Introduction
Look up at the sky. It’s not the usual color. Instead, the blues and purples swirl together, some pink blurs across, pulsing and shimmering as if it were speaking to you. Now close your eyes. It’s not dark. There are patterns, the fractals seen in a kaleidoscope. Swirling and mixing and changing all at the same time every time you take a breath. Inhale, exhale, inhale, exhale. Jolts of energy rush through your body, from your shoulders to your stomach all the way down to your feet [1]. Everything vibrates, everything is connected, and you are in the center of it. You are a part of everything. You feel a sense of peace, but overwhelming emotion at the same time [2]. But it’s okay, it’s beautiful. You are no longer a part of yourself, subject to your own body. You are part of the world, the fibers of the universe, and you see it all so clearly. Welcome to the psilocybin trip.

These other-world mystical experiences caused by “Magic Mushrooms” have been known and documented for hundreds of years [3]. They are now making their way into modern medicine. Due to its abilities to increase neuroplasticity and act in a prolonged and effective manner, psilocybin is being researched as an alternative for treatment-resistant depression in conjunction with talking therapy.
Psilocybin and early uses
Hallucinogenic mushrooms, also called magic, medicinal, psychedelic, or sacred mushrooms, are naturally found in the forest floors of Central America, Mexico, and the Pacific Northwest [3]. These mushrooms contain a psychedelic substance known as psilocybin, though its concentration varies based on the species of the fungus. Psilocybin induces psychic effects and changes in consciousness and cognition by altering a person’s sense of time, emotion, perception, and sense of self. The most potent form of psilocybin is found in the Psilocybe genus of mushrooms [3].
Before adopting the colloquial moniker of the “Magic Mushroom,” these hallucinogenic mushrooms were widely used in religious and healing rituals in many indigenous cultures. The earliest uses of psilocybin mushrooms were recorded in the early 1500s in Mesoamerica by the Mixtec indigenous group. In ceremonies surrounding psilocybin rituals, participants would work towards gaining an internal sense of spiritual presence and access to the spiritual world. Aside from its religious use, many Latin American cultures would employ psilocybin as a medical aid for bodily ailments, anxiety, and chronic diseases. In Mexico, ancient texts reference approximately 57 species of hallucinogenic Psilocybe mushrooms, 35 species and nine varieties of which were reported to be used by ethnic groups mainly in central and southern Mexico [4,5].

Until the 19th century, the use of hallucinogenic mushrooms was denied worldwide by scientists and historians. Even after the existence of psychedelic fungi was confirmed by researchers, its use in medicine was heavily stigmatized throughout the 1950s and 1960s due to its derogatory association with “hippies.” In the 1970s, the Controlled Substances Act banned psilocybin, claiming it had a high potential for abuse and could not be accepted for medical use, and, as a result, all psilocybin-related experiments came to a complete halt. It was only recently that research regarding the therapeutic benefits of psilocybin restarted. Furthermore, the legal status of psilocybin has changed in the past five years, modeled after the legalization of medical cannabis. Now psilocybin is available to use in research, specifically in Michigan, Oregon, Minnesota, and Washington, to better understand its therapeutic effects on the brain and nervous system [3].
