A person can walk around experiencing seizures for months without realizing it. In my dad’s case, his seizures manifested as odd smells, bouts of fear, intense anxiety, all of which came and went within seconds. Even as these symptoms worsened, he took them in stride, and his life carried on without anyone noticing that there was something urgently wrong with him. But one day, my dad had a seizure that lasted for several minutes, and he was rushed to the ER. If someone experiencing these odd symptoms brushes them aside like my father did, they could risk ignoring what is often the first symptom of a much deadlier disease: brain cancer.
Brain Tumors can Cause Epilepsy
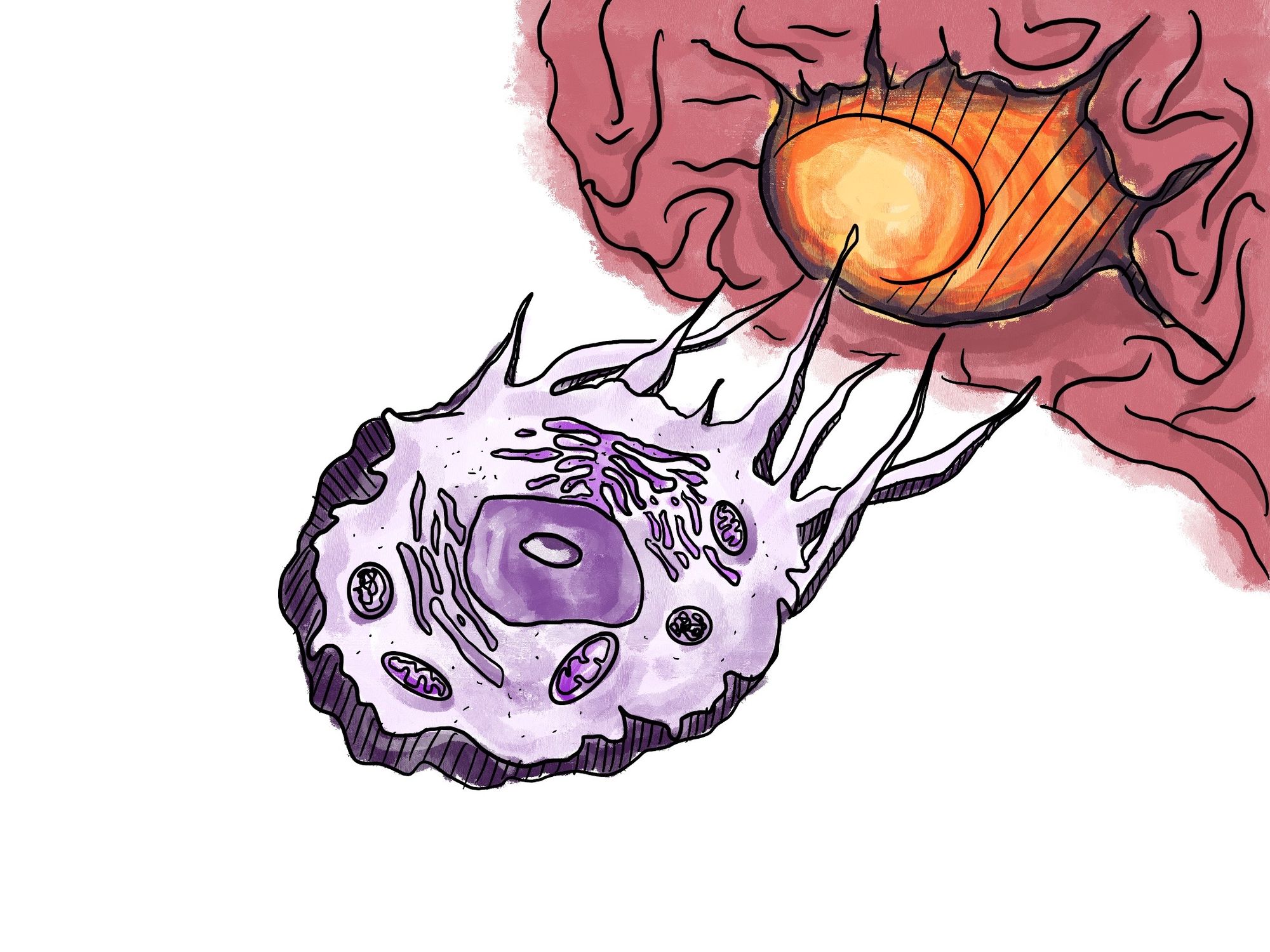
The neocortex is the part of the brain associated with higher thinking and is responsible for human consciousness and cognition. Any kind of brain tumor located in the neocortex has the potential to cause many seizures over a period of time [1]. In other words, brain tumors can cause epilepsy. Epilepsy is a very broad term for a disease that is widely misunderstood, but it is applicable to any person who has had two or more unprovoked seizures in a relatively short amount of time. Seizures are caused by abnormal electrical activity in the brain’s neural network and are broadly classified into two categories: general and focal seizures [2].

