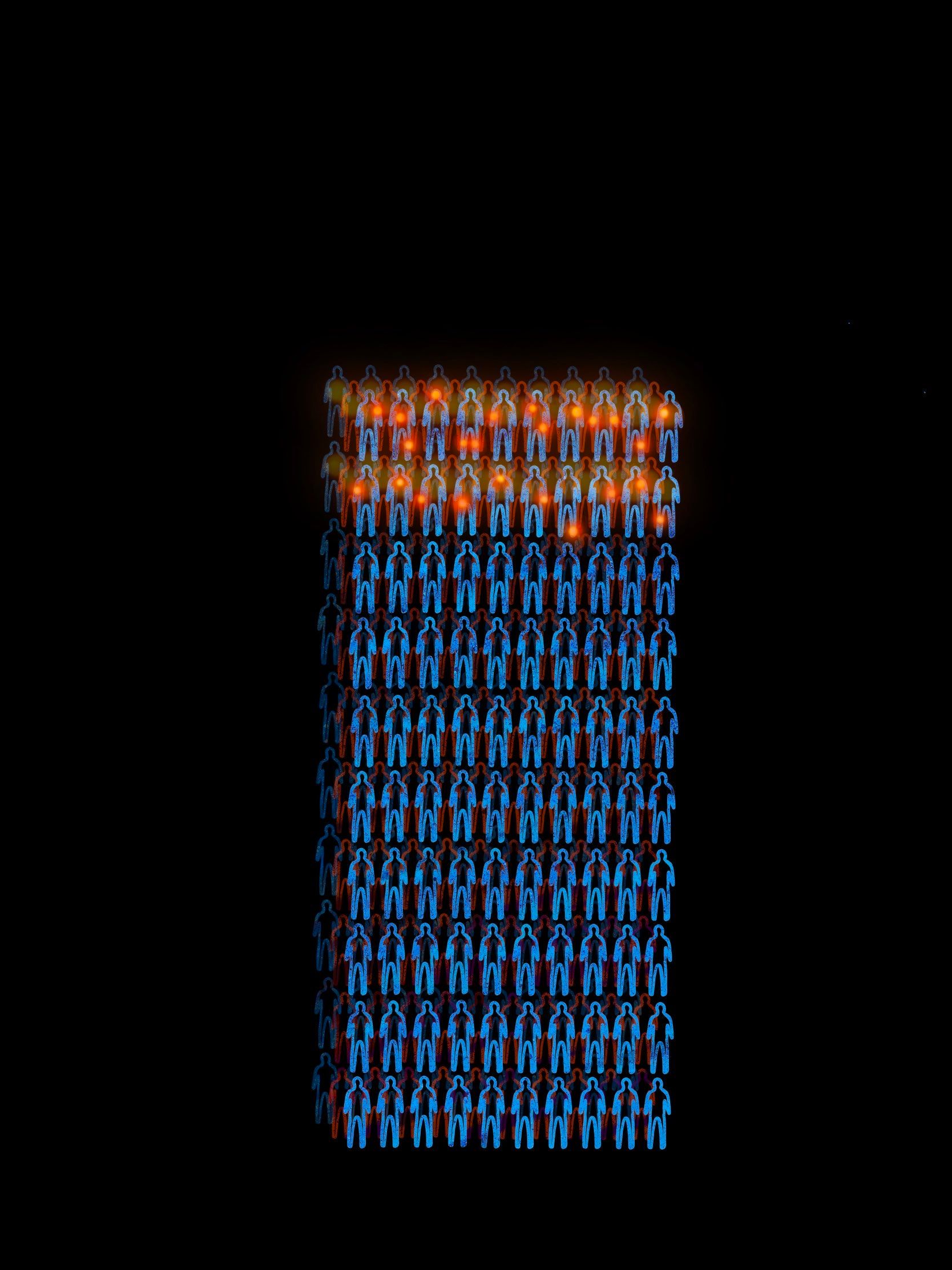
Everyone knows what pain is…right? While most people have a comfortable understanding of what pain means to them, pain as a clinical symptom is nebulous: difficult to describe and even more difficult to treat [1]. Pain can be anything from a mild annoyance to a daily mountain to climb. While acute pain is temporary, chronic pain is a long-term burden, lasting more than three months and often for life [1]. Chronic pain is a widespread problem. In 2019, the National Health Interview Survey revealed that one in five adults have chronic pain, a third of which live with high-impact chronic pain that limits work and other daily activities [2]. With chronic pain affecting an estimated 76.2 million Americans – more than diabetes, heart disease, and cancer combined – there is a growing need for effective pain treatment [3].
