Introduction
We’ve come a long way since the cranial surgeries of the neolithic period, where small holes were drilled in the skull to release evil, disease-causing spirits. Ancient peoples had attributed these unexplainable symptoms of epilepsy, mental illness, and schizophrenia to the supernatural [1], but as ancient anatomists learned more about the brain, they began to attribute diseases not to spirits but to physiological imbalances in the body itself. Some cultures such as Hippocrates’ Greece hesitated to perform human surgeries or dissections unless absolutely necessary - opting for a more herbal and holistic treatment approach to these imbalances [2]. This hesitancy or apprehension may stem from the duality of neurosurgery that exists even in the modern era. Modern day neurosurgery is beautiful yet terrifying. Sterile yet warm and compassionate. We have access to the most precise and accurate diagnostic and imaging technology in the history of mankind. We have real-time intraoperative navigation of the brain to better locate more tumors, lesions, and other areas of interest than ever before [3]. Surgery is beautiful in our undying will and desire to treat these life-altering nervous system malfunctions. It is beautiful in the ways that our scalpel and microscopes can uncover the blood, bones, cells, and vessels that work together to create our realities. It is beautiful in giving us another toolbox in our endeavor towards a longer, happier future with our families. Each step along the way, each attention to detail is supported by decades if not centuries of research built upon the foundations of prior generations. Yet, even with all these advancements, there are risks with any surgical procedure. The surgical outcome may improve quality of life but may not resolve all the symptoms. Neurosurgery can fail. We are talking about involving one of our most prized possessions: the thing that makes us, us. Our identity. Our brain. It is the warehouse and machinery that stores the memories of our loved ones and operates our bodily functions. It can be terrifying to think about the unknowns of neurosurgery. It can be daunting to start learning about neuroscience in general. It can be scary to think about the outcomes of a procedure. Globally, an estimated 13.8 million annual neurological cases require surgical intervention [4]. With only 3,800 board certified neurosurgeons in the USA, access to open discussion and dialogue about neurological surgery can be limited [5]. This article is meant to bridge the knowledge gap between the experts in the field and anyone who wants to learn about neurosurgery through discussion of two commonly performed surgeries in the Anterior Cervical Discectomy & Fusion (ACDF) and Extracranial-Intracranial Bypass (EC-IC Bypass). The goal is to make neurosurgery anatomy accessible and to help answer brimming questions and budding students’ curiosities.
Patient Population
Responsibility bears heavy on the surgeon as their scalpel grazes betadine-prepped skin in the operating room, because surgery is often one of the last lines of treatment for a patient. Some conditions heal naturally on their own, but if intervention is required, medication for pain management, physical therapy to rebuild, or technology to support may be used to improve quality of life. Often, surgical intervention is suggested only in cases where these approaches do not meet patient expectations. This recommendation is given with a patient’s unique circumstances, life-style, and cost-risk analysis in mind. The patient population that would require an ACDF are usually people who present chronic compression of the spinal cord called myelopathy or nerve roots called radiculopathy [6]. These are long-term conditions that progressively deteriorate a person’s quality of life. Some symptoms may include loss of dexterity, strength, and pain in the upper extremities [7]. The patient population that would require an EC-IC bypass usually presents with cranial stenosis or narrowing of a blood vessel, blockage in a blood vessel, or had a history of ischemic strokes [8]. An ischemic stroke occurs when an artery cannot adequately pass blood to parts of the brain. That said, there are a plethora of reasons that would warrant surgical intervention, and each person is unique in their needs.
Anterior Cervical Discectomy & Fusion
Each step in a surgery is done for a specific purpose. It can be helpful to think about the purpose from a bottom-up approach and the steps of the procedure in chronological order. In the long name of: Anterior Cervical Discectomy & Fusion (ACDF), anterior refers to approaching the cervical (neck) area from the front of the body. A discectomy is the surgical removal of the vertebral discs of the spinal cord. A fusion refers to the management of the two adjacent vertebrae to hold it in place. Thus, the main purpose of the ACDF is to remove parts or the entirety of a herniated, degraded, bulging, or thinning vertebral disc through the front of the neck. Some common contributing factors to disc damage are lifestyle, bad posture, trauma, or genetic predisposition [9]. These discs act as the connective gel tissue to prevent the bony vertebral column from grinding itself down. If the discs are damaged, the spinal nerves that project from the vertebral openings can get pinched leading to pain, motor deficits, or weakness in the upper extremities or neck. These pinched nerves may mimic symptoms of carpal tunnel or pain from overuse, which makes ACDF hard to characterize [6].
