James, a 43 year old software developer, had chronic back pain for years. Despite seeing countless doctors, he never found lasting relief. After a particularly bad month, he decides to visit a local back pain specialist, Dr. Charlie Mutters. The physician suggests what he calls a “placebo pill,” an inert pill that can take advantage of the body’s natural painkilling. Intrigued, James takes Dr. Mutters up on the offer.
Placebos and Nocebos: What are they, and how do they work?
The term placebo comes from the Latin phrase “I shall please,” but today, it typically means a sham medical treatment. Despite being inactive, placebo treatments can still have significant beneficial effects on patients, known as the placebo effect. The most well known use for a placebo is in experiment design, where researchers give a placebo to a control group to confirm the treatment's efficacy [1].
But why does the placebo effect happen? Well, the placebo effect is largely a result of a patient’s expectation that a treatment will alleviate their illness. Many lines of evidence point to this belief being vital for the effect of a placebo. For one, patients who are told that they will be given a treatment respond better than those who are informed that the treatment is a placebo [1]. In addition, changes in how information is portrayed to the patient make substantial differences in not only how effective placebo medications are, but also how effective the active medication is [2].
On top of expectations, conditioning plays a large role in the placebo effect. Classical conditioning is a type of learning where an otherwise neutral stimulus becomes associated with an innate response and elicits that same response. For example, just as a cat may associate the sound of a food can with eating, a patient may associate the experience of ingesting a pill with pain relief. Although expectations and conditioning typically work together, these two mechanisms can independently cause the placebo effect [3]. Many everyday drugs become significantly more effective because we have been conditioned to expect them to work, thus improving treatment quality. Through both conditioning and expectations, otherwise inactive treatments are able to have large positive effects.
Sounds fantastic, but the placebo effect has an evil counterpart: the nocebo effect. Whereas the Latin term placebo means “I shall please,” the Latin term nocebo means “I shall harm.” Instead of bringing relief to the patient, the nocebo effect creates adverse side effects through the same mechanisms of expectation and conditioning [4]. In fact, the nocebo effect makes up a notable portion of all clinically reported adverse events. Often, a significant majority of side effects in clinical trials are actually a result of the patient's expectations of harm, or random events attributed to the treatment [4]. For example, in trials for the COVID-19 vaccine, over 70% of the side effects, such as fatigue, for the first dose and over 50% of side effects for the second dose were seen in the placebo group [5]. While the placebo response is able to consistently boost the efficacy of many medications, the nocebo effect frequently results in more perceived side effects — lowering the quality of the patients’ medical experience.

Mind Over Matter: Unveiling the Mechanisms of Placebo Pain Relief
Conditioning and expectations are the source of the placebo and nocebo effect, but how exactly do they cause a change in someone's perception of a medication? One well-studied type of placebo effect is the pain response, with much of our understanding of the neurological aspects of placebos coming from this subfield. Functional magnetic resonance imaging (fMRI), a tool used to measure activity of different regions of the brain, is effective in placebo analgesia research. By comparing the fMRI scans of people undergoing placebo pain relief and those who are not, researchers have spotted differences in the activity of many brain regions [6]. The researchers saw decreased activity of brain regions which have roles in decision making, pain processing, information relaying, and motor control. Those who responded more to placebo treatment saw larger decreases in the ventral attention and somatomotor networks, which work to detect new stimuli and coordinate motor movements, respectively. These networks are also activated during a painful stimulus, showing their role in processing and recognizing pain. Essentially, brain networks that serve important roles in feeling and shifting attention to pain are less active during a placebo response.
fMRI studies have also shown increases in activity in other brain regions during placebo pain relief, especially the dorsolateral prefrontal cortex, a key region involved in creating expectations and communicating those to the rest of the brain [6]. The placebo response is associated with an increase in the activity of the dorsolateral prefrontal cortex and the dorsal attention network, both of which are associated with focusing attention on external tasks [6]. In fact, using transcranial magnetic stimulation to disrupt activity in the dorsolateral prefrontal cortex results in an elimination of the placebo response [7]!
The dorsolateral prefrontal cortex seems to play a large role in conditioning and setting expectations, as well as modulating brain regions more directly involved in pain sensation, such as the periaqueductal gray. The degree of neural activity coupling — correlation of the activity of two brain regions — across the dorsolateral prefrontal cortex and the periaqueductal gray, may explain individual differences in placebo pain relief [8]. This link between the dorsolateral prefrontal cortex, a region of the brain generally involved in higher order tasks, with lower level pain processing, can show how an expectation can end up with changes in someone's perception of pain.