Neuroplasticity and Depression
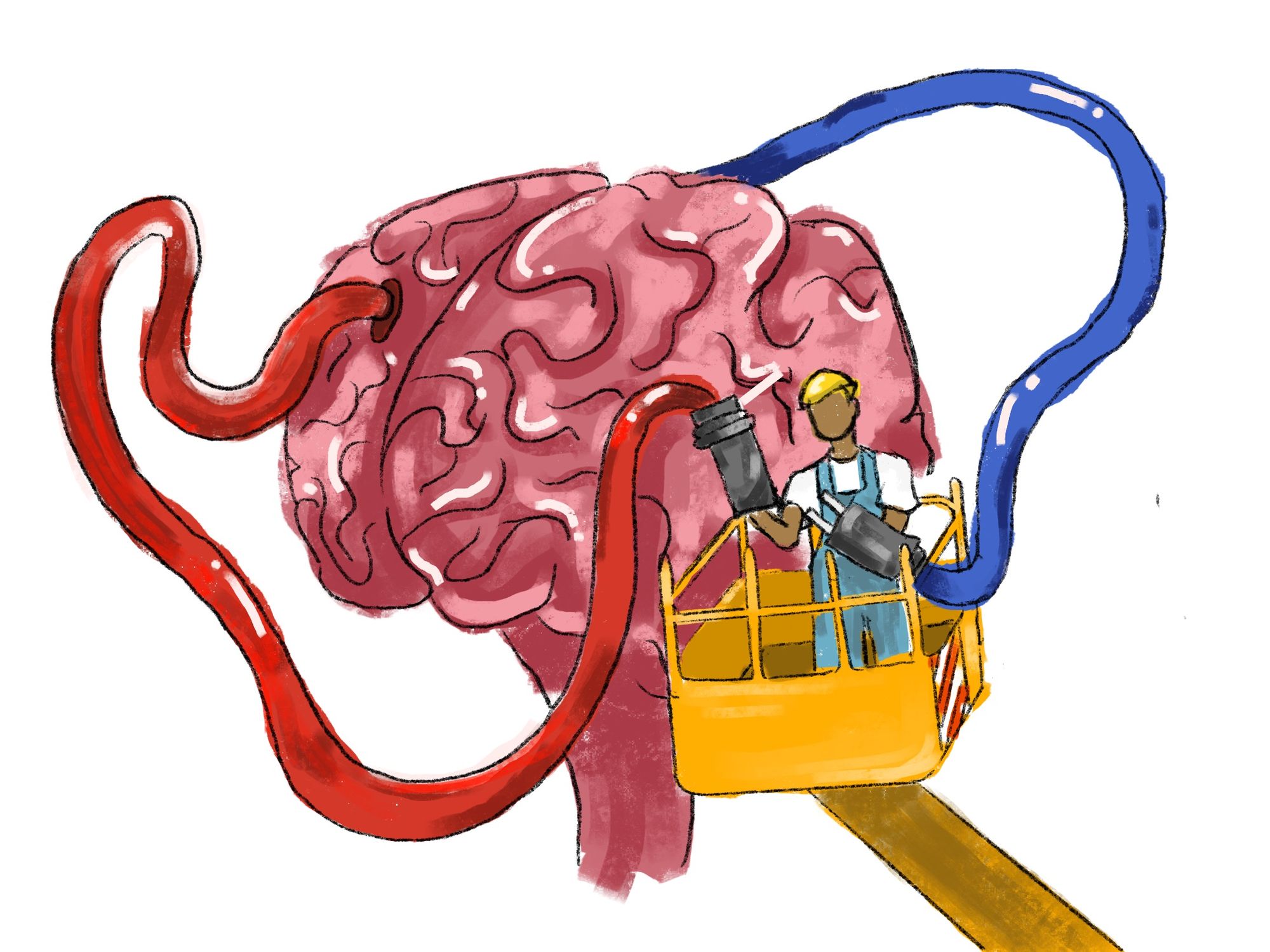
Our brains’ have the ability to learn and adapt by changing the strength of connections between the neurons that send signals throughout our body. This is called neuroplasticity.
A fundamental property of neurons is their ability to modify their strength and efficacy of communication through different activity-dependent mechanisms, a phenomenon referred to as synaptic plasticity. The synapse is a specialized gap between two neurons, where chemical messengers known as neurotransmitters travel from one neuron to another, leading to neuronal activation [6]. Synaptic plasticity is incredibly important for learning new skills, forming memories, and rehabilitation after traumatic brain injuries such as stroke or seizure [7]. Neuroplasticity is now being studied in the context of mental health.