The Opioid Epidemic
In an effort to prioritize addressing pain in healthcare, organizations such as the Veterans Health Administration (VHA) and the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) added pain as the fifth vital sign in 1999, alongside body temperature, pulse, blood pressure, and respiration rate [3]. Recognizing pain as one of the five vital signs helps clinicians standardize their healthcare evaluation and treatment. However, this step forward also dangerously simplifies routine pain assessments to a one-dimensional scale. Unlike the remaining vital signs, pain is subjective: one patient’s level six pain may be a four on another’s scale. While well-intended, the effort failed and in 2016, the American Medical Association removed pain as a vital sign [4].
One consequence of the push for system-wide reform to pain management has been a dramatic increase in prescription opioids and opioid-related deaths [3]. The uptick in prescription of opioids for pain management has changed the landscape of the modern opioid epidemic. Today, opioids represent a majority of drug overdose related deaths [5]. When treating pain pharmacologically, morphine is one of the first-line opioids used [6][7][8]. Other standard treatments involve derivatives of morphine that bind to the same opioid receptor. Using a strong opiate like morphine is tricky. It is attractive as a pain treatment due to its potent pain relief properties, but it comes with a catch. Strong drugs often elicit another response known as tolerance, which occurs when the body becomes accustomed to a drug and requires a progressively higher dose to achieve the same baseline effect. If a patient were to take the same dose of morphine daily, the relief provided would eventually shrink to nothing. Humans show measurable morphine tolerance in the first week at all doses [6][7][8]. This leads to a twofold effect: patients depend on increasing opioid usage for pain relief, and they risk addiction.
Drug addiction has two main components: a chemical and a psychological one. In chemical addiction, the body depends on the drug for a certain level of function. In psychological addiction, the person believes they need the drug for a certain level of function. Together, this may result in erratic behaviors towards continued drug usage [9]. To use a parallel example, withdrawal from caffeine dependence due to chemical effects can last up to a couple of weeks [10]. Psychological dependence is more complex in caffeine use disorder, and there is no set timeline for cessation of effects [11]. Moreover, drug tolerance reinforces dependence on morphine and is why the drug has a high risk of substance abuse. According to the 2019 National Survey on Drug Use and Health, 96 percent of 10.1 million opioid misuse cases that year were of prescription opioids. Of these, an estimated 1.6 million people were first-time misusers [12]. There are existing treatments for morphine tolerance that provide some pain relief but are less addictive, such as weaker opioids like methadone [13][14]. These treatments are currently insufficient as a replacement for morphine for many reasons. Using weaker opioids to combat opioid addiction is partially effective in reducing withdrawal and relapse. However, they are still opioids that bind to the same receptor and thus have similar side effects in long-term usage that makes morphine dangerous and addicting [13][14]. Additionally, other opioids come with different chemical dynamics in the body that are poorly understood and complex [15].
Defeating the opioid epidemic means treating the problem from both sides of the timeline: providing effective pain treatment and addressing the addiction that can stem from it. It is an endless cycle where current pain treatments lead to addiction, creating a need for new effective treatments. This burden is felt at all levels: for the patient facing both addiction and persisting pain, the clinicians seeking to treat pain without causing addiction, and the ripple effects felt in other industries. An ideal solution would combat tolerance while enabling the same level of relief. Without improving the current toolbox of pain treatments, the epidemic will continue to persist.
