What are Organoids?
Since 2011, one or more neurological diseases have afflicted nearly 100 million Americans [1]. Unfortunately, unlocking the mysteries of the brain to begin to address and treat affected individuals is an expensive endeavor. Procuring brain tissue can set labs back tens of thousands of dollars [2]. Even animal models demand a hefty investment, with a single mouse costing up to $600 depending on maturity and genetic makeup [3]. But there's a more promising solution on the horizon.
Enter organoids, the cost-efficient game-changers of modern research. Organoids are three-dimensional cell cultures that are designed to mimic the structure and function of specific organs. These remarkable structures have greatly impacted various fields of biological research by offering a unique opportunity to study organ development, disease modeling, and drug testing in a controlled laboratory setting. Organoid stem cell cultures offer scientists a potentially more biologically representative approach compared to rodent models [4]. Organoids are also more cost-efficient, with the average kit, containing media, tissues, and other materials, costing approximately $400 and producing multiple organoids [4].
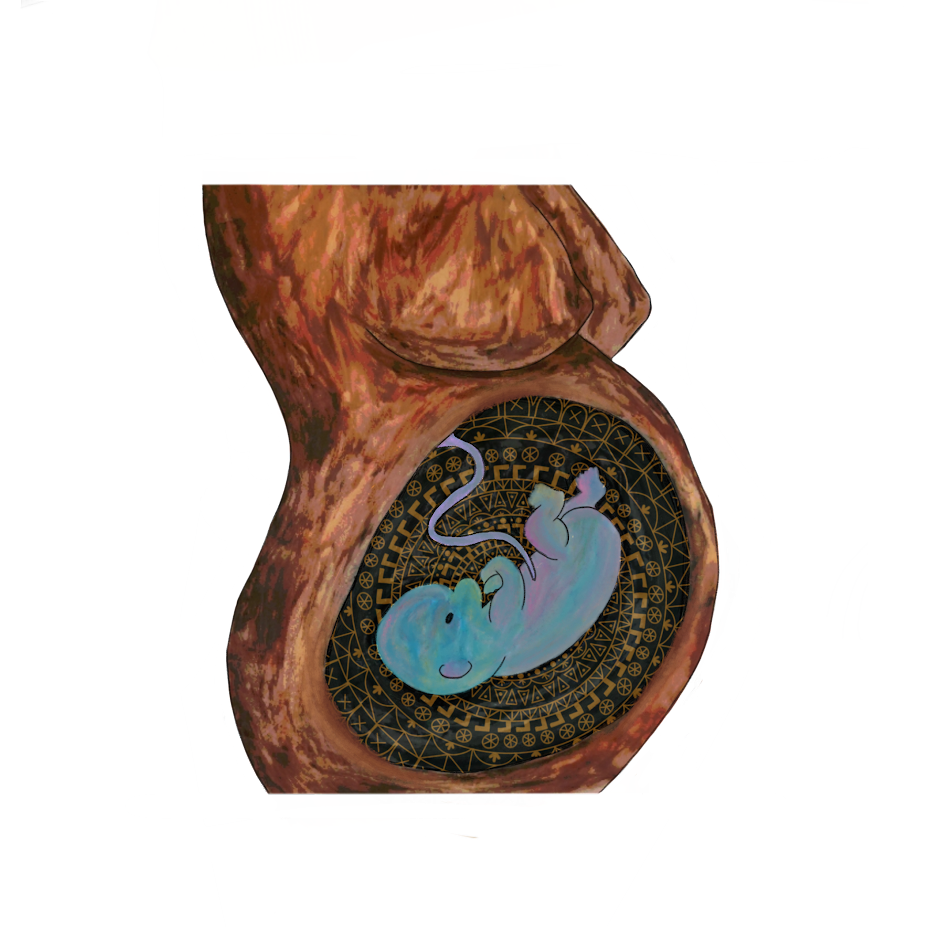
Not all organoids are equal - there is great diversity within the cell cultures used to make organoids, enabling them to be used in a variety of research settings. Some organoids are made using stem cells from adult tissue and treated in specific sets of chemicals that direct them to form new cell types [5]. In research on neurological disorders, patient stem cells and stem cells created from other types of patient cells are induced by different chemicals and growth factors to mimic normal cell development. These then become different types of brain cells, including support cells called glia and neurons, and come together in a way that mimics parts of the brain [5]. Overall, these 3D cultures could lead to a more comprehensive understanding of organ development, function, and disease pathology by providing a more accurate representation of conditions in the human body.
