Every year, over half a million Americans suffering from osteoarthritis undergo pain-reducing arthroscopic surgery of the knee [1]. Surgeons clean out loose fragments of cartilage surrounding the knee joint in an attempt to reduce irritation. A majority of patients report significantly reduced pain after the surgery [2]. The only problem? So do most patients who only think they’ve had the procedure. In a 2002 study led by Dr. Bruce Moseley, arthritis patients received either traditional pain-reducing arthroscopic surgeries or a sham designed to mimic them [1]. In the sham surgery, patients were taken into the operating room and the normal incision was made. Then, instead of performing the usual cleaning, the physicians pretended to perform the procedure, complete with simulated sounds and mimed actions. Post-operative conditions, including pain medication and rehabilitation, were identical between groups. From the patient’s perspective, there was nothing to distinguish the sham from the real treatment. And researchers found that this wasn’t the only similarity. Patients receiving the sham surgery reported almost exactly the same reduction in pain as did those who had the real thing. Simply put, it seems that surgery may not have actually reduced the patients’ pain, but believing they had the treatment certainly did. This is an example of the placebo effect – the illusion of treatment having a very real impact.
Observations of the placebo effect
British physician John Haygarth first recorded the placebo effect in 1799. At the time, two metal rods called Perkin’s Tractors were used to treat inflammation and pain, supposedly as a result of their complex metal alloys. Haygarth compared these to simple wooden rods and found that both produced the same improvement, concluding that any benefit of Perkin’s Tractors was due to “mere imagination” [3]. Placebo controls did not play a major role in clinical trials until the 1960s. Since then, a wide range of studies have demonstrated just how effective placebo procedures or medications can be. Fake infections of hook worm have improved asthma symptoms [4]. Wounded soldiers given saline as a substitute for morphine report decreased pain [5]. Recently, some studies have demonstrated that patients with mild to moderate depression may achieve similar improvement with sugar pills as with antidepressants [6]. Studies have shown that subjects told that flavored tonic water is alcoholic become intoxicated solely from the placebo effect [7].
It’s not just a pill or procedure that produces this effect; there are other factors involved that further complicate things. For example, studies have shown that even the color of a pill plays a role in its perceived effects. A group from the Netherlands examined this very phenomenon in 1998, and reported that yellow pills seem to be especially effective as antidepressants, while red pills are better stimulants. Green pills are best for reducing anxiety and white, chalky tablets best sooth ulcers. Pills stamped with a brand name are more effective than the generic, even if they’re chemically identical. Additionally, taking a fake pill more times per day increases its efficacy [8]. And none of this has anything to do with what is inside the pills.
The placebo effect in modern medicine
So why, if placebos are so powerful, don’t we use them in place of traditional medicine? A large-scale analysis of placebo trials from researchers at the University of Copenhagen in 2001 explains just this. In each of the 130 trials they examined, some patients received a placebo, while another group received no treatment at all [9]. This served as an ideal testing ground for the true power of the placebo. Unfortunately for mind-over-matter proponents, researchers concluded that the placebo effect was present only when the outcome metric was continuous – an outcome measure reported on a sliding scale – and trial outcomes were subjectively reported. Both objective and subjective reports for binary outcomes – an outcome measure reported as one of two options – and objective reports for continuous outcomes, failed to produce significant results for the placebo groups [9]. This is why physicians will never prescribe a sugar pill to treat high blood pressure or a slow healing wound. When it comes to continuous, subjective responses like pain, however, placebos can do wonders. Acupuncture, for example, has been suggested to be no more effective than a placebo using sham needles that never pierce the skin [10]. Yet in 2011, this technique was used in China as an alternative to anesthesia for open-heart surgery. The patients who received acupuncture needed far lower doses of narcotics for pain and had shorter stays in the intensive care unit [11].