Generalized seizures originate from both sides of the brain, and therefore affect both sides of the body [2]. This type of seizure often involves the involuntary jerking movements that many people associate with epilepsy. Focal seizures, on the other hand, are localized to one side of the brain. These can stay localized and have different symptoms, ranging from emotional or cognitive to behavioral arrest, where the afflicted patient simply freezes up. These seizures often also present with varying levels of awareness on the patient's end. In the case that a focal seizure spreads to both sides of the brain, it will become generalized and may involve loss of some motor control as well [2].
Focal seizures are more common than generalized seizures but are often underreported or simply misrecognized [2]. Each patient can have a unique combination of symptoms, which makes the diagnosis more difficult. In patients with brain cancer, various side effects based on the brain tumor’s location can also complicate diagnosis and symptoms of seizures. For example, my father’s tumor was located on the left side of his brain, near the areas that control language. Because of this, he would have difficulty communicating and speaking clearly in both English and Vietnamese, and it was often unclear if that was due to a seizure or due to the tumor invading areas of the brain responsible for speaking. In general, common side effects of brain tumors include headaches, fatigue, and side effects such as imbalance or vision problems depending on what parts of the brain are affected [2].
Many brain tumors occur as a result of a glioma, which is a cluster of cancerous cells that originate and grow from the brain or the spinal cord [3]. Primary tumors start in the brain, while secondary tumors metastasize, or spread, to the brain from other cancers. Brain tumors are classified from Grades 1 to 4, where Grades 1 and 2 represent benign tumors that grow slowly, and Grades 3 and 4 represent malignant tumors that grow aggressively [4]. Some types of brain tumors progress in grade and spread more rapidly, but others may only start and stay at a certain grade. It is extremely rare for multiple types of brain tumors to affect one patient [5]. Although brain tumor-related seizures are common in both children and adults, there are some differences in the types of cancer, and therefore there are differences in the occurrence of seizures that tend to affect either demographic [6]. Children tend to be diagnosed with low-grade gliomas, which often have a high incidence of seizures, with anywhere from 75-99% of patients having epilepsy depending on the type of cancer [7]. In comparison, high-grade brain tumors tend to occur in adults. The most common high-grade tumor is glioblastoma, which only causes epilepsy in around 29-60% of patients [6]. Seizures are nonetheless very common as a presenting symptom of brain cancer, which means that the symptoms they cause are one of the first signs that drive patients to seek a diagnosis from their doctor.
The overall survival rate of patients with brain tumor-related epilepsy is not necessarily affected if the patients have seizures as the first symptom of their brain tumor or if seizures begin after the initial diagnosis [8]. However, if focal seizures are the first presenting symptom of a brain tumor, doctors may be able to treat the brain tumor itself earlier. In the case that a patient’s symptoms are not fully understood, this may lead to several complications in the treatment process. When my father was first seeking treatment, his physician did not link his seizures to brain cancer, which led to a misdiagnosis and lost him precious time before he was able to receive treatment for his tumor.
Altered Brain Signaling
In order to understand how and why brain tumor-related epilepsy presents such a unique challenge to diagnose and control, it is important to understand the biology that connects seizures and brain tumors.
Brain signals often end with the release of neurotransmitters such as serotonin and dopamine, which send communicative signals between the brain and body. The two neurotransmitters that are most involved in epilepsy are glutamate and GABA, which help increase and decrease signaling respectively.
