the pathogenesis of the metabolic syndrome: neuro-endocrine and target tissue-related causes. International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity, 24 Suppl 2, S50–S55. https://doi.org/10.1038/sj.ijo.0801278
- Burguera, B., Muruais, C., Peñalva, A., Dieguez, C., & Casanueva, F. F. (1990). Dual and selective actions of glucocorticoids upon basal and stimulated growth hormone release in man. Neuroendocrinology, 51(1), 51–58. https://doi.org/10.1159/000125315
- Kyrou, I., Chrousos, G. P., & Tsigos, C. (2006). Stress, visceral obesity, and metabolic complications. Annals of the New York Academy of Sciences, 1083, 77–110. https://doi.org/10.1196/annals.1367.008
- Rosengren, A., Hawken, S., Ounpuu, S., Sliwa, K., Zubaid, M., Almahmeed, W. A., Blackett, K. N., Sitthi-amorn, C., Sato, H., Yusuf, S., & INTERHEART investigators (2004). Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet (London, England), 364(9438), 953–962. https://doi.org/10.1016/S0140-6736(04)17019-0
- Booth, J., Connelly, L., Lawrence, M., Chalmers, C., Joice, S., Becker, C., & Dougall, N. (2015). Evidence of perceived psychosocial stress as a risk factor for stroke in adults: a meta-analysis. BMC neurology, 15, 233. https://doi.org/10.1186/s12883-015-0456-4
- Blix, E., Perski, A., Berglund, H., & Savic, I. (2013). Long-term occupational stress is associated with regional reductions in brain tissue volumes. PloS one, 8(6), e64065. https://doi.org/10.1371/journal.pone.0064065
- Ota, K. T., Liu, R. J., Voleti, B., Maldonado-Aviles, J. G., Duric, V., Iwata, M., Dutheil, S., Duman, C., Boikess, S., Lewis, D. A., Stockmeier, C. A., DiLeone, R. J., Rex, C., Aghajanian, G. K., & Duman, R. S. (2014). REDD1 is essential for stress-induced synaptic loss and depressive behavior. Nature medicine, 20(5), 531–535. https://doi.org/10.1038/nm.3513
- Fonkoue, I. T., Hu, Y., Jones, T., Vemulapalli, M., Sprick, J. D., Rothbaum, B., & Park, J. (2020). Eight weeks of device-guided slow breathing decreases sympathetic nervous reactivity to stress in posttraumatic stress disorder. American journal of physiology. Regulatory, integrative and comparative physiology, 319(4), R466–R475. https://doi.org/10.1152/ajpregu.00079.2020
- van den Berg, M. M., Maas, J., Muller, R., Braun, A., Kaandorp, W., van Lien, R., van Poppel, M. N., van Mechelen, W., & van den Berg, A. E. (2015). Autonomic Nervous System Responses to Viewing Green and Built Settings: Differentiating Between Sympathetic and Parasympathetic Activity. International journal of environmental research and public health, 12(12), 15860–15874. https://doi.org/10.3390/ijerph121215026
- Littman, A. J., Bratman, G. N., Lehavot, K., Engel, C. C., Fortney, J. C., Peterson, A., Jones, A., Klassen, C., Brandon, J., & Frumkin, H. (2021). Nature versus urban hiking for Veterans with post-traumatic stress disorder: a pilot randomised trial conducted in the Pacific Northwest USA. BMJ open, 11(9), e051885. https://doi.org/10.1136/bmjopen-2021-051885
- Lazar, L., & Eisenberger, N. I. (2021). The benefits of giving: Effects of prosocial behavior on recovery from stress. Psychophysiology, 59(2). https://doi.org/10.1111/psyp.13954
- Inagaki, T. K., & Eisenberger, N. I. (2016). Giving support to others reduces sympathetic nervous system-related responses to stress. Psychophysiology, 53(4), 427–435. https://doi.org/10.1111/psyp.12578
- Lee, K. S., Jeong, H. C., Yim, J. E., & Jeon, M. Y. (2016). Effects of Music Therapy on the Cardiovascular and Autonomic Nervous System in Stress-Induced University Students: A Randomized Controlled Trial. Journal of alternative and complementary medicine (New York, N.Y.), 22(1), 59–65. https://doi.org/10.1089/acm.2015.0079
- Bottaccioli, A. G., Bottaccioli, F., Carosella, A., Cofini, V., Muzi, P., & Bologna, M. (2020). Psychoneuroendocrinoimmunology-based meditation (PNEIMED) training reduces salivary cortisol under basal and stressful conditions in healthy university students: Results of a randomized controlled study. Explore (New York, N.Y.), 16(3), 189–198. https://doi.org/10.1016/j.explore.2019.10.006