As such, the relevance of neuroplasticity for depression, one of the most common mental health disorders, is being thoroughly researched. According to the Diagnostic and Statistical Manual of Mental Disorders - Edition 5 (DSM-5), a depressive disorder is characterized by physical and mental impairment, psychiatric and substance abuse disorders, poor health, mortality, and economic and social burdens [8]. For many decades, various researchers have sought to study the effect of depression on the brain. In the late 1900s, it was thought that imbalances in serotonin (5-hydroxytryptamine or 5-HT) levels could be correlated with depressive behaviors, with researchers theorizing that diminished activity of serotonin pathways plays a strong role in depressive behaviors arising in patients [9]. Many studies validate this claim, finding serotonin affects the mood of previously depressed patients, thus explaining the use of selective serotonin reuptake inhibitors (SSRIs) as a possible antidepressant because they artificially increase the amount of the neurotransmitter active at the synapse of neurons.
Many mood disorders, including depression, show alterations in intracellular signaling, gene expression, neurotrophic factors, neurogenesis, neuroinflammation, neurotransmission, synaptic number, and synaptic function [10]. Furthermore, decreased brain volume in the limbic system is likely to explain how depressive symptoms affect key structures [11]. All of these compounded factors impair neuroplasticity in an individual. These changes have been described in several brain regions implicated in depression such as the emotion-regulating prefrontal cortex (PFC) and memory-regulating hippocampus.
Moreover, chronic stress from depression leads to sustained decreases in protective protein expression and signaling, also resulting in damaged or hindered plasticity abilities [11]. This can further cause neural atrophy and decreased synaptic number and function. With this in mind, it is no surprise that magnetic resonance imaging results of the brains of depressed individuals show decreased hippocampal and PFC volume [12]. Volumetric changes lead to decreased functional connectivity within and between the PFC and limbic networks, which is important because these structures have a direct correlation to the degree of neuroplasticity in one's brain.
As a hallucinogenic drug, psilocybin temporally affects one’s perception of reality. When psychedelics are ingested, they interact with brain receptors [13]. Receptors are molecules inside or on the surface of a cell that bind to a specific substance and cause a reaction in the cell, which can either have a positive or negative effect depending on what is binding to the receptor. Psilocybin and most other psychedelics are most openly received by a serotonin receptor known as 5-HT2A. These receptors activate a signaling molecular acid that has been found to increase the neuroplasticity of the brain. Psilocybin specifically increases a chemical transmitter called glutamate, which is thought to be important for psychedelic-enhanced neuroplasticity [13]. Glutamate is an excitatory neurotransmitter and the transmission of glutamate is modulated by serotonin, thus linking glutamate to depressive behavior in individuals [14].
As mentioned before, the PFC and hippocampus have both been found to have decreased volume in patients with depression, which make them key structures for observation in experiments [15]. In the PFC, several psychedelics have been shown to increase the expression of genes linked to neuroplasticity. On the other hand, the effects of psychedelics on the hippocampus were less pronounced, perhaps partially due to fewer 5-HT2A receptors in the hippocampus compared to the PFC. However, psilocybin specifically has been shown to strengthen connections in a particular circuit of the hippocampus that is related to memory formation and retrieval [15].