Looking into the Microscope
Let’s zoom into the tolerance process on the cellular level. To grasp a better understanding of tolerance, it is important to understand how our bodies interact with drugs like morphine. What does acute morphine tolerance look like in a single cell? As our body adjusts to new drugs in its system, especially strong drugs like morphine, cells adapt by decreasing signaling. Morphine binds to its receptor at the cell membrane, then downstream signaling cascades fall like dominos, leading to some of morphine’s more well-known effects: euphoria, pain relief, and depression of breathing. Over time, the cell begins to inactivate their receptors, and less signaling occurs. When this happens, the cell no longer reacts to morphine binding onto its receptors [16]. But how does this happen inside the cell? Honestly, scientists don’t know for sure. The most recent hypothesis came with the discovery of the phospho-cJun N-terminal Kinase (JNK) tolerance mechanism [17]. When morphine meets a neuron, it binds to a protein called the mu-opioid receptor (MOR), which then changes shape. This starts an intracellular signaling cascade that ends with the production of reactive oxygen species (ROS) like hydrogen peroxide. ROS then inactivates the opioid pathway by turning off MOR and linked proteins, effectively preventing all responses to morphine. This is currently believed to be the cause of MOR inactivation and acute morphine tolerance [17][18].
Enter a New Player: Cannabidiol
In Cannabis, there are two primary phytocannabinoids: cannabidiol (CBD) and tetrahydrocannabinol (THC) [19]. Generally, CBD is associated with hemp and THC is associated with marijuana, two different strains of Cannabis. More specifically, the plant must contain less than 0.3% THC to classify and be sold as hemp. Cannabis has maintained popularity for thousands of years for its pain relief properties, among other effects. This relief has in large part been credited to THC; however, CBD is also beginning to attract attention from both the general public and researchers. This is partly due to the 2018 Farm Bill removing hemp, a sub-type of Cannabis with low levels of THC and higher levels of CBD, from the Controlled Substances Act [19]. CBD is especially interesting as a future avenue of pain and addiction treatment, as it is the non-psychoactive strain contemporary to THC [20]. Clinical data from the Icahn School of Medicine at Mount Sinai suggests that CBD alleviates some opioid withdrawal symptoms such as anxiety, depression, inflammation, and relaxing effects [21]. On a psychological level, CBD also reduces cue-induced opioid seeking behaviors. Additionally, CBD was well received in co-treatment with potent opioids and showed no significant negative effects [21].
Across America, rising access to medical Cannabis is associated with a decrease in filled opioid-related prescriptions [22][23]. This is not terribly surprising, as the pre-existing internal opioid and cannabinoid systems in humans are believed to both be involved in pain relief and utilizing the neural pathways and brain regions associated with addiction [24][25][26][27]. It is important to note, however, that scientists do not yet understand how CBD works in humans. With this in mind, researchers have become curious about potential signaling overlap between CBD and morphine [17]. If CBD can block the morphine tolerance pathway, it could have the potential to serve as a co-treatment with morphine and preempt opioid addiction. Researchers at the University of Washington hypothesize that CBD enters the morphine tolerance pathway by inhibiting JNK signaling. When tested in both mouse models and cell models, researchers observed less morphine JNK signaling in groups given CBD and morphine together than when groups were given only morphine. This indicates that CBD is delaying or even blocking JNK signaling and the associated morphine tolerance. Mouse models also revealed longer lasting pain relief at sustained doses of morphine when given with CBD [17].
The potential synergistic effects between morphine and CBD are promising for several reasons. One benefit of inhibiting morphine tolerance at JNK, which is lower in the signaling pathway, is that it is less likely to have undesirable side effects. We might see future applications of this research in which CBD is used as a co-treatment with morphine to maintain the potent pain relief effects while decreasing acute morphine tolerance and risk of addiction.
It is important to note that properties of CBD are not well characterized. Like with other proposed treatments, CBD is unlikely to be a miracle drug that solves all of our problems. Regardless, each discovery is an important step towards understanding how to better treat patients. The exciting potential synergy between morphine and CBD could simply be an additive effect instead of an intersection of signaling pathways [28]. Next steps for research involving the morphine JNK signaling pathway will likely explore effects of CBD on its own and in a longer study [17].
TLDR
The long and short of it for those of you who skipped to the end is simple: CBD is this season’s rising star in pain medicine. The research presented in this article on CBD shows some promise to steer the opioid epidemic in our favor. The role of JNK signaling in morphine tolerance is groundbreaking, as science has long struggled to find a cellular explanation behind morphine tolerance. Our current treatments for chronic pain have limited efficacy and carry risk of addiction and abuse. We continue to need effective treatments for the millions of patients living with chronic pain. CBD could potentially help make an existing treatment, morphine, do its job better. While CBD as a co-treatment with morphine or even an addiction treatment is new and unquantified, we have high hopes for its future role in pain medicine.