Recently, researchers have linked a transporter for an amino acid called glutamate, named SLC7A11, to glioma seizures and tumor growth [9]. Brain tumors grow so quickly partly because the tumor itself causes glutamate release beyond normal levels. In a normal brain, glutamate generally helps the body function by acting as an excitatory neurotransmitter. These neurotransmitters help fire neurons, but in excess, glutamate can lead to seizures, as well as cell death. When a brain tumor mediates the release of glutamate, the level of this neurotransmitter becomes toxic, causing healthy tissue around the tumor to die and allowing the tissue of the brain tumor to expand into the newly vacant space. This means that if SLC7A11’s gene expression is increased, it may function as a predictor for accelerated tumor growth, as well as seizures [9].
The other neurotransmitter related to glioma-related epilepsy is GABA, which is the primary inhibitory neurotransmitter in the brain. Its function is the opposite of glutamate, as it serves to turn neuron activity off. When gliomas are nearby, GABA ceases to function normally and starts to turn neuron activity on instead [10]. A recent study done on rats with gliomas found that the density of neurons that act as GABA receptors is greatly decreased in the peritumoral region, which is the tissue that surrounds the tumor [11]. Because of this, the hyperactivity in the brain that is characteristic in patients with seizures may be due to a lack of GABA, which normally calms down electrical activity.
Presently, scientists are investigating whether the tumor itself causes changes in the peritumoral area of the brain. This theory is constantly evolving, as this field of study is still relatively new. One of the studies that supports this theory investigated the pathways involved in glioma-related seizures and collected peritumoral tissues obtained from surgeries in order to use them for RNA sequencing [12]. This technique is a tool that allows scientists to observe gene expression in a sample by noting the presence and number of different RNA molecules [13]. The researchers in this study discovered differentially expressed genes in patients with brain tumors and seizures, which suggested that altered signaling of glutamate is a potential cause of peritumoral epilepsy [12]. Increased glutamate signaling may drive the brain into overexcitability, which can cause seizures.
Another factor that may promote seizures in brain tumor patients is the disruption of action potentials. To send a signal, a neuron fires an action potential, which is created by a difference in ion concentrations in the neuron. In order to keep signals firing at normal rates, homeostasis in these ions must be maintained. As such, disruption of calcium ion homeostasis is one potential cause of peritumoral epilepsy. Another example that was found recently in mouse studies pinpoints the gene IGSF3 as one that mediates tumor growth by altering potassium ion homeostasis [12] [14].
A different approach to understanding why brain tumors may cause seizures is to look at how the glioma itself spreads. A type of molecule in the brain that controls how neurons spread and then differentiate is called neurotrophic factor, which scientists have recently pinpointed as a possible component that may drive glioma progression. In particular, the neurotrophic factor BDNF, which promotes plasticity in synapse function in a regular brain, may in a brain tumor augment its progression by helping new synapses form between regular neurons and tumor neurons [15]. The new signaling pathways made between healthy and unhealthy brain cells might drive epileptic activity and thus cause seizures.
All of the studies discussed above highlight important pathways involved in brain tumor-related epilepsy, which also identify new mechanisms for medications that aim to decrease the severity of seizures in brain cancer patients. There is also evidence that points towards neuroinflammation as a factor that ties together epilepsy and brain tumors. The tumor microenvironment (TME) is a key area within the peritumoral region regarding the incidence of seizures. Understanding the composition of the different immune cells within the TME across brains with epilepsy, metastases, and primary brain tumors reveals key insights into the relationship between brain cancer and seizures. In particular, the TME of brains contains different types of macrophages, which are immune cells that eliminate unhealthy cells. In recent research, scientists found that the composition of these immune cells in a glioma’s TME was similar to that of an epileptic brain’s TME [16]. The immune link between the two diseases expands our current understanding of brain dysfunction and may provide some insight into why brain cancer occurs at all.