Organoid cultures were first introduced in a study published in 2005 that discussed the process of enabling the growth of brain cells in a controlled environment [6]. Developed by a lab in Japan, this technique helped scientists understand how different brain regions develop and communicate. Using advanced kits to manipulate embryonic stem cells into neural stem cells and then further into mature brain cell types, researchers could cultivate organoids that mimic the cerebral and midbrain regions of the brain [6]. By altering the culture conditions, they were able to generate specific types of brain cells, offering potential applications to better understand and develop new therapies for diseases that are hard to treat. Additionally, the study demonstrated that these artificially grown brain cells could form networks that mimic those that exist between brain regions, allowing different parts of the brain to work together to perform a specific task [6]. These miniature organ-like structures have provided a new avenue for research in neuroscience and regenerative medicine. The accessibility and specificity of organoids relative to other models of neurological systems make them a valuable contribution to neuroscience research, providing neuroscientists with a powerful tool to study the intricacies of the human brain, such as neural development, disease mechanisms, and potential therapeutic interventions.
Use of Organoids in Neuroscience Research
One of the most significant applications of organoids in neurological research is modeling brain development. This convergence has opened new pathways for understanding the complexities of neural development and neurological disorders [6]. The use of organoids could make up for gaps in research on the repercussions of genetic disorders on human brain development, which are difficult to produce and observe in animal models.
A study focused on primary microcephaly (MCPH), a neurodevelopmental disorder characterized by reduced brain size, found that organoid models offer a more accurate representation of the disease compared to mice with known mutations that cause MCPH [7]. Since the organoid models could be maintained longer than developing mouse brains, researchers were able to study MCPH development over extended periods and across various brain regions. When comparing both the organoids and rodent models for the presence of DNA markers of specific regions of the brain during development, researchers observed that the development of the organoids over time was more congruent with embryonic brain development than the rodent models. Even more significantly, when they stained different regions’ genetic cell markers, the different regions were organized separately but still communicated with one another, effectively modeling the complex interdependent relationships between different parts of the brain. This allowed the researchers to use lab-grown groups of cells derived from patients with MCPH to replicate symptoms of microcephaly and study the cause of the characteristic reduction of cells in tissues that result in smaller brain size [7]. Organoids can be used to investigate the previously inaccessible intricacies of the human brain, allowing researchers to explore the underlying mechanisms of various neurological conditions from their labs. However, they are not a perfect solution for expanding research on brain development, as inconsistencies and unpredictable variation across organoid cell lines and cultures make replicating and confirming findings very difficult.
Growing the cell cultures is one of the main challenges in organoid research, due to the lengthy and complex process of inducing differentiation and maturation of the stem cells. For example, cerebral organoids commonly used in research on neurological and neurodevelopmental disorders take nearly 11 weeks to fully mature [5]. However, the complexity of these cultures is what makes them such excellent models of the functional features of the brain, such as neural pathways and brain region formation. By chemically inducing pathways that cause stem cells to form specific cell types, researchers can guide human stem cells to mimic structural and functional characteristics of the human brain and utilize these structures to model complex diseases.
Disease Modeling
Neurological disorders encompass a broad spectrum of conditions affecting the nervous system, leading to various cognitive, motor, and sensory impairments. Affecting more than 12% of Americans of ages 65 and older since 2010 [8], Alzheimer’s and other dementia-related diseases have been notoriously difficult to treat because of the variance from patient to patient caused by a myriad of underlying causes and unknown genetic pathways. Stem cell research offers a promising platform for understanding the underlying mechanisms and development of these disorders, leading to potential therapeutic breakthroughs. Organoids provide a unique opportunity to study the cellular and molecular changes associated with neurological diseases, offering insights into disease progression and potential targets for intervention.