References
- Chronic Pain. (2021, August 8). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/chronic-pain
- NCHS Data Briefs - Number 390 - November 2020. (2020, November). National Center for Health Statistics. https://www.cdc.gov/nchs/products/databriefs/db390.htm#:%7E:text=Interview%20Survey%2C%202019.-,Summary,65%20and%20over%20(30.8%25)
- Morone, N. E., & Weiner, D. K. (2013). Pain as the fifth vital sign: exposing the vital need for pain education. Clinical therapeutics, 35(11), 1728–1732. https://doi.org/10.1016/j.clinthera.2013.10.001
- Scher, C., Meador, L., Van Cleave, J. H., & Reid, M. C. (2018). Moving Beyond Pain as the Fifth Vital Sign and Patient Satisfaction Scores to Improve Pain Care in the 21st Century. Pain management nursing : official journal of the American Society of Pain Management Nurses, 19(2), 125–129. https://doi.org/10.1016/j.pmn.2017.10.010
- Vital Statistics Rapid Release - Provisional Drug Overdose Data. (2022, May). National Vital Statistics System. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
- Adesoye, A., Duncan, N. (2017). Acute Pain Management in Patients With Opioid Tolerance. US Pharmacist. 42(3):28-32.
- Gudin, J. (2012). Risk Evaluation and Mitigation Strategies (REMS) for Extended-Release and Long-Acting Opioid Analgesics: Considerations for Palliative Care Practice. Journal of Pain & Palliative Care Pharmacotherapy, 26(2), 136–143. https://doi.org/10.3109/15360288.2012.679724
- Xu, J., Faskowitz, A. J., Rossi, G. C., Xu, M., Lu, Z., Pan, Y. X., & Pasternak, G. W. (2014). Stabilization of morphine tolerance with long-term dosing: Association with selective upregulation of mu-opioid receptor splice variant mRNAs. Proceedings of the National Academy of Sciences, 112(1), 279–284. https://doi.org/10.1073/pnas.1419183112
- Juurlink, D. N., & Dhalla, I. A. (2012). Dependence and addiction during chronic opioid therapy. Journal of medical toxicology : official journal of the American College of Medical Toxicology, 8(4), 393–399. https://doi.org/10.1007/s13181-012-0269-4
- Sajadi-Ernazarova KR, Anderson J, Dhakal A, et al. Caffeine Withdrawal. [Updated 2022 Apr 30]. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK430790/
- Meredith, S. E., Juliano, L. M., Hughes, J. R., & Griffiths, R. R. (2013). Caffeine Use Disorder: A Comprehensive Review and Research Agenda. Journal of caffeine research, 3(3), 114–130. https://doi.org/10.1089/jcr.2013.0016
- Opioid Crisis Statistics. US Department of Health and Human Services. (2021) https://www.hhs.gov/opioids/about-the-epidemic/opioid-crisis-statistics
- Clinical Guidelines for Withdrawal Management and Treatment of Drug Dependence in Closed Settings. Geneva: World Health Organization; 2009. 6, Methadone maintenance treatment. https://www.ncbi.nlm.nih.gov/books/NBK310658/
- Lintzeris, N. & National Expert Advisory Committee on Illicit Drugs (Australia). Department of Health and Aging. & National Drug Strategy (Australia). (2006). National clinical guidelines and procedures for the use of buprenorphine in the treatment of opioid dependence. Canberra: Dept. of Health and Aging, http://www.nationaldrugstrategy.gov.au/internet/drugstrategy/publishing.nsf/Content/15B5C4ED2E7A5F75CA25717E000A39CC/$File/buprenorphine_guide.pdf