Psilocybin as a Treatment for Depressive Disorders
Since depression tends to decrease brain volume and neuroplasticity while psilocybin has been shown to increase neuroplasticity, researchers are studying the use of psilocybin as an antidepressant treatment. Other unorthodox treatments for depression have shown promise before. For example, the drug ketamine can rapidly improve symptoms for patients with treatment resistant depression; however, the therapeutic effects of the drug typically last one week after the initial administration [16]. A group of scientists from the Amsterdam University Medical Center directly compared ketamine and psilocybin in regard to their therapeutic and antidepressant effects and found many differences between the short-term and long-term effects of psilocybin and ketamine [17]. In one experiment, researchers compared healthy mice, who were injected with saline solution, with mice that were injected with hydrocortisone (CORT) to induce a persistent depressive state [18]. A single dose of psilocybin was administered to both these groups. In healthy mice, the effects of psilocybin were measured through an open-field test. In this test, mice were allowed to move freely in a plastic box and researchers measured the average total distance traveled by the mice. “Depressive,” mice behavior was measured through a sucrose preference test. The open field test resulted in a positive experience in normal mice as their motor activity was not altered, suggesting psilocybin did not hinder the mice’s normal behavior. Mice that received CORT were divided into groups based on psilocybin concentration. After CORT administration, mice had a decreased sucrose preference, a result that is indicative of depressive behavior. However, once psilocybin was administered, sucrose preference of mice increased, implying psilocybin is effectively acting as an antidepressant. Neuroplasticity was measured through the total number of dendritic branches, synaptic protein levels, and signaling pathway activation in the PFC and hippocampus. Dendritic branches are of interest as this process allows neurons to form new synapses. In both normal and “depressive” mice, there was an increase in all these factors, leading researchers to believe there was an increase in neuroplasticity in both groups, likely due to the psilocybin administration. The effects of the psilocybin were rapid and sustained 12 hours after initial administration. These results persisted one month after the initial injection [18].
Building upon previous animal studies, in 2019, a clinical trial was conducted by a team of researchers at Johns Hopkins [19]. Participants aged between 21 and 75 with Major Depressive Disorder (MDD) were asked to withhold from consuming antidepressants throughout the experiment. Individuals were administered psilocybin in two sessions and were assisted with psychotherapy. Results were measured with the GRID-Hamilton Depression Screening (GRID-HAMD) and the Quick Inventory of Depressive Symptomatology (QIDS-SR). The GRID-HAMD is a clinician-administered survey with a grid-like scoring chart [20]. Scoring a zero correlates to absent symptoms of depression; scoring a five results in very severe symptoms of depression [21]. The QIDS-SR is a self-administered survey with scores ranging from 0-27, with scores greater than 11 correlating to moderate to severe depression [21]. The trial documented rapid antidepressant effects from psilocybin, similar to that of ketamine, suggesting that psilocybin may have therapeutic benefits for individuals with MDD. However, the length of these effects differed between ketamine and psilocybin: the effects of ketamine typically last for a few days up to two weeks maximum, while the response to psilocybin therapy persists for at least four weeks. Psilocybin was also found to have a lower potential for addiction and fewer side effects. The most common issues reported by participants were mild to moderate headaches and challenging emotions, such as anxiety and suicidal ideation. Both issues were limited to the time of sessions with psilocybin [19].
A more recent trial in August 2023 achieved similar results. 104 participants aged between 21 and 65 years old who met the criteria for MDD were split into groups, one receiving 25 mg of psilocybin and the other receiving a placebo and both administered with psychological counseling [22]. Those in the psilocybin group experienced a clinically significant reduction in depressive symptoms when compared to those who had just received the placebo. Moreover, improvements in depression were apparent within eight days of dose administration, which is consistent with the rapid onset action of psilocybin found in other studies. The improved behavior of patients was also maintained across the six-week follow-up period. Furthermore, the researchers found psilocybin treatment improved psychological functioning, reducing overall disease severity and anxiety [22]. However, while the conclusions from this study are exciting, the experiment itself has major flaws. Patients, due to the effects of psilocybin administration, almost certainly know which group they are in. Therefore, the study lacks a truly double-blind placebo. This will likely affect the results as the placebo effect can be potent [23].
These studies all suggest psilocybin acts in a rapid and sustained manner, with patients feeling the antidepressant effects in as little as twenty-four hours and the therapeutic effects being persistent for as long as six weeks. Psilocybin also has a low potential for addiction and minimal side effects. While ketamine also acts rapidly, its therapeutic effects lasting only two weeks in addition to its potentially high abuse rate and detrimental side effects makes psilocybin the more attractive antidepressant. That being said, the balance between distressing and therapeutic effect is dependent on the complex interaction between patient, therapists, expectancy, readiness, and ability to fully surrender to the experience and treatment [24].