As of now, most of the information scientists have about Alzheimer's Disease (AD) comes from studies done on individuals with early-onset familial Alzheimer’s (fAD), a specific subtype of AD that occurs at a relatively young age and has a strong genetic component. During a study from 2016 conducted at the Tsai lab at MIT, researchers looked at the possible use of neural organoids made using stem cells from both fAD patients and healthy controls [9]. A common characteristic of Alzheimer's that researchers specifically looked at was the phenomena of proteins clumping together like Lego bricks to impede brain function, which causes memory problems and difficulty in thinking and reasoning. They found that both types of cultures could model this clumping, demonstrating the opportunity organoid models provide to study a specific characteristic of AD [9]. However, the translatability of this information into research that focuses on treating symptoms of the disease is minimal, due to the variation between organoids and the current inability to model complex interactions with them [10]. It is also difficult to model aging-related aspects of neurological disorders using these cell cultures, unlike with animal models [10]. Despite these shortcomings, organoids provide another valuable experimental model for studying the mechanisms underlying neurodegenerative diseases.
Development of Neurological Disorders
Advances in refining the organoid model for greater accuracy and reproducibility have paved the way for its expanded use in various fields of biomedical research. Researchers have used organoids to study the effects of viral infections and their connections with the development of various neurological conditions, including Miller-Dieker Syndrome (MDS). A defining characteristic of the brain is its walnut-like exterior, otherwise known as the cortex [11]. During fetal development, sometimes the ridges in the cortex, called cortical folds, do not fully develop. The resulting seemingly smooth brain, called lissencephaly, is a characteristic of MDS. Children born with MDS have a life expectancy of 3-10 years and often experience issues with cognitive functioning, learning, problem-solving and have epileptic seizures [12]. In a study conducted in 2016 by the Kriegstein Lab at UCSF, researchers used organoids derived from diseased and normal brain cells to investigate how brain cells move during brain development, and how this connects to lissencephaly [13]. The study found that non-diseased neurons moved efficiently away from the edge of the organoid to form the cortical folds, while neurons from individuals with Miller-Dieker Syndrome (MDS) showed limited migration, contributing to the smooth brain surface characteristic of the syndrome. Additionally, the study confirmed that the migration issues of MDS neurons were primarily due to intrinsic rather than problems within the neurons themselves. This process was visualized as a delicate balance akin to assembling complex structures, with the disrupted migration patterns resembling an incomplete puzzle [13]. Overall, this study suggests that these models hold immense promise in understanding not just neurological disorders but also broader aspects of human health and disease.
The use of organoids in this study to replicate the developmental processes of the brain highlights their pivotal role in unraveling the complexities of neurological disorders. By specifically mimicking the migration patterns of neurons in the context of Miller-Dieker Syndrome (MDS), organoids provided a controlled environment for understanding the intrinsic neuronal defects contributing to the syndrome's characteristic smooth brain surface. This demonstration emphasizes the overall capability of organoids to model intricate physiological processes, enabling researchers to gain deeper insights into the mechanisms underlying various developmental disorders. With such precise mimicry of conditions in the human body, organoid research can be extended to encompass a diverse range of applications, including the study of infectious diseases.
Recently, researchers at the University of Cologne were able to use organoids to explore the effect of the Zika virus on neural development and differentiation of neurons [14]. They found several important connections between the Zika virus (ZIKV) and microcephaly. By analyzing the effects of ZIKV on developing brain cells in organoids, the researchers found that the virus targeted rapidly dividing brain cells, leading to cells becoming too specific and maturing very early on, as well as appearing in reduced numbers [14]. This effect is similar to what is observed in individuals with genetic microcephaly, where brain cells exhibit structural defects that affect their ability to divide correctly. Understanding this similarity suggests that ZIKV might induce microcephaly by disrupting the normal developmental processes of the brain, resulting in impaired growth and development. This research sheds light on the potential mechanisms underlying ZIKV-induced microcephaly and underscores the importance of further investigating the link between viruses and developmental disorders, as well as exemplifies the unique way that organoids can help investigate these links [14].
Organoid research has emerged as a groundbreaking tool in understanding and addressing various complex neurological disorders. By mimicking the intricate physiological processes within the brain, organoids offer valuable insights into the cellular and molecular changes that occur as a result of neurological conditions like Alzheimer's and Parkinson’s. They provide crucial insights into the complexities of neurological disorders, facilitating the exploration of disease mechanisms and potential treatments. Moreover, their utility extends to studying the effects of infectious diseases on neural development, contributing to a deeper understanding of the intricate links between viruses and developmental conditions.