Treatments for Seizures
As our knowledge of irregular signaling and glioma growth increases, the current repertoire of treatments available to treat brain cancer, and specifically brain-tumor-related epilepsy, also continues to grow. The normal courses of treatment for cancer are radiation therapy, chemotherapy, and surgery [6]. For brain cancers in particular, neurosurgery is normally the very first step taken. Patients may have the option to undergo a biopsy during which a small piece of tissue of the tumor is removed in order to identify what the tumor is, or a full removal of as much cancerous tissue as the surgeon deems safe. Generally, it is inadvisable to undergo more than one brain surgery, as the patient will likely be too weak to attempt the procedure a second time, especially if other treatments are ongoing at the same time. In my father’s case, a biopsy was preferred because his tumor was located near the areas of the brain that controlled language. Removing too much of the tissue in the surrounding area could have caused him to lose his ability to communicate at all. In other patients, removing as much of the tumor as possible is preferred, especially if it is smaller and thus would disturb fewer existing connections. By nature, reducing the size of a tumor makes it so that the surrounding healthy cells are no longer crowded by cancerous cells. With the activity of healthy neurons no longer impacted by TME, this type of treatment often manages to naturally decrease the incidence of seizures. In some cases, neurosurgery may be specifically performed to control seizures rather than reduce the volume of a tumor, especially in cases where the tumor is benign. This type of surgery focuses on cutting out as much of the tumor as possible while also targeting the areas around the tumor that induce the most seizures [6].
It is vital to treat seizures in order to improve the quality of life for patients who have brain tumor related epilepsy. Although there are presently no known cures for either brain cancer or epilepsy, the severity of symptoms can be controlled. The most common type of approach to treating seizures is to prescribe patients antiseizure medications, which reduce the frequency and intensity of seizures. They tend to target the various pathways involved in overexcitability and neuron signaling in the brain with different mechanisms that can target voltage-gated sodium, calcium, or potassium ion channels [17]. Several other antiseizure medications also target the release of excitatory or inhibitory neurotransmitters directly.
In general, only one type of antiseizure drug is prescribed to patients, to minimize the different side effects that may occur. One of the most common antiseizure drugs prescribed to patients is Levetiracetam, while the drugs Pregabalin and Temozolomide are used less often. Levetiracetam and Pregabalin are both relatively new drugs, having been approved for medical use in the last thirty years, but they are promising as monotherapies for treating seizures that arise as a result of gliomas. Both drugs are non-enzyme-inducing, which means that they do not encourage the synthesis of enzymes. Antiepileptic drugs that induce enzymes reduce the ability of many other drugs to function properly, which can cause various other comorbidities in patients [18]. Therefore, Levetiracetam and Pregabalin offer patients a better course of treatment because they do not have this unintended effect.
When these drugs were first going through their clinical trials for patients with high-grade gliomas, Levetiracetam and Pregabalin were successful in helping the majority of the surviving patients to remain seizure-free after a 1-year follow-up. The retention rate, or the overall effectiveness of the medication, after a year of each of the drugs in patients with gliomas was similar to patients with epilepsy but no brain tumors: 70% for Levetiracetam, and 50% for Pregabalin [19]. This was crucial because Phenytoin, which was often prescribed to brain tumor patients before the development of Levetiracetam, has since been replaced because it had the common side effect of decreasing cognitive abilities like attention span and memory [20] [21].
Treatments other than anti-seizure medications may also be able to decrease the frequency of seizures in patients with brain tumors. In some primary brain cancer patients, chemotherapy has been shown to help reduce seizures as a side effect [22]. The most prominent example of this is the use of the chemotherapy drug Temozolomide, which has been used in some studies done on glioma patients. In a clinical trial of elderly glioblastoma patients, patients who were prescribed Temozolomide in addition to receiving radiation therapy tended to have a later onset for seizures as well as longer overall survival rates [22].
New pathways have also been discovered that increase our understanding of brain tumors and allow the development of potential new medicines with different mechanisms. For example, protein kinases, which help to catalyze reactions through modifying other proteins, may be connected to glioma progression and seizures. Scientists recently discovered that a specific protein kinase called mTOR promotes seizures when it is hyperactive [23]. Their study on tumor-bearing mice with recurring behavioral seizures showed an effective response to the drug AZD, an inhibitor of the mTOR kinase, which reduced its activity. Mice that had seizures in the 12 hours before drug administration did not display any epileptic activity in the 12 hours after drug administration [23]. This medication may be able to decrease overexcitability in the brain connected to seizures, as well as glioma progression itself. Many other mechanisms are continuously being studied and developed to improve the well-being of patients.
Attempting to target brain cancer and brain tumor-related seizures from multiple angles is the most common approach that doctors and scientists take. This method is most likely to increase the quality of life for patients living with the disease and involves a constantly improving repertoire.