Future of Psilocybin in Medicine
While psilocybin shows great promise for depression treatment, its use can be expanded to other areas of psychological care.
For instance, psilocybin is being looked into as a treatment for substance abuse disorders [25]. Its low abuse potential and short half-life of three hours make it more desirable compared to psychedelics with lower elimination and longer duration of action. Researchers have also seen that only two or three administrations of psilocybin will cause long-term or even permanent beneficial effects, in comparison to methadone, which is taken daily for treatment of opioid use disorder [25].
Future research studying psilocybin and MDD should take more interest in how this treatment works for various people. An important part of making a treatment with psychedelics work is having the patient fully immerse themselves in the therapy and experience. It would be extremely beneficial for researchers to conclude which patients are best suited, what experimental design will be conclusive, and how long the benefits last in the context of psilocybin-treated MDD.
Conclusion
For centuries, psilocybin has been stigmatized as a harmful recreational drug. Today, the medical field is experiencing a resurgence of interest in psilocybin, recognizing the amazing potential it has to improve medical accessibility and efficiency. Psilocybin’s incredible ability to increase the degree of neuroplasticity and have a prolonged and rapid effect on individuals makes its future as an antidepressant promising.
References
- Back, A. L. (2020). What psilocybin taught me, one year later. Journal of Palliative Medicine, 23(8), 1130–1131. https://doi.org/10.1089/jpm.2020.0018
- Ross, S., Bossis, A., Guss, J., et al. (2016). Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: A randomized controlled trial. Journal of Psychopharmacology, 30(12), 1165–1180. https://doi.org/10.1177/0269881116675512
- Sharma, P., Nguyen, Q. A., Matthews, S. J., et al. (2023). Psilocybin history, action and reaction: A narrative clinical review. Journal of Psychopharmacology, 37(9), 849–865. https://doi.org/10.1177/02698811231190858
- Pepe, M., Hesami, M., de la Cerda, K. A., et al. (2023). A journey with psychedelic mushrooms: From historical relevance to biology, cultivation, medicinal uses, biotechnology, and beyond. Biotechnology Advances, 69. https://doi.org/10.1016/j.biotechadv.2023.108247
- Van Court, R. C., Wiseman, M. S., Meyer, K. W., et al. (2022a). Diversity, biology, and history of psilocybin-containing fungi: Suggestions for research and technological development. Fungal Biology, 126(4), 308–319. https://doi.org/10.1016/j.funbio.2022.01.003
- Nesterova, A. P., Klimov, E. A., Zharkova, M., Sozin, S., et al. (2020). Diseases of the nervous system. Disease Pathways, 219–258. https://doi.org/10.1016/b978-0-12-817086-1.00005-1
- Mateos-Aparicio, P., & Rodríguez-Moreno, A. (2019). The impact of studying brain plasticity. Frontiers in Cellular Neuroscience, 13(66). https://doi.org/10.3389/fncel.2019.00066
- Hasin, D. S., Sarvet, A. L., Meyers, J. L., et al. (2018). Epidemiology of adult dsm-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry, 75(4), 336–346. https://doi.org/10.1001/jamapsychiatry.2017.4602
- Cowen, P. J., & Browning, M. (2015). What has serotonin to do with depression? World Psychiatry, 14(2), 158–160. https://doi.org/10.1002/wps.20229
- Price, R. B., & Duman, R. (2019). Neuroplasticity in cognitive and psychological mechanisms of depression: An integrative model. Molecular Psychiatry, 25(3), 530–543. https://doi.org/10.1038/s41380-019-0615-x