Ethical Issues
While organoid research holds immense promise, ethical considerations surrounding consent regarding the use of human biomaterial and advances in cerebral organoid research become of greater concern. Stem cell research and informed consent have gone hand in hand since the infamous HeLa cell case, in which the cervical cancer cells of Henrietta Lacks taken during a biopsy were used without her or her family’s knowledge to create the first immortal human cell line for research [15]. Informed consent is critical to ensuring that individuals have the information necessary to decide whether to participate in a research study. Obtaining informed consent for use of biomaterials from individuals is a complicated process, involving providing participants with a complete understanding of potential uses of their donations and risks regarding the release of important or personal health information due to genetic match between organoids and tissue donors [10].
Consent is even more critical concerning individuals who have neurological and neurodegenerative disorders that impair their ability to give consent. Decisionally-sound adult stem cell donors can provide consent themselves when given a comprehensive explanation of their specific use, however, children and adults with brain disorders must rely on legal guardians for consent [10]. However, when studies use anonymously donated biomaterials from biobanks, informed consent becomes complicated. The International Society for Stem Cell Research guidelines for stem cell research require that informed consent be obtained close to the transfer of biomaterials to a research team [16]. The current standard is to obtain broad consent for unspecified uses of biomaterial, but this has been questioned by the scientific community, especially as scientific research with organoids becomes more commonplace and complex [17]. Proposed alternatives, such as retroactively requesting consent from donors or maintaining third-party contact with donors to convey overall research results, come with their own set of challenges. There is no current standard for identifying a method for reaching out to donors or returning research results, and the responsibility falls on individual labs and biobanks. Inconsistent practices across labs increase the possibility of insufficient consent and loss of donor anonymity [17].
Additionally, as organoids become more advanced, interest in the fusing of different brain regions together to better understand the complete model of the brain has increased. The question of organoids’ potential consciousness has sparked ethical dilemmas, stemming from two main concerns: the possibility of consciousness in organoids and the ethics surrounding the treatment of non-human animals that have organoid transplants [18]. Although there are still various barriers to achieving a significant level of consciousness with organoids to warrant serious concern, many researchers worry about the ethics of delaying philosophical debate.
Other Applications and Future Directions
Current advancements in organoid technology indicate a promising trajectory for precision medicine and personalized therapies for neurodevelopmental disorders. Integrating diverse organoid cultures has also enabled the modeling of complex neural processes, fostering a more comprehensive understanding of the human brain. These advancements are allowing researchers to explore new questions: to what extent can organoids show us how the brain changes as we get older or when it has mutations we can't predict? Researchers are increasingly exploring the potential of organoid models of multiple parts of the brain to mimic intricate interactions between different regions, providing a more complete view of brain function and pathology [19]. Although complex and needing further ethical consideration, the use of organoids offers a new and promising approach to neuroscience research.
References
1. Gooch, C. L., Pracht, E., & Borenstein, A. R. (2017). The burden of neurological disease in the United States: A summary report and call to action. Annals of neurology, 81(4), 479–484. https://doi.org/10.1002/ana.24897
2. Hulette C. M. (2003). Brain banking in the United States. Journal of neuropathology and experimental neurology, 62(7), 715–722. https://doi.org/10.1093/jnen/62.7.715