Insights from the unique pathology of Parkinson’s disease
Parkinson’s disease provides an especially interesting example of the placebo effect. Through a unique neurologic interaction it allows a glimpse into the placebo effect’s underlying mechanism. Parkinson’s is a neurodegenerative disease thought to be caused by the death of dopamine-producing cells in the midbrain. Without enough dopamine, a crucial neurotransmitter, a person’s movements become slow, shaky, and rigid. One treatment for the disease is to administer dopamine agonists, compounds that activate dopamine receptors without the neurotransmitter itself being present. These drugs serve as a sort of substitute for dopamine, duplicating its effect in the brain, and alleviating some of the symptoms of Parkinson’s. And unlike the other treatments mentioned so far, this one performs significantly better than a placebo [12]. A trial from St. Luke’s Medical center in 2000, however, claims that there still exists a significant placebo-associated improvement with Parkinson’s patients [13]. What’s astonishing about this placebo effect in particular is that it’s not just subjective patient reports that are affected. In a double-blind study, where knowledge of the subject’s treatment group is restricted to both subject and researcher, utilizing the UCLA disability scale instead of subjective patient reports, the placebo still performed nearly as well as the legitimate drug [14]. The authors, however, report limitations in the study, specifically that the negative side effects seen in experimental groups that may have limited their improvement – giving the placebo group an unfair advantage. Despite these limitations, placebos do produce some improvement in the objectively-measured physical symptoms of Parkinson’s. This seems to complicate the findings that placebos only matter in responses governed by subjects’ mind.
To understand the underlying cause of this phenomenon, researchers at the University of British Columbia used PET scans to image the brains of patients given dopamine agonists as well as those given a placebo [15]. The researchers utilized a radiolabelled molecule, (C11)-raclopride, that binds to the same receptors as dopamine. Because raclopride and dopamine compete to bind to the same receptor, higher concentrations of dopamine translate into less bound Raclopride. Thanks to its radioactive carbon molecule, raclopride can be observed with PET scans and used as a reverse measurement of dopamine concentration. Using this method, the researchers found that the placebos and real medication both caused an increase in synaptic dopamine concentration when compared to an untreated control group. They also found that this effect was consistent with the extent that patients reported their perceived symptom improvement. The study thus suggests that dopamine release seems to be somewhat variable and correlated with the individual strength of each placebo effect.
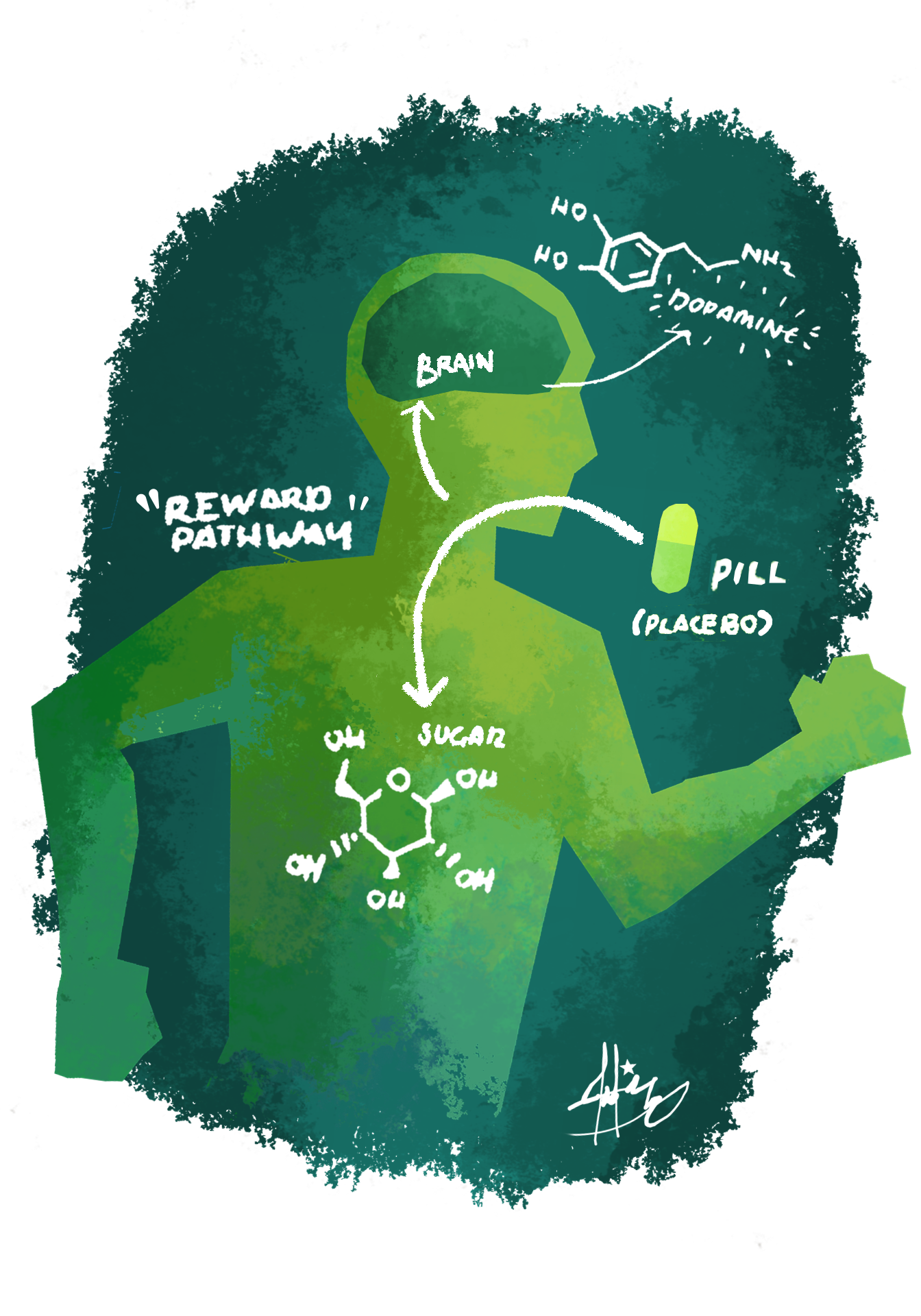
These measurements were carried out in the striatum, a region that is normally supplied with dopamine by the cells typically lost in Parkinson’s disease. [Call-out: Striatum: An interior portion of the forebrain involved in motivation and controlling movement that is supplied with dopamine from neurons in the substantia nigra. Because Parkinson’s disease is the result of cell death of dopamine producing neurons in the substantia nigra, the amount of dopamine provided to the striatum via the nigrostriatal pathway is reduced.] This means that the placebo effect caused the disease-damaged regions to pump out a closer to healthy flow of dopamine. The researchers concluded that “dopamine release in the nigrostriatal system is linked to expectation of a reward”– in this case, relief of the patient’s symptoms [15]. Parkinson’s Disease is a unique coincidence because the reward pathway activated by the placebo effect happens to affect the disease itself through this dopamine release. In doing so, Parkinson’s provides valuable insight into the inner workings of the placebo effect in general.