There are a lot of layers before accessing the vertebrae [6]. Once the patient is given anesthesia, an endotracheal tube may be placed to ensure an open airway. Then, a horizontal or more rarely, a vertical incision is made in the front of the neck. Retractors safely move the layers of muscles and the trachea along with the esophagus away from the surgical site. Once the disc and vertebrae are located, the damaged parts are removed, and a bone graft is placed in the newly formed cavity to help the healing and fusion. Metal plates are lined on the bone to ensure proper alignment. At the end of the surgery, the layers of muscle, the trachea, and the esophagus are carefully put back in place [6].
There is a similar procedure that approaches the spinal cord from the posterior side. The type of approach depends on what works best for each patient. For instance, a posterior cervical discectomy and fusion (PCDF) is a more common approach for lateral herniated discs. Luckily, there are multiple treatment options that a clinician may opt to recommend. Both the anterior cervical discectomy and fusion and the PCDF are standard procedures with decades of research to back them up, each with detailed benefits and risks associated with both. The ACDF surgery seems to present less trauma to large posterior neck muscles and lower mean reoperation rates [10]. The PCDF surgery has indicated a lower mean post-operative complication rate in seven studies [10].
Outcomes & Recovery
The vast majority of ACDF patients say they consider the surgery a successful procedure. For a standard ACDF, the usual recovery period is 8-12 weeks with a mean return to work of around 11 weeks [11]. Throughout this period, patients may have restrictions on neck mobility, and they may have short term difficulty swallowing. Post-operative wound infections are rare, and some studies indicate that 0.1 - 1.6% of all ACDF cases become infected [12]. Even then, these infections occur in the early stages of postoperative care. These surgeries may seem daunting, but the research indicates that relatively few patients experience significant complications.
Future of Cervical Spinal Cord Treatments: ACDF, Slight Modifications, Alternative Procedures
The field of surgery is always expanding with new advances and promising research to treat cervical myelopathy or radiculopathy. One study compared two patient population ACDF groups, one that underwent a double horizontal incision and one that underwent a vertical incision. It was found that the patient population group that underwent double horizontal incision had better cosmetic results according to patient survey as well as less difficulty swallowing than the vertical group [13]. Another promising advancement involves engineering different cages for the fusion in