The pain system allows us to look beyond brain regions, as it is strongly and remarkably tied to compounds that act on a single neurotransmitter receptor: the opioid receptor. Some drugs which act on opioid receptors that you have likely heard of are fentanyl, heroin, and oxycontin, but what is less known is that the human body naturally produces similar molecules [9]. These so-called endogenous opioids are released in some of the same regions known to be involved in placebo pain relief, including the periaqueductal gray. The effect of these endogenous opioids is very similar to that of outside ones, so the same drug that blocks overdoses, naloxone, more commonly known as narcan, can actually block the placebo effect in people! This placebo blocking occurs even if the patient isn’t aware that they have received naloxone [6][9]. In short, placebo pain relief relies on the patient’s opioid receptors’ capacity to accept endogenous opioids.
Beyond Illusion: Other Examples of Placebos
While much of this research is looking at placebo analgesia, many of these same regions and molecules appear to be involved in other placebo responses.
Placebos can affect other body systems because of the endogenous opioid release, which includes some inflammatory cytokines, a type of secreted protein that induces the immune response. Endogenous opioids bind with and regulate the concentration of Interleukin 18 (IL-18), a pro-inflammatory cytokine that triggers the inflammatory immune response, explaining how the placebo effect is able to reduce inflammation [10].
Another instance of the placebo effect in action is its effects on hunger. In one study two groups were given water, and instructed that it would either be filling or unfilling. The high satiety group reported being made more full by the water, and the activity in the dorsolateral prefrontal cortex, the same attention control and expectation-setting region as before, seems to explain placebo-related hunger differences in these groups [11]. Placebo effects can also increase the presence of the hunger causing hormone ghrelin, although the effects are relatively modest [12]. The fact that the brain has a significant and direct physiological effect on hunger should not be a surprise: we all know how it feels to get hungry because you thought about something tasty, or to lose your appetite because you imagined something disgusting. The brain can expect to become hungry and subsequently increase the relevant hunger hormone ghrelin to prepare for eating, or expect satiety and decrease hunger signaling in the brain.
Placebo Modulation: What Impacts the Size of a Placebo Effect?
Because the placebo effect is dependent on the patient’s expectations, it stands to reason that stronger expectations would elicit stronger placebo responses — and that seems to be the case! Optimists who are more prone to positive beliefs about a treatment’s efficacy tend to experience more of the placebo effect, whereas pessimists often experience more of the nocebo effect [13][14].
Not only can a patient’s mindset influence the size of a placebo response, but so can a multitude of factors related to the medication itself. Despite identical active ingredients, patients report greater pain relief from drugs marketed as more expensive. These findings suggest that people, reasonably or not, associate higher priced treatments with higher values [15]. Taking more pills per day can also increase the magnitude of the placebo effect, likely because people view a high frequency intervention to be more effective, even if the intervention is sugar pills [16]. Because more extreme and seemingly convincing treatments seem to have larger effects, it is questioned if more invasive procedures would as well. While some studies show this to be the case, various systematic reviews on this topic find no consistent difference between more and less invasive treatment methods, so if any differences exist, the benefit likely doesn’t outweigh the cost [17][18].
Placebo effects pose a great challenge to researchers, as it becomes more difficult to discern the efficacy of a given treatment. The existence of the placebo effect is a major factor driving the need for control groups in clinical trials to determine the actual connections between the medical treatments and patient outcomes. On the other hand, the nocebo effect can cause active harm to patients, which is the last thing any doctor would want, even as a result of their patient’s own expectations. The medical field is aware of the role of both the placebo and nocebo effects in treatment, and it is an expert consensus that health professionals should try to maximize placebo effects and minimize nocebo effects [19]. How information is portrayed to patients, as well as how clinicians communicate empathetically with patients, can change how likely the patient is to believe that the treatment will be safe and effective.