The mechanism behind this reward-expectation explanation of the placebo effect is the mesolimbic pathway, commonly known as the reward center [16]. The reward center is made up of the dopamine-producing cells of the midbrain and regions that they supply. One such area is the previously mentioned Striatum, a critical area in Parkinson’s disease. The midbrain also supplies dopamine to the frontal cortex - the outer layer of our brain that is directly responsible for what we think of as conscious thought. This “higher brain” also regulates lower functions, including pain responses and reflexes. When a placebo leaves us with the expectation of a reward, the midbrain releases dopamine to the frontal cortex, which gives rise to the conscious, subjective response that are typically associated with placebos. Studies supporting this theory have shown that late-stage Alzheimer’s patients, who tend to experience cortical degeneration, often show significantly weakened responses to placebos [17]. As a result they may find little improvement from medications with a large placebo component. Parkinson’s is a unique case because this same pathway produces objective, clinical improvement due to the pathology and anatomy of the dopamine-mediated disease [18].
The placebo effect: an emergent property
This reward model is a useful way to look at placebos, but it’s far from the complete picture. Pain, for example, is not regulated by dopamine, yet the placebo effect clearly influences pain processing as well. Therefore, a complete explanation of the placebo effect should involve the related pain pathways as well. In 2011 an Italian group made substantial progress towards this goal by identifying two different pain placebo pathways. By using drugs that block each pathway’s chief neurotransmitter (opioids and cannabinoids rather than dopamine) they were able to nullify the placebo effect’s impact on pain perception [19]. This indicates the presence of multiple pathways that differently mediate the placebo effect for pain and reward. But given the connections between pain relief and reward, it’s likely that these multiple pathways are often simultaneously active. There is also growing evidence that psychological phenomena like Pavlovian conditioning and anxiety responses may be involved with the placebo effect. Some researchers have even observed evidence of a genetic component [20].
The placebo effect could be categorized as an “emergent property”, meaning it only comes about as a result of many different pieces of the brain working together and cannot be fully attributed to one area. While our picture of the placebo effect is far from complete, some things are clear. The placebo effect is part psychology and part biology. It is powerful and far reaching, but also measurable and predictable. It is almost frightening how much control it can have over our conscious minds, yet it can also do immeasurable good by helping to treat some of today’s most devastating diseases. While we may not perfectly understand its mechanisms, the placebo effect is one of the most fascinating phenomena of science and medicine.
References
- Moseley, J., O'malley, K., Petersen, N., Menke, T., Brody, B., Kuykendall, D., . . . Wray, N. (2002). A Controlled Trial of Arthroscopic Surgery for Osteoarthritis of the Knee. New England Journal of Medicine N Engl J Med, 347(2), 81-88.