Quality of Life
Patients who suffer from the symptoms of brain tumor-related epilepsy as well as the tumor itself face a host of difficulties. Both focal seizures and generalized seizures are dangerous. If left uncontrolled, patients who continue to experience these seizures have a mortality risk about 40 times as high as patients whose seizures are controlled or in remission. Sudden unexpected death can occur in patients with brain tumor-related epilepsy, alongside a higher chance of accidental injuries, which can arise from lapses in attention or as a result of involuntary movements [24].
These symptoms are only part of the consequences that patients with brain-tumor-related epilepsy experience because of their disease. The high risks of having a seizure in combination with the unique communication, attention, motor control, and various other issues due to an individual’s brain cancer mean that many patients are no longer able to drive without risking an accident. They may no longer be able to work due to decreased competency in previously routine tasks. Many may face their disease without social support, as well as stigmatization, as many people do not know about or understand the various symptoms and causes of epilepsy. Because this condition is chronic, the mental and financial burden on patients, their families, and caregivers is similarly long-lasting and can often continue well after the afflicted patient has passed [24].
Moreover, many of the treatments previously discussed are not foolproof—in fact, attempting to treat symptoms may actually lead to more seizures or serious side effects. Patients routinely experience seizures after brain surgery and can sometimes even develop seizures without prior history of epileptic activity. Additionally, the drugs used to treat seizures come with the common side effects of dizziness, depression, and concentration problems. Side effects are different from patient to patient, but it is normal to witness someone change into a completely different person throughout the course of their treatment. My family was lucky that my dad responded relatively well to chemotherapy and radiation therapy. He experienced fatigue, some dizziness, and lost weight, but was not completely bedridden and did not go through intense pain or vomiting episodes like other patients.
Though brain cancer patients each have their own ways of facing their illnesses, it is common for them to lash out, self-isolate, and lose motivation for simple activities. In the face of such an overwhelming disease, the best course of action is to treat as many symptoms as possible and to provide emotional and social support for the afflicted and their family as they go through the most difficult time of their lives. My father was blessed with an abundance of aunts, uncles, and cousins in addition to his immediate family—we believe throughout his sickness he retained much of his liveliness and personality due to having a constant presence of love in his life.
Conclusion
Though it may at times seem futile for patients to pursue treatment for brain cancer and seizures—especially because the diagnosis for brain tumors is often terminal—treatment can still offer patients an avenue to live the rest of their lives as fully as possible. In cases such as my own, pursuing treatment was invaluable not just for the time I was able to gain with my father, but also for the fact that my family has grown much closer than before.
Effectively treating the seizures associated with brain tumors is one of the ways doctors can prolong the life expectancy and health outcomes of patients. For patients that have metastases or high-grade gliomas, seizures are treated until the patient passes away. For children who are diagnosed with a low-grade glioma, the chances of surviving into adulthood are quite high. However, around half of survivors still suffer from seizures more than five years after their initial diagnosis [25]. Even though this condition is so common and able to last for years on end, not many people know of it.
Further research investigating the cause of seizures is needed in order to increase awareness and understanding of the relationship between epilepsy and brain tumors. This will encourage better detection and diagnosis of brain tumors. New drug discoveries will make antiseizure medications more effective for those who need them, while innovative therapies will lower the overall toxicity of current treatments, allowing patients to live more comfortably. Every new research paper and every new treatment allows us to better treat every new patient. And every new discovery leads us closer to a cure for cancer.