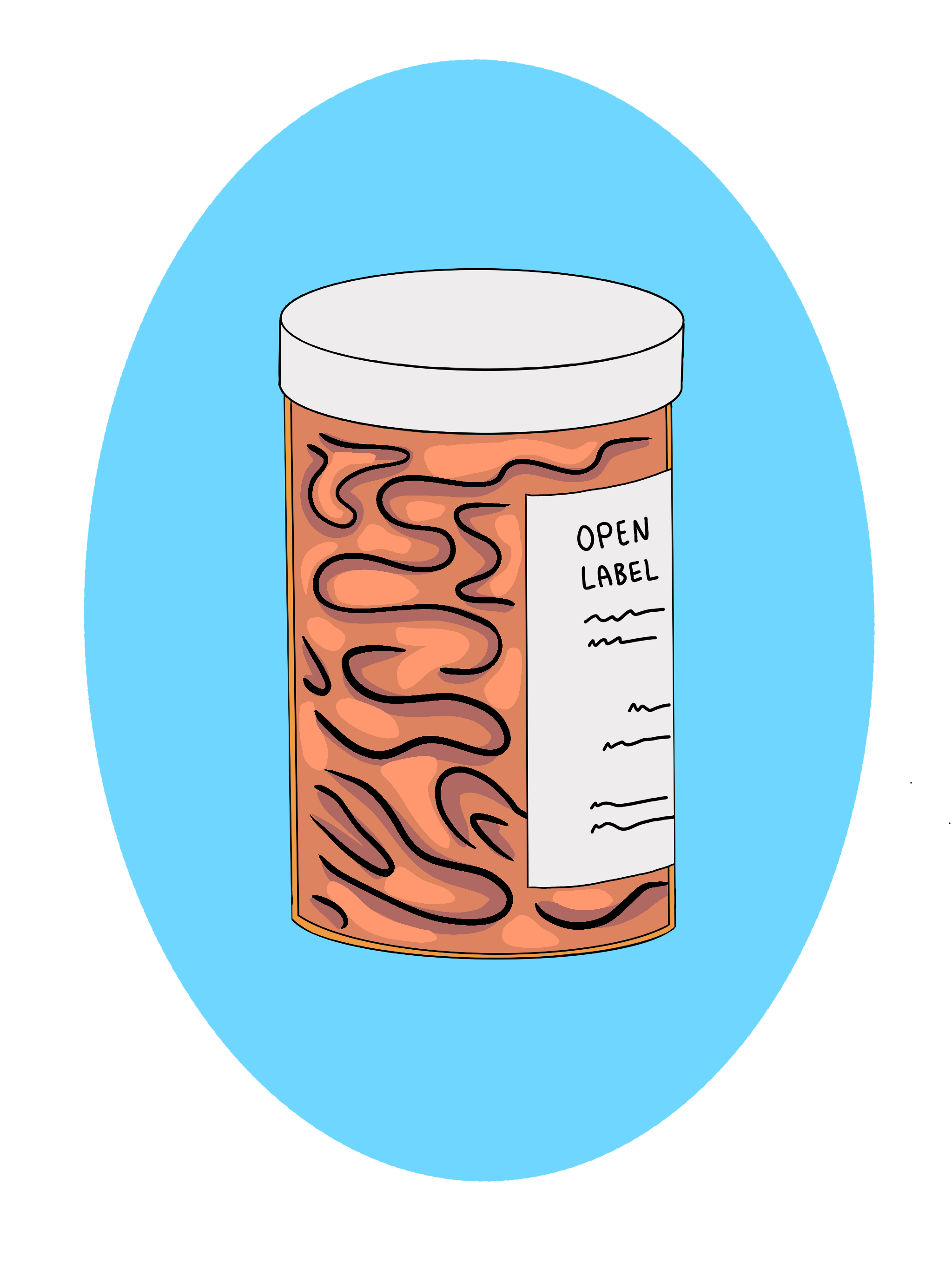
Breaking the Blinding: The Open-Label-Placebo
Remember James? His doctor gave him a placebo and told him exactly what it was! James was given an open-label-placebo, a relatively new treatment where the patient is told that they will be taking a placebo pill and instructed to take the medication regardless. Doctors emphasize the power of the placebo effect to patients, informing them about conditioning, and how the placebo effect can be powerful [20][21]. While it may sound absurd that doctors would give a patient a fake treatment, it is a useful option for conditions with poor treatments. Standard medical treatments can be detrimental for a number of reasons. For chronic lower back pain, the consistent and heavy use of opioids can result in addiction, and the other treatments we use have been shown to be less effective than an open placebo [21]. Open-label-placebos have been studied in many conditions, including irritable bowel syndrome, cancer-related fatigue, and depression, and have often been shown to produce postive effects [22]. In fact, one study found that open-label-placebos were as effective as double-blind placebos for the treatment of irritable bowel syndrome, suggesting that some patient populations may not have a more effective treatment if they used deceptive placebos [23]. That said, when diseases have objective biomarkers such as blood pressure, instead of being up to self-report such as conditions like pain or depression, open-label-placebos are no more effective than the absence of treatment [22]. Although open-label-placebos have limitations, they may be an effective treatment for many of medicine’s common self-report-based conditions.