ACDF, which has produced a zero-profile cage that prolongs alignment of the spine [14]. A zero-profile cage could be thought of as a more efficiently designed spacer that reduces complications. Other minimally invasive approaches such as modifications to ACDFs are constantly being explored and have shown promising results in terms of lowering hospitalization and lowering risk of complications for the patients [15]. Entirely different surgical procedures to treat disc damage have been explored and utilized to similar complication rates as traditional ACDF procedures. A minimally invasive posterior cervical foraminotomy is a procedure that enlarges the vertebral opening of a nerve in the neck to decompress it. This approach utilizes a smaller opening to enter the spine leading to less tissue damage [16].
EC-IC Bypass & Craniotomy
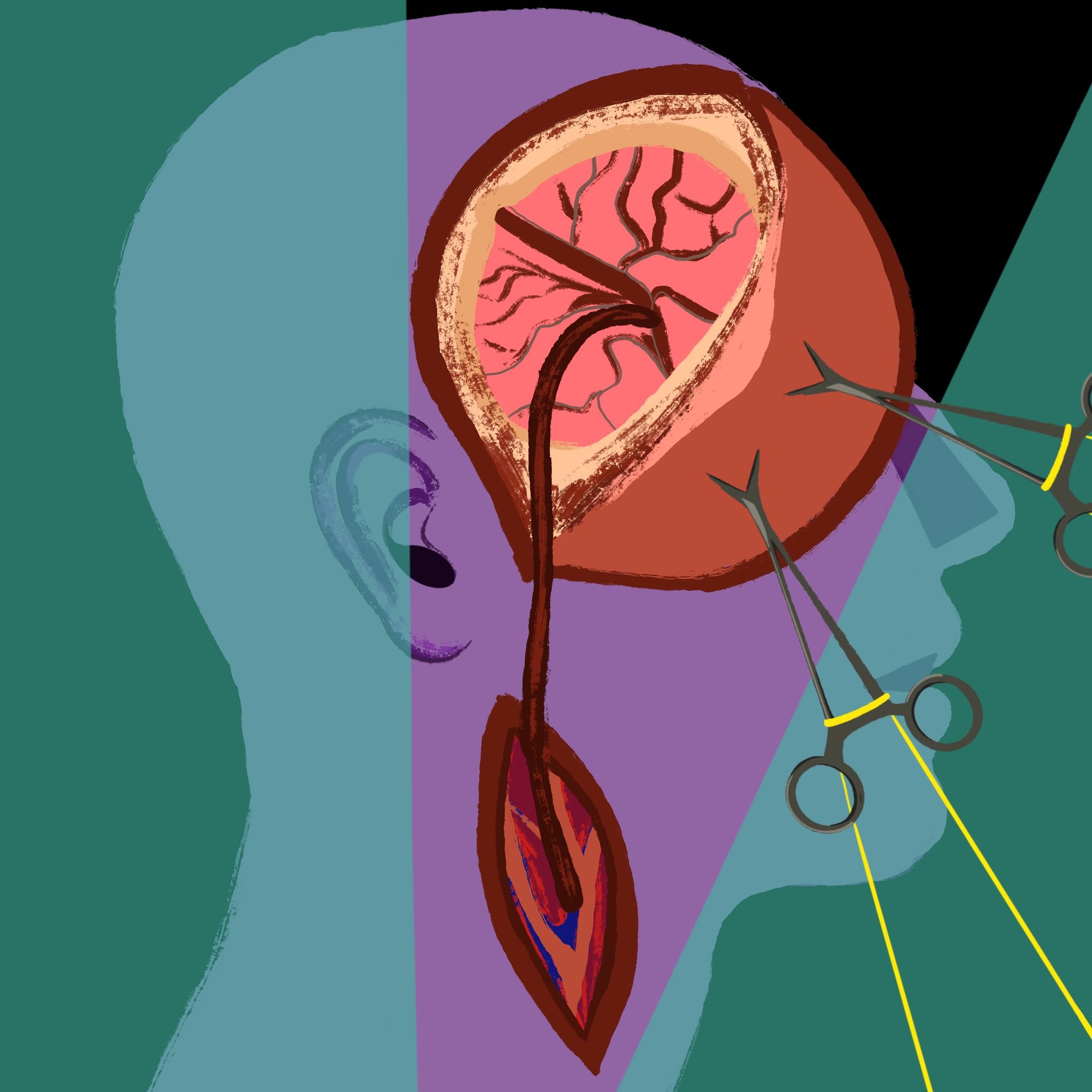
The brain relies on about 616 to 781 milliliters of blood flow per minute to function normally [17]! The brain is so metabolically demanding that loss of blood to any region of the brain may cause permanent damage within minutes. Such is the case in ischemic strokes where cerebral arteries are blocked or narrowed. One of the current standards used to treat these blockages is an extracranial-intracranial bypass (EC-IC bypass). Extracranial and intracranial refers to a blood vessel harvested from outside (Extra-) of the brain to connect to a blood vessel inside (Intra-) of the brain to bypass the blocked vessel. To do so, surgeons must also perform a craniotomy, meaning that a part of the skull is removed, to gain access to the impaired artery.
Just as the spinal vertebrae protects the spinal cord, the skull protects your brain from impact and collision. There are a few considerations for a craniotomy regarding the hair, scalp, skull, and dura mater, the protective tissue surrounding the brain [18]. The hair can be shaved off in the preparatory process before surgery. Some patients may be worried about the effect of the surgery on their hair, but even in rare instances of scar alopecia, hair transplant treatments have led to similar hair densities pre-operation [19]. The incision of the scalp must be carefully considered as to not damage the vasculature that delivers blood to those regions, especially if this is a repeated craniotomy or if the patient has had an incision in a similar place before. There should also be care taken to avoid damaging both the sensory and motor nerves in those regions. The next step is to remove the actual skull. A high-speed drill helps remove the bone flap [20]. This flap is kept neatly to the side until it is time to close the hole. Then, the dura mater is cut and placed to the side, exposing the brain tissue. This creates a window to explore the vasculature of the brain [21].