- Guevara, N., Lorier, M., Vázquez, M., Fagiolino, P., Feria-Romero, I., & Orozco-Suarez, S. (2018). Revisiting Pharmacokinetics and Pharmacogenetics of Methadone in Healthy Volunteers. In V. Gaitonde, P. Karmakar, & A. Trivedi (Eds.), Drug Discovery and Development - New Advances. IntechOpen. https://doi.org/10.5772/intechopen.82426
- Stein, C. (2016) Opioid Receptors. Annual Review of Medicine 67:1, 433-451
- Schattauer, S. S., Land, B. B., Reichard, K. L., Abraham, A. D., Burgeno, L. M., Kuhar, J. R., Phillips, P. E. M., Ong, S. E., & Chavkin, C. (2017). Peroxiredoxin 6 mediates Gαi protein-coupled receptor inactivation by cJun kinase. Nature Communications, 8(1). https://doi.org/10.1038/s41467-017-00791-2
- Langsdorf, E.F. (2011). Reactive Oxygen Species Modulation of the Mu-Opioid Receptor. Seton Hall University Dissertations and Theses (ETDs). 1765. https://scholarship.shu.edu/dissertations/1765
- Hemp Production and the 2018 Farm Bill. (2019, July 25). U.S. Food and Drug Administration. https://www.fda.gov/news-events/congressional-testimony/hemp-production-and-2018-farm-bill-07252019
- McLemon, E., & Chesworth, R. (2021). Cannabinoid treatment of opiate addiction. Neuroanatomy and Behaviour, 3, e14. https://doi.org/10.35430/nab.2021.e14
- Kudrich, C., Hurd, Y. L., Salsitz, E., & Wang, A. L. (2021). Adjunctive Management of Opioid Withdrawal with the Nonopioid Medication Cannabidiol. Cannabis and Cannabinoid Research. https://doi.org/10.1089/can.2021.0089
- Aviram, J., Lewitus, G. M., Vysotski, Y., Amna, M. A., Ouryvaev, A., Procaccia, S., Cohen, I., Leibovici, A., Akria, L., Goncharov, D., Mativ, N., Kauffman, A., Shai, A., Bar-Sela, G., & Meiri, D. (2022). The Effectiveness and Safety of Medical Cannabis for Treating Cancer Related Symptoms in Oncology Patients. Frontiers in Pain Research, 3. https://doi.org/10.3389/fpain.2022.861037
- Wendelboe, A. M., Mathew, R., Chongsuwat, T., Rainwater, E., Wendelboe, M. A., Wickersham, E., & Chou, A. F. (2019). Is There Less Opioid Abuse in States Where Marijuana Has Been Decriminalized, Either for Medicinal or Recreational Use? A Clin-IQ. Journal of Patient-Centered Research and Reviews, 6(4), 267–273. https://doi.org/10.17294/2330-0698.1704
- Scavone, J., Sterling, R., & van Bockstaele, E. (2013). Cannabinoid and opioid interactions: Implications for opiate dependence and withdrawal. Neuroscience, 248, 637–654. https://doi.org/10.1016/j.neuroscience.2013.04.034
- Fattore, L., Deiana, S., Spano, S., Cossu, G., Fadda, P., Scherma, M., & Fratta, W. (2005). Endocannabinoid system and opioid addiction: Behavioural aspects. Pharmacology Biochemistry and Behavior, 81(2), 343–359. https://doi.org/10.1016/j.pbb.2005.01.031
- Robledo, P., Berrendero, F., Ozaita, A., & Maldonado, R. (2008). Advances in the field of cannabinoid-opioid cross-talk. Addiction Biology, 13(2), 213–224. https://doi.org/10.1111/j.1369-1600.2008.00107.x
- Mansour, A., Fox, C. A., Akil, H., & Watson, S. J. (1995). Opioid-receptor mRNA expression in the rat CNS: anatomical and functional implications. Trends in Neurosciences, 18(1), 22–29. https://doi.org/10.1016/0166-2236(95)93946-u
- Chen, X., Cowan, A., Inan, S., Geller, E. B., Meissler, J. J., Rawls, S. M., Tallarida, R. J., Tallarida, C. S., Watson, M. N., Adler, M. W., & Eisenstein, T. K. (2019). Opioid-sparing effects of cannabinoids on morphine analgesia: participation of CB1 and CB2 receptors. British journal of pharmacology, 176(17), 3378–3389. https://doi.org/10.1111/bph.14769