- Chakrapani, S., Eskander, N., De Los Santos, L. A., et al. (2020). Neuroplasticity and the biological role of brain derived neurotrophic factor in the pathophysiology and management of depression. Cureus, 12(11). https://doi.org/10.7759/cureus.11396
- Schmaal, L., Veltman, D. J., van Erp, T. G., Sämann, et al. (2015). Subcortical brain alterations in major depressive disorder: Findings from the Enigma Major Depressive Disorder Working Group. Molecular Psychiatry, 21(6), 806–812. https://doi.org/10.1038/mp.2015.69
- Calder, A. E., & Hasler, G. (2022). Towards an understanding of psychedelic-induced neuroplasticity. Neuropsychopharmacology, 48, 104–112. https://doi.org/10.1038/s41386-022-01389-z
- Xie, G., Zuo, W., Wu, L., et al. (2016). Serotonin modulates glutamatergic transmission to neurons in the lateral habenula. Scientific Reports, 6. https://doi.org/10.1038/srep23798
- Davis, C. (2023). Effects of microdosing with psilocybin mushrooms . The Science Journal of the Lander College of Arts and Sciences, 17(1), 59–67. https://doi.org/https://touroscholar.touro.edu/sjlcas/vol17/iss1/8
- Matveychuk, D., Thomas, R. K., Swainson, J., et al. (2020a). Ketamine as an antidepressant: Overview of its mechanisms of action and potential predictive biomarkers. Therapeutic Advances in Psychopharmacology, 10. https://doi.org/10.1177/2045125320916657
- Dahan, J. D., Dadiomov, D., Bostoen, T., & Dahan, A. (2024). Meta-correlation of the effect of ketamine and psilocybin induced subjective effects on therapeutic outcome. Npj Mental Health Research, 3. https://doi.org/10.1038/s44184-024-00091-w
- Zhao, X., Du, Y., Yao, Y., et al. (2024). Psilocybin promotes neuroplasticity and induces rapid and sustained antidepressant-like effects in mice. Journal of Psychopharmacology, 38(5), 489–499. https://doi.org/10.1177/02698811241249436
- Davis, A. K., Barrett, F. S., May, D. G., et al. (2021). Effects of psilocybin-assisted therapy on major depressive disorder. JAMA Psychiatry, 78(5), 481–489. https://doi.org/10.1001/jamapsychiatry.2020.3285
- Williams, J. B. W., Kobak, K. A., Bech, P., et al. (2008). The GRID-HAMD: Standardization of the Hamilton depression rating scale. International Clinical Psychopharmacology, 23(3), 120–129. https://doi.org/10.1097/yic.0b013e3282f948f5
- Weiss, B., Erritzoe, D., Giribaldi, B., et al. (2023). A critical evaluation of QIDS-SR-16 using data from a trial of psilocybin therapy versus escitalopram treatment for depression. Journal of Psychopharmacology, 37(7), 717–732. https://doi.org/10.1177/02698811231167848
- Raison, C. L., Sanacora, G., Woolley, J., et al. (2023). Single-dose psilocybin treatment for major depressive disorder. JAMA, 330(9), 843–853. https://doi.org/10.1001/jama.2023.14530
- Conti, A. (2024). The FDA rejected a psychedelic sponsor’s bid for approval. Here are six industry takeaways. AgencyIQ by POLITICO https://www.agencyiq.com/blog/the-fda-rejected-a-psychedelic-sponsors-bid-for-approval-here-are-six-industry-takeaways/
- Breeksema, J. J., Niemeijer, A., Krediet, E., et al. (2024). Patient perspectives and experiences with psilocybin treatment for treatment-resistant depression: A qualitative study. Scientific Reports, 14. https://doi.org/10.1038/s41598-024-53188-9
- Ziff, S., Stern, B., Lewis, G., et al. (2022). Analysis of psilocybin-assisted therapy in Medicine: A Narrative Review. Cureus, 14(2). https://doi.org/10.7759/cureus.21944