Of course, lying to patients and administering a placebo under the guise of real treatment is another option. In fact, it can be surprisingly common, with one study finding a majority of doctors prescribing hidden placebos [24]. Many of the doctors in that same study reported that they expected at least some patients would be disappointed to learn they had received a placebo [24]. Nonetheless, the ethics of a doctor lying to their patient about the administration of placebos are controversial, with many frowning upon the use of deception in treatment [19]. Lack of deception has been touted by open-label-placebo advocates as one of the benefits of that method, weighing the greater integrity higher than any possible benefit born from deception [19].
The Placebo Revolution: Unblurring the Lines
While James' back pain may not be cured by an open-label-placebo, he is a fascinating example of the changing landscape of placebo research. In recent years, researchers have gained a better understanding of the neurological basis of the placebo effect, including relevant brain regions. Additionally, scientists have learned more about the placebo effect’s impact on neurotransmitters and hormones, providing insight into the mechanism of the placebo response. The scientific community is working to improve understanding of the factors that modify the placebo effect and increase expert consensus on how to best harness it for standard treatment. Most interesting of all is the development and increasing utilization of the open-label-placebo, which may be able to give James the treatment he so desperately needs.
References
- Gerdesmeyer, L., Klueter, T., Rahlfs, V. W., Muderis, M. A., Saxena, A., Gollwitzer, H., Harrasser, N., Stukenberg, M., & Prehn-Kristensen, A. (2017). Randomized Placebo-Controlled Placebo Trial to Determine the Placebo Effect Size. Pain physician, 20(5), 387–396.
- Kam-Hansen, S., Jakubowski, M., Kelley, J. M., Kirsch, I., Hoaglin, D. C., Kaptchuk, T. J., & Burstein, R. (2014). Altered placebo and drug labeling changes the outcome of episodic migraine attacks. Science Translational Medicine, 6(218). https://doi.org/10.1126/scitranslmed.3006175
- Bąbel, P. (2019). Classical conditioning as a distinct mechanism of placebo effects. Frontiers in Psychiatry, 10. https://doi.org/10.3389/fpsyt.2019.00449
- Mahr, A., Golmard, C., Pham, E., Iordache, L., Deville, L., & Faure, P. (2017). Types, frequencies, and burden of nonspecific adverse events of drugs: Analysis of randomized placebo‐controlled clinical trials. Pharmacoepidemiology and Drug Safety, 26(7), 731–741. https://doi.org/10.1002/pds.4169
- Haas, J. W., Bender, F. L., Ballou, S., Kelley, J. M., Wilhelm, M., Miller, F. G., Rief, W., & Kaptchuk, T. J. (2022). Frequency of adverse events in the placebo arms of COVID-19 Vaccine Trials. JAMA Network Open, 5(1). https://doi.org/10.1001/jamanetworkopen.2021.43955
- Zunhammer, M., Spisák, T., Wager, T. D., Bingel, U., Atlas, L., Benedetti, F., Büchel, C., Choi, J. C., Colloca, L., Duzzi, D., Eippert, F., Ellingsen, D.-M., Elsenbruch, S., Geuter, S., Kaptchuk, T. J., Kessner, S. S., Kirsch, I., Kong, J., Lamm, C., … Zeidan, F. (2021). Meta-analysis of neural systems underlying placebo analgesia from individual participant fmri data. Nature Communications, 12(1). https://doi.org/10.1038/s41467-021-21179-3
- Krummenacher, P., Candia, V., Folkers, G., Schedlowski, M., & Schönbächler, G. (2010). Prefrontal cortex modulates placebo analgesia. Pain, 148(3), 368–374. https://doi.org/10.1016/j.pain.2009.09.033
- Crawford, L. S., Mills, E. P., Peek, A., Macefield, V. G., Keay, K. A., & Henderson, L. A. (2023). Function and biochemistry of the dorsolateral prefrontal cortex during placebo analgesia: How the certainty of prior experiences shapes endogenous pain relief. Cerebral Cortex, 33(17), 9822–9834. https://doi.org/10.1093/cercor/bhad247
- Sauro, M. D., & Greenberg, R. P. (2005). Endogenous opiates and the placebo effect. Journal of Psychosomatic Research, 58(2), 115–120. https://doi.org/10.1016/j.jpsychores.2004.07.001