- Baumgaertner, M., Cannon, W., Vittori, J., Schmidt, E., & Maurer, R. (1990). Arthroscopic Debridement of the Arthritic Knee. Clinical Orthopaedics and Related Research, 253, 197-202.
- Booth, C. (2005). The rod of Aesculapios: John Haygarth (1740-1827) and Perkins' metallic tractors. Journal of Medical Biography, 13(3), 155-161.
- Feary, J., Venn, A., Mortimer, K., Brown, A., Hooi, D., Falcone, F., . . . Britton, J. (2010). Experimental hookworm infection: A randomized placebo-controlled trial in asthma. Clinical & Experimental Allergy, 40(2), 299-306.
- Beecher, H. (1955). The Powerful Placebo. JAMA Journal of the American Medical Association, 159(17), 1602-1602.
- Fournier, J., Derubeis, R., Hollon, S., Dimidjian, S., Amsterdam, J., Shelton, R., & Fawcett, J. (2010). Antidepressant Drug Effects and Depression Severity. JAMA, 303(1), 47-53.
- Assefi, S., & Garry, M. (2003). Absolut(R) Memory Distortions: Alcohol Placebos Influence the Misinformation Effect. Psychological Science, 14(1), 77-80.
- Craen, A., Roos, P., Vries, A., & Kleijnen, J. (1996). Effect of colour of drugs: Systematic review of perceived effect of drugs and of their effectiveness. Bmj, 313(7072), 1624-1626.
- Hrobjartsson, A., & Gøtzsche, P. (2001). Is the Placebo Powerless? An Analysis of Clinical Trials Comparing Placebo With no Treatment. Obstetrical and Gynecological Survey, 344(21), 628-629.
- Moffet, H. (2009). Sham Acupuncture May Be as Efficacious as True Acupuncture: A Systematic Review of Clinical Trials. The Journal of Alternative and Complementary Medicine, 15(3), 213-216.
- Zhou, J., Chi, H., Cheng, T., Chen, T., Wu, Y., Zhou, W., . . . Yuan, L. (2011). Acupuncture anesthesia for open heart surgery in contemporary China. International Journal of Cardiology, 150(1), 12-16.
- Pinter, M., Pogarell, O., & Oertel, W. (1999). Efficacy, safety, and tolerance of the non-ergoline dopamine agonist pramipexole in the treatment of advanced Parkinson's disease: A double blind, placebo controlled, randomised, multicentre study. Journal of Neurology, Neurosurgery & Psychiatry, 66(4), 436-441.
- Goetz, C., Leurgans, S., Raman, R., & Stebbins, G. (2000). Objective changes in motor function during placebo treatment in PD. Neurology, 54(3), 710-710.
- Diamond, S., Markham, C., & Treciokas, L. (1985). Double-blind trial of pergolide for Parkinson's disease. Neurology, 35(3), 291-291.
- Fuente-Fernandez, R. (2001). Expectation and Dopamine Release: Mechanism of the Placebo Effect in Parkinson's Disease. Science, 293(5532), 1164-1166.
- Benedetti, F., Mayberg, H., Wager, T., Stoler, C., & Zubieta, J. (2005). Neurobiological Mechanisms of the Placebo Effect. Journal of Neuroscience, 25(45), 10390-10402.
- Benedetti, F., Arduino, C., Costa, S., Vighetti, S., Tarenzi, L., Rainero, I., & Asteggiano, G. (2006). Loss of expectation-related mechanisms in Alzheimer’s disease makes analgesic therapies less effective. Pain, 121(1-2), 133-144.
- Kaasinen, V., Aalto, S., Nagren, K., & Rinne, J. (2004). Expectation of caffeine induces dopaminergic responses in humans. European Journal of Neuroscience Eur J Neurosci, 19(8), 2352-2356.
- Benedetti, F., Amanzio, M., Rosato, R., & Blanchard, C. (2011). Nonopioid placebo analgesia is mediated by CB1 cannabinoid receptors. Nature Medicine Nat Med, 17(10), 1228-1230.
- Furmark, T., Appel, L., Henningsson, S., Ahs, F., Faria, V., Linnman, C., . . . Fredrikson, M. (2008). A Link between Serotonin-Related Gene Polymorphisms, Amygdala Activity, and Placebo-Induced Relief from Social Anxiety. Journal of Neuroscience, 28(49), 13066-13074.