References
- Fisher, R. S., Acevedo, C., Arzimanoglou, A., Bogacz, A., Cross, J. H., Elger, C. E., Engel, J., Jr, Forsgren, L., French, J. A., Glynn, M., Hesdorffer, D. C., Lee, B. I., Mathern, G. W., Moshé, S. L., Perucca, E., Scheffer, I. E., Tomson, T., Watanabe, M., & Wiebe, S. (2014). ILAE official report: a practical clinical definition of epilepsy. Epilepsia, 55(4), 475–482. https://doi.org/10.1111/epi.12550
- Beghi, E. (2020). The Epidemiology of Epilepsy. Neuroepidemiology, 54(2), 185–191. https://doi.org/10.1159/000503831
- Mesfin, F. B., & Al-Dhahir, M. A. (2023). Gliomas. In StatPearls. StatPearls Publishing
- Torp, S. H., Solheim, O., & Skjulsvik, A. J. (2022). The WHO 2021 Classification of Central Nervous System tumours: a practical update on what neurosurgeons need to know-a minireview. Acta neurochirurgica, 164(9), 2453–2464. https://doi.org/10.1007/s00701-022-05301-y
- Tunthanathip, T., Kanjanapradit, K., Ratanalert, S., Phuenpathom, N., Oearsakul, T., & Kaewborisutsakul, A. (2018). Multiple, Primary Brain Tumors with Diverse Origins and Different Localizations: Case Series and Review of the Literature. Journal of neurosciences in rural practice, 9(4), 593–607. https://doi.org/10.4103/jnrp.jnrp_82_18
- Gonzalez Castro, L. N., & Milligan, T. A. (2020). Seizures in patients with cancer. Cancer, 126(7), 1379–1389. https://doi.org/10.1002/cncr.32708
- Slegers, R. J., & Blumcke, I. (2020). Low-grade developmental and epilepsy associated brain tumors: a critical update 2020. Acta neuropathologica communications, 8(1), 27. https://doi.org/10.1186/s40478-020-00904-x
- Knudsen-Baas, K. M., Storstein, A. M., Zarabla, A., Maialetti, A., Giannarelli, D., Beghi, E., & Maschio, M. (2021). Antiseizure medication in patients with Glioblastoma- a collaborative cohort study. Seizure, 87, 107–113. https://doi.org/10.1016/j.seizure.2021.03.012
- Robert, S. M., Buckingham, S. C., Campbell, S. L., Robel, S., Holt, K. T., Ogunrinu-Babarinde, T., Warren, P. P., White, D. M., Reid, M. A., Eschbacher, J. M., Berens, M. E., Lahti, A. C., Nabors, L. B., & Sontheimer, H. (2015). SLC7A11 expression is associated with seizures and predicts poor survival in patients with malignant glioma. Science translational medicine, 7(289), 289ra86. https://doi.org/10.1126/scitranslmed.aaa8103
- Pallud, J., Le Van Quyen, M., Bielle, F., Pellegrino, C., Varlet, P., Cresto, N., Baulac, M., Duyckaerts, C., Kourdougli, N., Chazal, G., Devaux, B., Rivera, C., Miles, R., Capelle, L., & Huberfeld, G. (2014). Cortical GABAergic excitation contributes to epileptic activities around human glioma. Science translational medicine, 6(244), 244ra89. https://doi.org/10.1126/scitranslmed.3008065
- Komiyama, K., Iijima, K., Kawabata-Iwakawa, R., Fujihara, K., Kakizaki, T., Yanagawa, Y., Yoshimoto, Y., & Miyata, S. (2022). Glioma facilitates the epileptic and tumor-suppressive gene expressions in the surrounding region. Scientific reports, 12(1), 6805. https://doi.org/10.1038/s41598-022-10753-4
- Kumar, K., Dubey, V., Zaidi, S. S., Tripathi, M., Siraj, F., Sharma, M. C., Chandra, P. S., Doddamani, R., Dixit, A. B., & Banerjee, J. (2023). RNA Sequencing of Intraoperative Peritumoral Tissues Reveals Potential Pathways Involved in Glioma-Related Seizures. Journal of molecular neuroscience : MN, 73(6), 437–447. https://doi.org/10.1007/s12031-023-02125-y
- Haque, A., Engel, J., Teichmann, S. A., & Lönnberg, T. (2017). A practical guide to single-cell RNA-sequencing for biomedical research and clinical applications. Genome medicine, 9(1), 75. https://doi.org/10.1186/s13073-017-0467-4
- Curry, R. N., Aiba, I., Meyer, J., Lozzi, B., Ko, Y., McDonald, M. F., Rosenbaum, A., Cervantes, A., Huang-Hobbs, E., Cocito, C., Greenfield, J. P., Jalali, A., Gavvala, J., Mohila, C., Serin Harmanci, A., Noebels, J., Rao, G., & Deneen, B. (2023). Glioma epileptiform activity and progression are driven by IGSF3-mediated potassium dysregulation. Neuron, 111(5), 682–695.e9. https://doi.org/10.1016/j.neuron.2023.01.013