- Prossin, A., Koch, A., Campbell, P., Laumet, G., Stohler, C. S., Dantzer, R., & Zubieta, J.-K. (2021). Effects of placebo administration on immune mechanisms and relationships with central endogenous opioid neurotransmission. Molecular Psychiatry, 27(2), 831–839. https://doi.org/10.1038/s41380-021-01365-x
- Khalid, I., Rodrigues, B., Dreyfus, H., Frileux, S., Meissner, K., Fossati, P., Hare, T. A., & Schmidt, L. (2024). Mapping expectancy-based appetitive placebo effects onto the brain in women. Nature Communications, 15(1). https://doi.org/10.1038/s41467-023-44569-1
- Hoffmann, V., Lanz, M., Mackert, J., Müller, T., Tschöp, M., & Meissner, K. (2018). Effects of placebo interventions on subjective and objective markers of appetite–a randomized controlled trial. Frontiers in Psychiatry, 9. https://doi.org/10.3389/fpsyt.2018.00706
- Geers, A., Helfer, S., Kosbab, K., Weiland, P., & Landry, S. (2005). Reconsidering the role of personality in placebo effects: Dispositional optimism, situational expectations, and the placebo response. Journal of psychosomatic research. https://pubmed.ncbi.nlm.nih.gov/15820839/
- Morton, D. L., Watson, A., El-Deredy, W., & Jones, A. K. P. (2009). Reproducibility of placebo analgesia: Effect of dispositional optimism. Pain, 146(1), 194–198. https://doi.org/10.1016/j.pain.2009.07.026
- Espay, A. J., Norris, M. M., Eliassen, J. C., Dwivedi, A., Smith, M. S., Banks, C., Allendorfer, J. B., Lang, A. E., Fleck, D. E., Linke, M. J., & Szaflarski, J. P. (2015). Placebo effect of medication cost in parkinson disease. Neurology, 84(8), 794–802. https://doi.org/10.1212/wnl.0000000000001282
- De Craen, A. J., Moerman, D. E., Heisterkamp, S. H., Tytgat, G. N., Tijssen, J. G., & Kleijnen, J. (1999). Placebo effect in the treatment of duodenal ulcer. British Journal of Clinical Pharmacology, 48(6), 853–860. https://doi.org/10.1046/j.1365-2125.1999.00094.x
- de Craen, A. J., Tijssen, J. G., de Gans, J., & Kleijnen, J. (2000). Placebo effect in the acute treatment of migraine: Subcutaneous placebos are better than oral placebos. Journal of Neurology, 247(3), 183–188. https://doi.org/10.1007/s004150050560
- Fässler, M., Meissner, K., Kleijnen, J., Hróbjartsson, A., & Linde, K. (2015). A systematic review found no consistent difference in effect between more and less intensive placebo interventions. Journal of Clinical Epidemiology, 68(4), 442–451. https://doi.org/10.1016/j.jclinepi.2014.11.018
- Evers, A. W. M., Colloca, L., Blease, C., Annoni, M., Atlas, L. Y., Benedetti, F., Bingel, U., Büchel, C., Carvalho, C., Colagiuri, B., Crum, A. J., Enck, P., Gaab, J., Geers, A. L., Howick, J., Jensen, K. B., Kirsch, I., Meissner, K., Napadow, V., … Kelley, J. M. (2018). Implications of placebo and nocebo effects for clinical practice: Expert consensus. Psychotherapy and Psychosomatics, 87(4), 204–210. https://doi.org/10.1159/000490354
- Von Wernsdorff, M., Loef, M., Tuschen-Caffier, B., & Schmidt, S. (2021).Effects of open-label Placebos in clinical trials:A systematic review and meta-analysis. Scientific Reports, 11(1). https://doi.org/10.1038/s41598-021-83148-6
- Carvalho, C., Caetano, J. M., Cunha, L., Rebouta, P., Kaptchuk, T. J., & Kirsch, I. (2016). Open-label placebo treatment in chronic low back pain: A randomized controlled trial. Pain, 157(12), 2766–2772. https://doi.org/10.1097/j.pain.0000000000000700
- Spille, L., Fendel, J. C., Seuling, P. D., Göritz, A. S., & Schmidt, S. (2023). Open-label Placebos—a systematic review and meta-analysis of experimental studies with non-clinical samples. Scientific Reports, 13(1). https://doi.org/10.1038/s41598-023-30362-z
- Lembo, A., Kelley, J. M., Nee, J., Ballou, S., Iturrino, J., Cheng, V., Rangan, V., Katon, J., Hirsch, W., Kirsch, I., Hall, K., Davis, R. B., & Kaptchuk, T. J. (2021). Open-label placebo vs double-blind placebo for irritable bowel syndrome: A randomized clinical trial. Pain, 162(9), 2428–2435. https://doi.org/10.1097/j.pain.0000000000002234
- Agarwal, R., Aujla, R., Sinha, S., & Kumar, A. (2020). Perception and practice of placebo use among physicians in Mangalore. Journal of Family Medicine and Primary Care, 9(3), 1424. https://doi.org/10.4103/jfmpc.jfmpc_1052_19