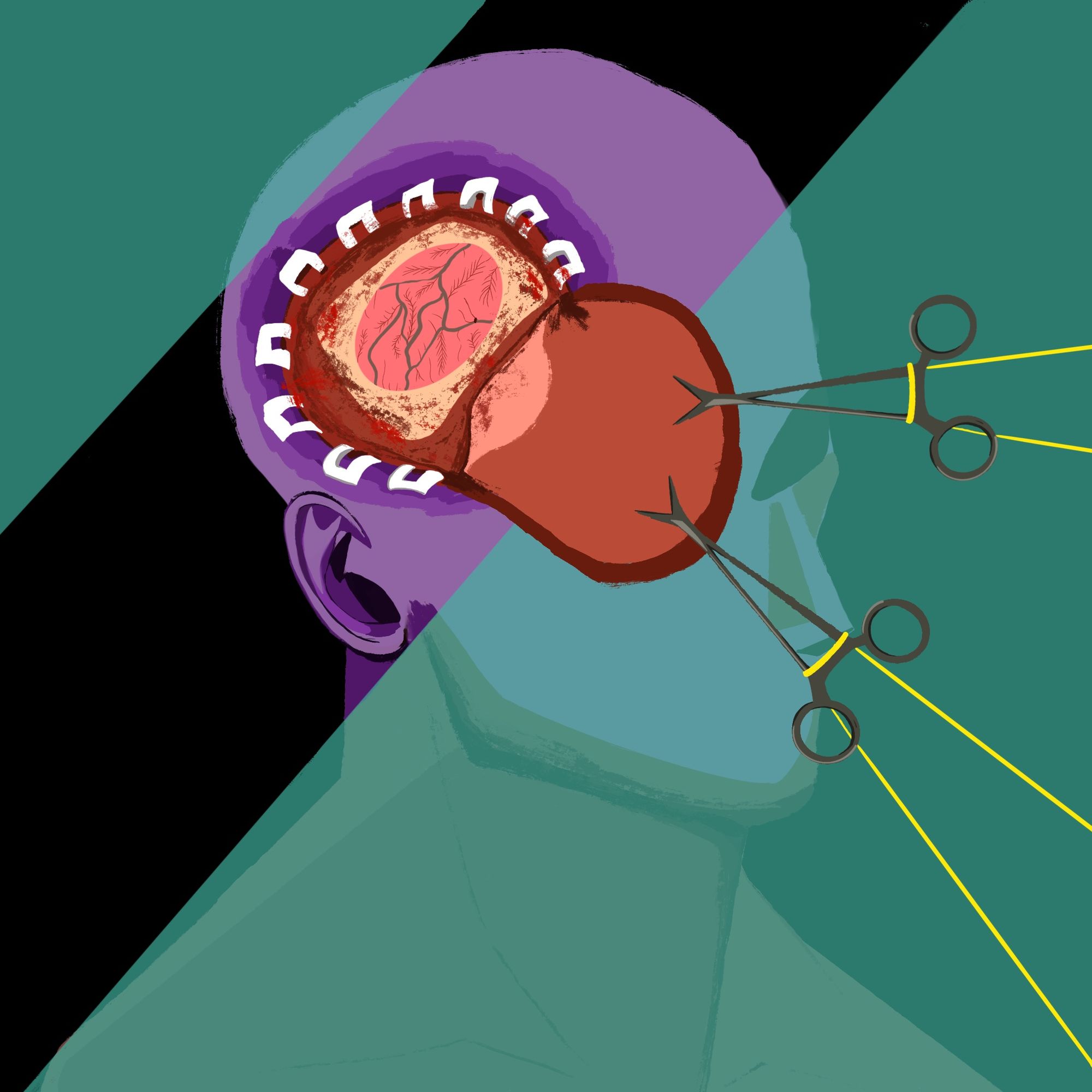
At the site of the harvest vessel, an incision is made to access the blood vessel. The blood vessel is then cut and the ends are prepared on the operating table. One of the most common cerebral arteries involved in strokes is the middle cerebral artery (MCA) [22]. The MCA is very important, delivering blood to the middle of the brain, primarily the motor and somatosensory cortices. It is often a site where the harvested vessel is sutured onto to bypass an occlusion. The MCA is clamped to stop blood flow, and a cut is made to help allow the vessels to connect. The two vessels are then sutured together. After removing the clamps on the blood vessel and verifying leakage using ultrasound or special fluorescent dyes, the dura mater is closed, and the bone flap is placed back with metal screws [21].
What Vessels are Usually Harvested?