3. The Jackson Laboratory. (2023, January). January 2023- December 2023 Jax mice, Clinical and Research Services price list. The Jackson Laboratory. https://www.jax.org/pricelist
4. Kim, J., Koo, B. K., & Knoblich, J. A. (2020). Human organoids: model systems for human biology and medicine. Nature reviews. Molecular cell biology, 21(10), 571–584. https://doi.org/10.1038/s41580-020-0259-3
5. Mayhew, C. N., & Singhania, R. (2023). A review of protocols for brain organoids and applications for disease modeling. STAR protocols, 4(1), 101860. https://doi.org/10.1016/j.xpro.2022.101860
6. Watanabe, K., Kamiya, D., Nishiyama, A., Katayama, T., Nozaki, S., Kawasaki, H., Watanabe, Y., Mizuseki, K., & Sasai, Y. (2005). Directed differentiation of telencephalic precursors from embryonic stem cells. Nature neuroscience, 8(3), 288–296. https://doi.org/10.1038/nn1402
7. Lancaster, M. A., Renner, M., Martin, C. A., Wenzel, D., Bicknell, L. S., Hurles, M. E., Homfray, T., Penninger, J. M., Jackson, A. P., & Knoblich, J. A. (2013). Cerebral organoids model human brain development and microcephaly. Nature, 501(7467), 373–379. https://doi.org/10.1038/nature12517
8. Hebert, L. E., Weuve, J., Scherr, P. A., & Evans, D. A. (2013). Alzheimer disease in the United States (2010-2050) estimated using the 2010 census. Neurology, 80(19), 1778–1783. https://doi.org/10.1212/WNL.0b013e31828726f5
9. Raja, W. K., Mungenast, A. E., Lin, Y. T., Ko, T., Abdurrob, F., Seo, J., & Tsai, L. H. (2016). Self-Organizing 3D Human Neural Tissue Derived from Induced Pluripotent Stem Cells Recapitulate Alzheimer's Disease Phenotypes. PloS one, 11(9), e0161969. https://doi.org/10.1371/journal.pone.0161969
10. Hyun, I., Scharf-Deering, J. C., & Lunshof, J. E. (2020). Ethical issues related to brain organoid research. Brain research, 1732, 146653. https://doi.org/10.1016/j.brainres.2020.146653
11. Jawabri, K. H., & Sharma, S. (2023). Physiology, Cerebral Cortex Functions. In StatPearls. StatPearls Publishing.
12. U.S. National Library of Medicine. (n.d.). Miller-Dieker Syndrome: Medlineplus genetics. MedlinePlus. https://medlineplus.gov/genetics/condition/miller-dieker-syndrome/
13. Bershteyn, M., Nowakowski, T. J., Pollen, A. A., Di Lullo, E., Nene, A., Wynshaw-Boris, A., & Kriegstein, A. R. (2017). Human iPSC-Derived Cerebral Organoids Model Cellular Features of Lissencephaly and Reveal Prolonged Mitosis of Outer Radial Glia. Cell stem cell, 20(4), 435–449.e4. https://doi.org/10.1016/j.stem.2016.12.007
14. Gabriel, E., Ramani, A., Karow, U., Gottardo, M., Natarajan, K., Gooi, L. M., Goranci-Buzhala, G., Krut, O., Peters, F., Nikolic, M., Kuivanen, S., Korhonen, E., Smura, T., Vapalahti, O., Papantonis, A., Schmidt-Chanasit, J., Riparbelli, M., Callaini, G., Krönke, M., Utermöhlen, O., … Gopalakrishnan, J. (2017). Recent Zika Virus Isolates Induce Premature Differentiation of Neural Progenitors in Human Brain Organoids. Cell stem cell, 20(3), 397–406.e5. https://doi.org/10.1016/j.stem.2016.12.005
15. Lucey, B. P., Nelson-Rees, W. A., & Hutchins, G. M. (2009). Henrietta Lacks, HeLa cells, and cell culture contamination. Archives of pathology & laboratory medicine, 133(9), 1463–1467. https://doi.org/10.5858/133.9.1463
16. (2016). Guidelines for Stem Cell Science and Clinical Translation. International Society for Stem Cell Research. www.icssr.org.
17. MacDuffie, K. E., Stein, J. L., Doherty, D., Jayadev, S., Girault, J. B., Emmons, K. A., Glass, M. R., Dempsey, J. C., Marrus, N., Botteron, K. N., Dager, S. R., Estes, A. M., Piven, J., & Wilfond, B. S. (2023). Donor perspectives on informed consent and use of biospecimens for brain organoid research. Stem cell reports, 18(7), 1389–1393. https://doi.org/10.1016/j.stemcr.2023.05.019
18. Sawai, T., Sakaguchi, H., Thomas, E., Takahashi, J., & Fujita, M. (2019). The Ethics of Cerebral Organoid Research: Being Conscious of Consciousness. Stem cell reports, 13(3), 440–447. https://doi.org/10.1016/j.stemcr.2019.08.003
19. Bagley, J. A., Reumann, D., Bian, S., Lévi-Strauss, J., & Knoblich, J. A. (2017). Fused cerebral organoids model interactions between brain regions. Nature methods, 14(7), 743–751. https://doi.org/10.1038/nmeth.4304