- Taylor, K. R., Barron, T., Hui, A., Spitzer, A., Yalçin, B., Ivec, A. E., Geraghty, A. C., Hartmann, G. G., Arzt, M., Gillespie, S. M., Kim, Y. S., Maleki Jahan, S., Zhang, H., Shamardani, K., Su, M., Ni, L., Du, P. P., Woo, P. J., Silva-Torres, A., Venkatesh, H. S., … Monje, M. (2023). Glioma synapses recruit mechanisms of adaptive plasticity. Nature, 623(7986), 366–374. https://doi.org/10.1038/s41586-023-06678-1
- Friebel, E., Kapolou, K., Unger, S., Núñez, N. G., Utz, S., Rushing, E. J., Regli, L., Weller, M., Greter, M., Tugues, S., Neidert, M. C., & Becher, B. (2020). Single-Cell Mapping of Human Brain Cancer Reveals Tumor-Specific Instruction of Tissue-Invading Leukocytes. Cell, 181(7), 1626–1642.e20. https://doi.org/10.1016/j.cell.2020.04.055
- Sills, G. J., & Rogawski, M. A. (2020). Mechanisms of action of currently used antiseizure drugs. Neuropharmacology, 168, 107966. https://doi.org/10.1016/j.neuropharm.2020.107966
- Brodie, M. J., Mintzer, S., Pack, A. M., Gidal, B. E., Vecht, C. J., & Schmidt, D. (2013). Enzyme induction with antiepileptic drugs: cause for concern? Epilepsia, 54(1), 11–27. https://doi.org/10.1111/j.1528-1167.2012.03671.x
- Rossetti, A. O., Jeckelmann, S., Novy, J., Roth, P., Weller, M., & Stupp, R. (2014). Levetiracetam and pregabalin for antiepileptic monotherapy in patients with primary brain tumors. A phase II randomized study. Neuro-oncology, 16(4), 584–588. https://doi.org/10.1093/neuonc/not170
- Iuchi, T., Kuwabara, K., Matsumoto, M., Kawasaki, K., Hasegawa, Y., & Sakaida, T. (2015). Levetiracetam versus phenytoin for seizure prophylaxis during and early after craniotomy for brain tumours: a phase II prospective, randomised study. Journal of neurology, neurosurgery, and psychiatry, 86(10), 1158–1162. https://doi.org/10.1136/jnnp-2014-308584
- Witt, J. A., & Helmstaedter, C. (2013). Monitoring the cognitive effects of antiepileptic pharmacotherapy--approaching the individual patient. Epilepsy & behavior: E&B, 26(3), 450–456. https://doi.org/10.1016/j.yebeh.2012.09.015
- Climans, S. A., Brandes, A. A., Cairncross, J. G., Ding, K., Fay, M., Laperriere, N., Menten, J., Nishikawa, R., O'Callaghan, C. J., Perry, J. R., Phillips, C., Roa, W., Wick, W., Winch, C., & Mason, W. P. (2020). Temozolomide and seizure outcomes in a randomized clinical trial of elderly glioblastoma patients. Journal of neuro-oncology, 149(1), 65–71. https://doi.org/10.1007/s11060-020-03573-x
- Gill, B. J. A., Khan, F. A., Goldberg, A. R., Merricks, E. M., Wu, X., Sosunov, A. A., Sudhakar, T. D., Dovas, A., Lado, W., Michalak, A. J., Teoh, J. J., Liou, J. Y., Frankel, W. N., McKhann, G. M., Canoll, P., & Schevon, C. A. (2022). Single unit analysis and wide-field imaging reveal alterations in excitatory and inhibitory neurons in glioma. Brain: a journal of neurology, 145(10), 3666–3680. https://doi.org/10.1093/brain/awac168
- Ioannou, P., Foster, D. L., Sander, J. W., Dupont, S., Gil-Nagel, A., Drogon O'Flaherty, E., Alvarez-Baron, E., & Medjedovic, J. (2022). The burden of epilepsy and unmet need in people with focal seizures. Brain and behavior, 12(9), e2589. https://doi.org/10.1002/brb3.2589
- King, A. A., Seidel, K., Di, C., Leisenring, W. M., Perkins, S. M., Krull, K. R., Sklar, C. A., Green, D. M., Armstrong, G. T., Zeltzer, L. K., Wells, E., Stovall, M., Ullrich, N. J., Oeffinger, K. C., Robison, L. L., & Packer, R. J. (2017). Long-term neurologic health and psychosocial function of adult survivors of childhood medulloblastoma/PNET: a report from the Childhood Cancer Survivor Study. Neuro-oncology, 19(5), 689–698. https://doi.org/10.1093/neuonc/now242