The extracranial blood vessel that is used in the bypass should meet two main criteria: first, adequate blood flow through the vessel must be achieved, and second, there needs to be a high rate of graft success. Two common extracranial blood vessels used are the radial artery (RA) of the forearm and the saphenous vein in the leg. These vessels are easy to use, versatile, and have shown better post-operative outcomes in patients [23]. The ulnar nerve in the forearm helps provide adequate blood flow in a RA harvest.
Outcomes & Future Improvements
One important finding from several randomized clinical trials is that the EC-IC bypass did not show a statistical benefit in preventing strokes or death [24]. This puts into question the efficacy of this surgery compared to other treatment plans for strokes.
There has been an effort and a subsequent improvement to the ways we can treat blocked arteries in the brain. Currently, indirect revascularizations are being explored as an alternative to the direct revascularization of the EC-IC bypass [25]. New stent delivery systems may make it possible to treat a wider range of cases [25]. In the future, we may have a more expansive toolbox to choose from.
Conclusion: Inequalities, Disparities, & Limitations
Neurosurgery may be the oldest documented surgical practice [3], but there is still so much room for improvements. Modern neurosurgery still has its limitations and disparities. Many of the previously mentioned studies presented in this article utilizes smaller case studies with vastly different demographics and sample sizes. Many individual studies also employ differing metrics to analyze their data on patient outcomes, which makes it a bit harder to understand for a patient or general audiences.
For instance, in one study, Black and Hispanic patients were found to be significantly more likely to experience more severe spine disease impairments after ACDF [7]. This is not okay. There has been a concerted effort to improve the field that may yield more positive and equitable outcomes though. Neurosurgery continues to evolve each year. Notably, the field has seen an increase in gender diversity, with women matching into neurosurgery residencies at a rate of 18.8% from 2010 to 2019, compared to 12% from 2000 to 2009 [26]. It is beautiful to see the constant desire for the growth of neurosurgery because despite the current limitations, the field is always expanding to improve patient outcomes because that has always been, is, and will be the purpose of modern neurosurgery.
References
[1] Faria, Miguel A. “Neolithic trepanation decoded- a unifying hypothesis: Has the mystery as to why primitive surgeons performed cranial surgery been solved?” Surgical Neurology International, vol. 6, no. 1, 7 May 2015, p. 72, https://doi.org/10.4103/2152-7806.156634.
[2] Kleisiaris, Christos F et al. “Health care practices in ancient Greece: The Hippocratic ideal.” Journal of medical ethics and history of medicine vol. 7 6. 15 Mar. 2014
[3] Gilard, Vianney, et al. “Precision neurosurgery: A path forward.” Journal of Personalized Medicine, vol. 11, no. 10, 12 Oct. 2021, p. 1019, https://doi.org/10.3390/jpm11101019.
[4] Dewan, Michael C., et al. “Global neurosurgery: The current capacity and deficit in the provision of essential neurosurgical care. executive summary of the global neurosurgery initiative at the program in Global Surgery and social change.” Journal of Neurosurgery, vol. 130, no. 4, 1 Apr. 2019, pp. 1055–1064, https://doi.org/10.3171/2017.11.jns171500.
[5] Smith, Alexander D., et al. “The neurosurgeon workforce: A geographical gender-focused analysis of the trends in representation of neurosurgeons and choices in training over 70 years.” Neurosurgical Focus, vol. 55, no. 5, Nov. 2023, https://doi.org/10.3171/2023.8.focus23473.
[6] Rhee, John M., and Kevin L. Ju. “Anterior cervical discectomy and fusion.” JBJS Essential Surgical Techniques, vol. 6, no. 4, 9 Nov. 2016, https://doi.org/10.2106/jbjs.st.15.00056.
[7] Das, Ankita, et al. “Disparities in anterior cervical discectomy and fusion provision and outcomes for cervical stenosis.” North American Spine Society Journal (NASSJ), vol. 14, Apr. 2023, p. 100217, https://doi.org/10.1016/j.xnsj.2023.100217.
[8] Fluri, Felix, et al. “Extracranial-intracranial arterial bypass surgery for occlusive carotid artery disease.” Cochrane Database of Systematic Reviews, 17 Feb. 2010, https://doi.org/10.1002/14651858.cd005953.pub2.
[9] Fakhoury, Jordan, and Thomas Dowling. “Cervical Degenerative Disc Disease.” StatPearls, U.S. National Library of Medicine, 14 Aug. 2023, www.ncbi.nlm.nih.gov/books/NBK560772/.
[10] Liu, Wei‐jun, et al. “Comparison of anterior cervical discectomy and fusion versus posterior cervical foraminotomy in the treatment of cervical radiculopathy: a systematic review.” Orthopaedic Surgery, vol. 8, no. 4, 29 Nov. 2016, pp. 425–431, https://doi.org/10.1111/os.12285.
[11] De Biase, Gaetano, et al. “Postoperative restrictions after anterior cervical discectomy and fusion.” Cureus, 3 Aug. 2020, https://doi.org/10.7759/cureus.9532.
[12] Jin, Sung-Won, et al. “Late infection from anterior cervical discectomy and fusion after twenty years.” Korean Journal of Spine, vol. 11, no. 1, 2014, p. 22, https://doi.org/10.14245/kjs.2014.11.1.22.
[13] Lee, Hyung Rae, et al. “What type of incision for anterior cervical spine surgery involving long segments can bring better cosmetic and functional outcomes?” Neurospine, vol. 19, no. 2, 30 June 2022, pp. 412–421, https://doi.org/10.14245/ns.2143260.630.
[14] Yin, Mengchen, et al. “The new zero-P implant can effectively reduce the risk of postoperative dysphagia and complications compared with the traditional anterior cage and plate: A systematic review and meta-analysis.” BMC Musculoskeletal Disorders, vol. 17, no. 1, 18 Oct. 2016, https://doi.org/10.1186/s12891-016-1274-6.
[15] Kim, Lily H, et al. “Anterior techniques in managing cervical disc disease.” Cureus, 14 Aug. 2018, https://doi.org/10.7759/cureus.3146.
[16] Huang, Chuan-Ching, et al. “Evolution of cervical endoscopic spine surgery: Current progress and Future Directions—A narrative review.” Journal of Clinical Medicine, vol. 13, no. 7, 6 Apr. 2024, p. 2122, https://doi.org/10.3390/jcm13072122.
[17] Zarrinkoob, Laleh, et al. “Blood flow distribution in cerebral arteries.” Journal of Cerebral Blood Flow & Metabolism, vol. 35, no. 4, 7 Jan. 2015, pp. 648–654, https://doi.org/10.1038/jcbfm.2014.241.
[18] Rao, Dinesh, et al. “An illustrative review of common modern craniotomies.” Journal of Clinical Imaging Science, vol. 10, 10 Dec. 2020, p. 81, https://doi.org/10.25259/jcis_176_2020.
[20] Thanapal, Sengottuvel, et al. “Direct cerebral revascularization: Extracranial-intracranial bypass.” Asian Journal of Neurosurgery, vol. 13, no. 01, Mar. 2018, pp. 9–17, https://doi.org/10.4103/ajns.ajns_76_17.
[21] Joshi, Girish, et al. “EC-IC Bypass; our experience of cerebral revascularization with intraoperative dual-image video angiography (DIVA).” Asian Journal of Neurosurgery, vol. 15, no. 03, Sept. 2020, pp. 499–506, https://doi.org/10.4103/ajns.ajns_84_20.
[22] Nichols, Larry, et al. “Where in the brain do strokes occur? A pilot study and call for Data.” Clinical Medicine & Research, vol. 19, no. 3, 13 May 2021, pp. 110–115, https://doi.org/10.3121/cmr.2021.1632.
[23] Tatoulis, James. “The radial artery: An important component of multiarterial coronary surgery and considerations for its Optimal Harvest.” JTCVS Techniques, vol. 5, Feb. 2021, pp. 46–55, https://doi.org/10.1016/j.xjtc.2020.10.042.
[24] Ma, Yan, et al. “Extracranial-intracranial bypass in patients with symptomatic artery occlusion—reply.” JAMA, vol. 330, no. 24, 26 Dec. 2023, p. 2396, https://doi.org/10.1001/jama.2023.22002.
[25] Elder, Theresa A., et al. “Future of endovascular and surgical treatments of atherosclerotic intracranial stenosis.” Stroke, vol. 55, no. 2, 23 Jan. 2024, pp. 344–354, https://doi.org/10.1161/strokeaha.123.043634.
[26] Smith, Eleanor C., et al. “Fueling the future of neurosurgery: Increasing trends in female enrollment expanding the neurosurgical workforce from 2010 to 2019.” Journal of Neurosurgery, vol. 141, no. 5, 1 Nov. 2024, pp. 1427–1432, https://doi.org/10.3171/2024.4.jns24158.
